- male
- 45 Years
- 07/02/2025
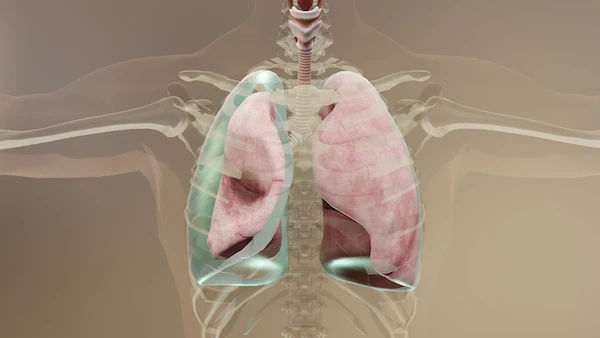
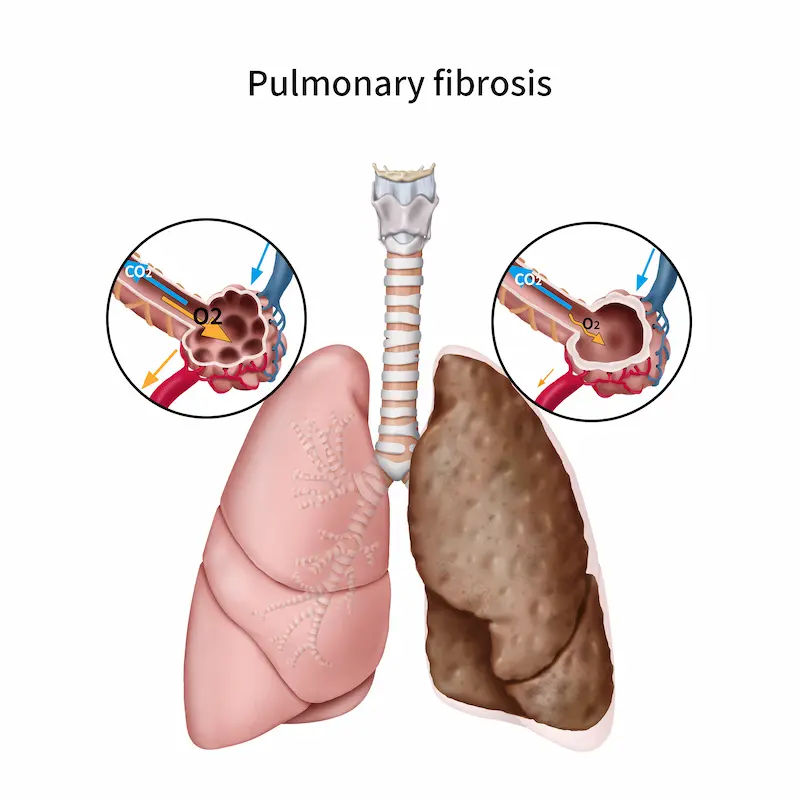
I was covid positive and just got a negative test result on May 22nd. My SR value was 16.44. I didnt really have any big issues, just a little fever and body pain. But now, even after a month, my oxygen levels have dropped from 98 to 94 and they're not going up. Should I be worried? What should I do?
More Pulmonology/ Respiratory Medicine Health Queries
View allIs it okay for a 17-year-old boy to use an asthalin inhaler? If I start using it, do I need to carry it everywhere I go? Could it actually lead to more breathing issues after using it? I checked online and found info saying the inhaler works for about 4-6 hours after taking two puffs. Does that mean the breathing problems will definitely return after those hours?
consult pulmonologist he will guide you about good inhalers that u have to take for only one or two times according to your requirements
read more![Doctor 1]()
![Doctor 2]()
Answered by 1 Apollo Doctors
I've been experiencing pain on the right side of my chest, and it seems to get worse when I laugh or cough. I'm a bit worried about what it could be, and I'm wondering if I should be taking any medication for it. Could you give me some advice on how to relieve it or if theres anything specific I should do?
zerodol MR for 3 days
read more![Doctor 1]()
![Doctor 2]()
Answered by 1 Apollo Doctors
I've been dealing with a persistent cough for what feels like ages, like over a thousand years, and it's been seriously frustrating. I've visited countless doctors, but none of the treatments seem to work for me. I'm constantly dealing with a dry cough and a sore throat, and it just keeps cycling back. Its leaving me feeling really stuck and I'm not sure what to do anymore. Got any ideas on what could help?
do salt gargling , take tablet amoxyclav for 5 days twice a day
read more![Doctor 1]()
![Doctor 2]()
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.