- male
- 60 Years
- 29/01/2025
I'm really worried about my father. He's had high blood pressure for about 20 days now. He's already a BP patient, but lately, his pressure is shooting up to around 16090. He was on promolate xl 25 before and now he's been switched to telvas 40 by the doctor. It doesn't seem to be helping control his blood pressure, though. Can you suggest anything that might help us manage this better?
Answered by 1 Apollo Doctors
It seems like your father's blood pressure is not well controlled with Telvas 40. In this case, the doctor may consider adding or adjusting the dosage of another medication. One common combination for high blood pressure is Telvas 40 (Telmisartan 40mg) along with Amlodipine (usually 5mg to 10mg). Amlodipine helps to further lower blood pressure by relaxing the blood vessels. However, the final decision on the medication and dosage should be made by your father's treating physician after a thorough evaluation. It is important to continue monitoring his blood pressure regularly and follow up with his doctor for further management.
Dr. Dr Khaleel Suggests...
Consult a Cardiologist
Answered 04/07/2025
0
0

More Cardiology Health Queries
View allI'm currently on Telma 40 for the past year, but my blood pressure still isnt under control. I'm also taking amlodac 5mg and Rosuvas 5mg, but I havent noticed much improvement. What can I do to get off these medications?
Continue all the medications..
Answered by 1 Apollo Doctors
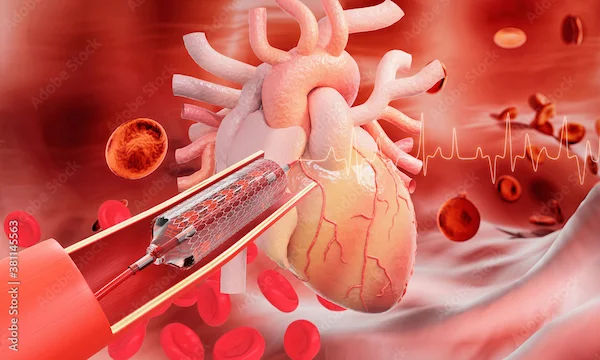
I'm trying to understand what mild bridging in the mid LAD means for my health. I know there aren't any blocks or holes, but are there specific problems I should be worried about because of this condition? What should I be looking out for, and does it affect my lifestyle in any way?
Mild bridging of the mid LAD (Left Anterior Descending) artery is a relatively common anatomical variant where the coronary artery tunnels through the myocardium instead of running on the surface of the heart. This can sometimes lead to compression of the artery during systole, potentially causing symptoms such as angina, arrhythmias, or even myocardial infarction in rare cases. However, in most cases, mild bridging of the mid LAD does not cause significant clinical issues and may not require any specific treatment. If you experience symptoms such as chest pain or shortness of breath, it is important to consult a healthcare professional for further evaluation and management.
Answered by 1 Apollo Doctors
I'm having some trouble with leg pain when I try to climb stairs, even just to the first floor. The pain seems to be worse in my calf muscle and I end up feeling really tired afterward. Is this something I should be worried about? Could it be a sign of a bigger issue, and what might help ease the pain?
-It sounds like you might be experiencing muscle fatigue or strain in your calf muscles when climbing stairs. This can happen if the muscles are overworked, especially if you're not used to the activity. Try resting, stretching, and strengthening your cal
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.


_3.webp)