- male
- 60 Years
- 14/08/2025
My doctor recommended bypass surgery but I'm unsure if it's really necessary - what are the alternatives or things I should consider before going ahead with this procedure
Answered by 1 Apollo Doctors
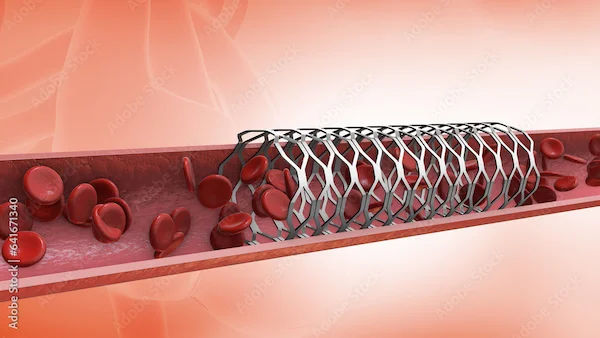
Before undergoing bypass surgery, consider alternatives like percutaneous coronary intervention (PCI) (angioplasty with stenting) and Enhanced External Counterpulsation (EECP). Discuss your concerns and explore all options with your doctor and heart care team to determine the most appropriate course of action.
Dr. Kamran Suggests...
Consult a Cardiologist
Answered 14/08/2025
0
0

More Cardiology Health Queries
View allI'm really worried about my father. He's been diagnosed with severe coronary ectasia and previously, doctors mentioned that a bypass surgery isn't an option for him. I'm wondering if treatments like Ace Inhibitors or the drug Entresto could be effective in his situation? Lately, he's been having more frequent chest pains and feeling a lot of unease. Could you provide some guidance on this?
For the treatment of coronary ectasia, Ace Inhibitors such as Lisinopril can be beneficial in managing symptoms and improving heart function. The recommended dosage of Lisinopril is usually starting at 2.5-5 mg once a day, which can be adjusted by the doctor based on individual response. Entresto, which is a combination of Sacubitril and Valsartan, can also be considered for the treatment of heart failure in patients with reduced ejection fraction. The usual starting dose of Entresto is 4951 mg twice daily, which can be increased to the target maintenance dose of 97103 mg twice daily as tolerated. However, it is important to consult with your father's healthcare provider before starting any new medication or making changes to his current treatment plan. Regular monitoring and follow-up with a healthcare professional are essential in managing coronary ectasia and associated symptoms.
Answered by 1 Apollo Doctors
I'm really concerned about my mom. She's got diabetes and high BP, and her recent echocardiography test had some results that are making me anxious. Her exercise duration was 9.51 minutes, and her max heart rate hit 152 bpm, which is 88% of the target heart rate of 172 bpm. Her max BP was 16680 mmHg, and she reached a max workload of 11.14 METS. The stress test came back positive for RMI. The doctors are suggesting an angiography test. I'm really worried. Is everything okay, or should I be more concerned?
Based on the results of the stress test showing a positive for reversible myocardial ischemia (RMI) and the recommendation for an angiography test, it indicates that there may be reduced blood flow to the heart muscle during physical activity. This could be a sign of underlying coronary artery disease. To address this issue, your mother may need to undergo angiography to further evaluate the blood flow in her coronary arteries. Depending on the findings of the angiography, the doctors will be able to determine the best course of treatment, which may include medications such as aspirin, statins, and beta-blockers to manage her condition and reduce the risk of complications. It is important to follow the advice of the medical professionals and proceed with the recommended tests and treatments to ensure the best possible outcome for your mother's heart health.
Answered by 1 Apollo Doctors
I recently went through a treadmill test (TMT) around mid-April, and just a few days after, I found out I had COVID. I got better by the end of April, but ever since, I've noticed that my heart races, especially when I'm doing things like climbing stairs. I went to a cardiologist, and both my ECG and echo tests looked fine, and he mentioned it might be anxiety. But, while my heartbeat is mostly normal now when I'm resting, I do notice a slight chest pain when I walk for more than 20-25 minutes. I'm curious, should I consider doing another TMT? And I'm really wondering, could having COVID possibly lead to plaque build-up in my arteries, even if the first TMT showed everything was fine? Any advice would be great.
It is unlikely that COVID infection would cause plaque in the arteries directly. However, COVID-19 can lead to inflammation in the body which may indirectly affect the heart and blood vessels. Since your previous TMT was fine, it may not be necessary to repeat it unless your symptoms worsen or persist. The chest pain you are experiencing while walking could be due to various reasons, including muscular pain or anxiety-related issues. To alleviate your symptoms, you can try medications like Ranitidine for acid reflux and Paracetamol for chest pain. If the symptoms persist, it is advisable to consult with your doctor for further evaluation and management.
Answered by 1 Apollo Doctors
Disclaimer: Answers on Apollo 247 are not intended to replace your doctor advice. Always seek help of a professional doctor in case of an medical emergency or ailment.

_2.webp)