Guide to Doctors Use Balloon Cryoablation Procedure To Treat Arrhythmia
Learn how doctors use balloon cryoablation to treat atrial fibrillation. Understand the procedure, who is eligible, risks, recovery, and how it compares with radiofrequency ablation.

Introduction
If you have been told you have atrial fibrillation (AF) or are experiencing stubborn heart palpitations, you may have heard your doctors mention balloon cryoablation. This minimally invasive procedure uses a small balloon to deliver cold energy inside the heart, freezing the areas that trigger abnormal rhythms. For many people, balloon cryoablation can reduce symptoms, improve quality of life, and decrease AF episodes, sometimes even as a first-line treatment.
In this guide, we explain balloon cryoablation in clear language. You will learn how the procedure works, who is most likely to benefit, its success rates and risks, how to prepare, and what recovery really feels like. We will compare cryoablation with radiofrequency heat-based ablation using real-world and clinical trial data and provide practical tips for choosing the right specialist and centre. If you are experiencing palpitations, shortness of breath, or fatigue, speak with a healthcare professional. If symptoms persist beyond two weeks or interfere with daily life, consult a doctor online
with Apollo 24|7 for further evaluation and guidance.
What Is Balloon Cryoablation?
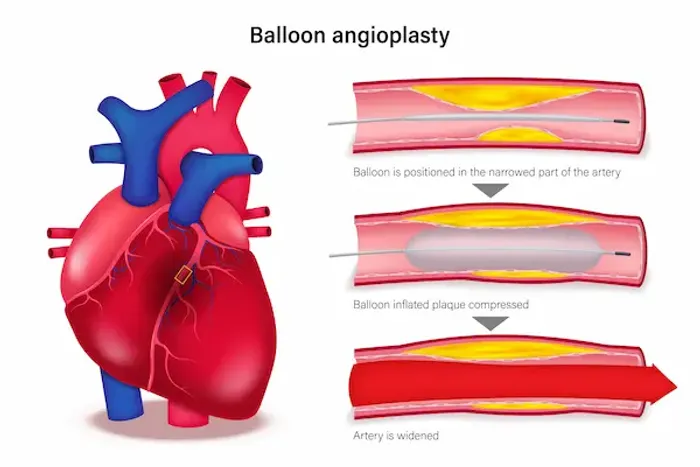
Balloon cryoablation is a type of catheter ablation used primarily to treat atrial fibrillation, the world’s most common heart rhythm disorder. Instead of burning heart tissue with heat, doctors guide a soft, compliant balloon into the left atrium and position it at the opening of each pulmonary vein, which carry oxygenated blood from the lungs to the heart. The balloon is inflated and cooled with a special refrigerant. This creates a circular freeze around the vein, electrically isolating it from the rest of the atrium. Many AF triggers originate within or near these veins, so isolating them, called pulmonary vein isolation, can stop atrial fibrillation from starting or sustaining itself.
The science of freezing is straightforward. Extreme cold temporarily stuns cells and, with sustained application, creates a lasting lesion by disrupting cell membranes and microcirculation. Unlike spot-by-spot radiofrequency lesions, the balloon’s circumferential contact can create a continuous ring of scar in a single application, reducing gaps. A mapping catheter confirms the veins are electrically isolated before the procedure ends.
While cryoballoon ablation is best known for AF, not every arrhythmia is suitable. Arrhythmias arising from focal points outside the pulmonary veins or requiring sculpted lesions, such as typical atrial flutter lines, complex atrial tachycardias, or ventricular arrhythmias, are often better treated with radiofrequency, pulsed field ablation, or hybrid strategies. Your electrophysiologist, a cardiologist specialising in heart rhythms, will recommend the best approach for your condition.
Two main points to remember: balloon cryoablation targets the source of many AF episodes through pulmonary vein isolation, and its freeze energy is as precise and controllable as heat. Whether it is right for you depends on your AF type, anatomy, and goals.
Consult Top Cardiologists
Who Should Consider It? Indications and Eligibility
Doctors consider balloon cryoablation for adults with symptomatic atrial fibrillation, especially paroxysmal AF, which starts and stops on its own. Evidence now supports ablation as a first-line therapy in many patients, not only after medications fail. The EARLY-AF randomised trial found that first-line cryoablation reduced AF recurrence and improved quality of life compared with antiarrhythmic drugs in patients with paroxysmal AF. Current professional guidelines endorse catheter ablation as a reasonable first-line option in selected patients with symptomatic paroxysmal AF, particularly when improving quality of life and reducing arrhythmia burden are priorities.
People with persistent AF, lasting more than seven days, can also benefit, though success rates may be lower and repeat procedures might be needed. Some electrophysiologists prefer radiofrequency or hybrid strategies for persistent AF because they allow tailored lesion patterns beyond pulmonary vein isolation. Cryoballoon ablation is used in many centres for persistent AF with good outcomes in selected patients.
Eligibility considerations include:
- Symptom burden and goals: If palpitations, fatigue, shortness of breath, or exercise intolerance affect your life despite
lifestyle changes or medications, you may be a candidate. - Heart structure and health: Echocardiogram or cardiac CT imaging helps assess left atrial size and pulmonary vein
anatomy to ensure the balloon can seal each vein effectively. Severe left atrial enlargement or complex anatomy may
influence the strategy. - Overall risk profile: Your team will review stroke risk, bleeding risk, sleep apnea, obesity, and other conditions. Treating
sleep apnea and weight management may improve success rates. - Contraindications: Active infection, uncontrolled bleeding, or inability to take anticoagulation around the procedure are
typical reasons to defer ablation. Certain rare anatomical variants may limit balloon use.
A unique perspective: the “right time” for ablation is earlier than many people realise. Trials like EARLY-AF show that
waiting for medications to fail is not always necessary. If you have had several documented AF episodes or are
avoiding activities you enjoy, ask your electrophysiologist whether first-line cryoablation could restore rhythm stability
sooner. If unsure, consult a cardiologist online via Apollo 24|7.
Benefits, Risks, and Real-World Outcomes
Balloon cryoablation offers meaningful benefits:
- Reduced AF recurrence and symptom burden: The FIRE AND ICE trial compared cryoballoon with radiofrequency
ablation in paroxysmal AF and found similar efficacy in preventing recurrent AF and avoiding repeat procedures and
hospitalisations. - First-line advantage over drugs: EARLY-AF demonstrated that first-line cryoballoon ablation led to lower arrhythmia
recurrence and improved quality of life than antiarrhythmic drugs. - Streamlined procedures: The balloon creates a circumferential lesion in a single application, potentially shortening
procedure time while achieving pulmonary vein isolation.
Risks include:
- Vascular access complications: Bruising, bleeding, or rarely, vessel damage at the groin.
- Stroke or transient ischaemic attack: Uncommon, minimised by careful anticoagulation.
- Phrenic nerve injury: Unique to right-sided pulmonary vein freezes. Phrenic nerve pacing during freezes helps detect
early changes. Most injuries improve over time. - Pulmonary vein stenosis: Rare with modern cryoballoons but remains a known risk.
- Other: Pericardial effusion, infection, or reaction to anaesthesia are rare but possible.
Success generally means fewer or no AF episodes, less reliance on medications, and better energy and exercise
tolerance. Some brief episodes can occur during the first three months, the “blanking period,” as the heart heals. A
recurrence after this period does not negate benefits; many patients still have dramatically fewer or milder episodes
overall.
Inside the Procedure: Before, During, and After
Preparation starts with a thorough review of symptoms and medications, including blood thinners. Many centres
continue anticoagulation through the procedure to minimise stroke risk. Blood tests, echocardiogram, and sometimes cardiac CT help map the pulmonary veins. Apollo 24|7 offers home collection for routine pre-procedure tests.
The day before, follow fasting instructions, review medication timing, and arrive as advised. Consent forms are signed,
and the team, including nurses and the electrophysiologist, will meet you. Bring a list of medications and allergies.
During the procedure, performed in an electrophysiology lab, you receive conscious sedation or general anaesthesia.
Catheters are advanced into the heart through a groin puncture. A transseptal puncture provides access to the left
atrium. The cryoballoon catheter is positioned at each pulmonary vein, with contrast dye confirming complete seal.
Freezing begins once positioning is confirmed. Phrenic nerve pacing protects the nerve during right-sided freezes. A
mapping catheter confirms electrical isolation.
After the procedure, you rest while the access site seals. Most patients go home the same day or after an overnight stay.
Mild chest discomfort, sore groin, or fatigue may last a few days. Desk work may resume in 2–5 days and exercise
within 1–2 weeks.
Red flags after discharge:
- Worsening chest pain or shortness of breath
- Fainting, one-sided weakness, trouble speaking, or severe headache
- Fever, chills, or groin site infection
- New or worsening swelling or bleeding at the access site
Seek urgent care if these occur. For non-urgent concerns like persistent palpitations beyond the blanking period,
schedule a follow-up. Consult a doctor online with Apollo 24|7 if you need help coordinating care.
Cryoballoon vs Radiofrequency: Which Is Better for You?
Cryoablation and radiofrequency (RF) ablation aim to achieve durable pulmonary vein isolation and symptom relief.
The FIRE AND ICE trial showed that, in paroxysmal AF, cryoballoon and RF had similar efficacy for preventing
arrhythmia recurrence and comparable safety profiles. Some secondary outcomes, such as repeat procedures and
quality-of-life measures, favoured cryo in certain analyses. Both options are excellent when performed by experienced
teams.
Potential advantages of cryoballoon:
- Workflow efficiency: Circumferential lesion creation in one application per vein.
- Comparable outcomes: Similar arrhythmia freedom to RF in paroxysmal AF.
Potential advantages of RF:
- Lesion flexibility: Tailored, point-by-point lesions beyond PV isolation.
- Evolving technology: High-power, short-duration RF and novel energy sources such as pulsed field ablation.
Doctors choose based on AF type, atrial anatomy, need for non-PV lesions, centre expertise, technology availability,
and patient preferences about anaesthesia and procedure time.
Recovery, Recurrence, and Long-Term Care
Recovery usually progresses quickly. Mild chest tightness is common for a few days. Light activity is encouraged. The
first 90 days are the “blanking period,” when short, self-limited arrhythmias may occur. Antiarrhythmic medication
may be used temporarily during this period.
Anticoagulation remains critical. Most patients continue blood thinners for several months. Long-term use depends on
stroke risk rather than procedural success.
Lifestyle factors that improve outcomes:
- Treat sleep apnea
- Weight management and exercise
- Alcohol and stimulant moderation
- Blood pressure and diabetes control
Monitoring at home can include wearable ECG patches or consumer devices. If AF recurs beyond the blanking period,
follow up with your doctor. Some patients may need a redo ablation if a vein reconnects.
Recovery is a partnership. Daily choices—sleep, stress, exercise, and medications—help stabilise heart rhythm. Consult
a doctor with Apollo 24|7 if improvements do not occur.
Finding the Right Doctor and Centre
Choosing an experienced electrophysiologist and centre is crucial. Consider:
- Experience and volume: Ask about annual cryoablation numbers.
- Technology and capabilities: Availability of cryoablation, RF, advanced imaging, phrenic nerve monitoring.
- Outcomes transparency: Complication rates, same-day discharge rates, redo rates.
- Team access: Communication, telehealth for pre- and post-procedure visits.
Questions to ask your electrophysiologist:
- Am I a good candidate for cryoballoon ablation?
- What are the alternatives, and how do outcomes compare?
- What anaesthesia will be used and how long is the lab time?
- What if a vein does not isolate?
- How will recurrence be monitored?
Costs and insurance: Coverage is common for symptomatic AF when medically indicated. Preauthorisation is typical.
Ask about out-of-pocket costs, hospital vs professional fees, and device-related costs. Telehealth can help coordinate
care.
Conclusion
Balloon cryoablation provides a clear, evidence-backed path to fewer AF episodes, better energy, and improved quality of life. By creating a controlled freeze around each pulmonary vein, doctors can disconnect the most common electrical triggers of atrial fibrillation. Clinical trials show cryoballoon ablation performs on par with radiofrequency ablation for paroxysmal AF and often outperforms medications when used first-line.
Best results come from partnership: a skilled electrophysiologist, a centre with the right tools, and your commitment to recovery, lifestyle adjustments, and follow-up. If you experience persistent palpitations, shortness of breath, or fatigue, or if medications have not relieved your symptoms, ask whether balloon cryoablation could be an option. Consult a doctor online with Apollo 24|7 to discuss your symptoms, arrange testing with home lab collection, and plan referral to an experienced electrophysiology team. Taking the next step could help restore your rhythm and improve quality of life.
Consult Top Cardiologists
Consult Top Cardiologists

Dr. Syed Akram Ali
Cardiologist
14 Years • MBBS DCH DNB(PED) DNB(CARD) CONSULTANT INTERVENTOINAL CARDIOLOGIST, EUROPEAN SOCIETY OF CARDIOLOGY CERTIFIED HEART FAILURE SPECIALIST
Hyderabad
AYMAN POLYCLINIC, Hyderabad

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sumanta Chatterjee
Cardiologist
12 Years • MBBS,MD General Medicine,DM Cardiology
Kolkata
HealthYou Speciality Clinic & Diagnostics., Kolkata
(25+ Patients)
Dr. Sibashankar Kar
Cardiologist
10 Years • MBBS, DNB
Bhubaneswar
Hi-Tech Medical College & Hospital, Bhubaneswar
Consult Top Cardiologists

Dr. Syed Akram Ali
Cardiologist
14 Years • MBBS DCH DNB(PED) DNB(CARD) CONSULTANT INTERVENTOINAL CARDIOLOGIST, EUROPEAN SOCIETY OF CARDIOLOGY CERTIFIED HEART FAILURE SPECIALIST
Hyderabad
AYMAN POLYCLINIC, Hyderabad

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sumanta Chatterjee
Cardiologist
12 Years • MBBS,MD General Medicine,DM Cardiology
Kolkata
HealthYou Speciality Clinic & Diagnostics., Kolkata
(25+ Patients)
Dr. Sibashankar Kar
Cardiologist
10 Years • MBBS, DNB
Bhubaneswar
Hi-Tech Medical College & Hospital, Bhubaneswar
More articles from Arrhythmia
Frequently Asked Questions
Q1. What is the success rate of cryoballoon ablation for atrial fibrillation?
For paroxysmal AF, studies show cryoballoon ablation achieves freedom from recurrent arrhythmia comparable to radiofrequency ablation and superior to antiarrhythmic drugs in first-line settings, with meaningful symptom and quality-of-life gains.
Q2. How long is recovery after balloon cryoablation?
Most people resume light activities within a few days and normal routines in one to two weeks. The first 90 days are a “blanking period,” when short, self-limited episodes can occur as the heart heals.
Q3. Is cryoablation safer than radiofrequency ablation?
Overall safety is similar. Cryoablation has a unique but uncommon risk of phrenic nerve injury, while both share rare risks such as stroke or vascular complications. Experienced teams mitigate these risks with careful protocols.
Q4. Do I still need blood thinners after cryoballoon ablation?
Usually yes, at least for several months. Long-term anticoagulation depends on your stroke risk (CHA2DS2-VASc score), not solely on procedural success. Always follow your doctor’s advice.
Q5. Who is a good candidate for first-line cryoballoon ablation?
Adults with symptomatic paroxysmal AF who want to reduce episodes and improve quality of life may be good candidates, as supported by the EARLY-AF trial and recent guidelines. Discuss this with your electrophysiologist or consult a doctor online with Apollo 24|7.




.webp)