How Does a Tumour Develop? A Step-by-Step Guide to Cancer Growth
Know about the tumour development, comparison of benign and malignant, role of DNA, multi-step process for tumour development, angiogenesis, metastasis and more.

Written by Dr. Siri Nallapu
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
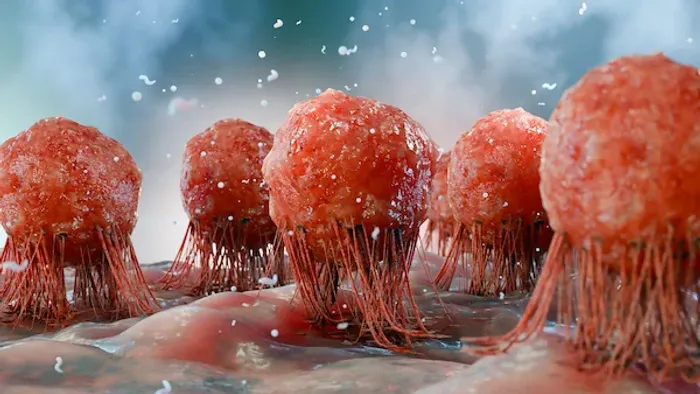
Finding a lump or hearing the word "tumour" can be frightening. But knowledge is power. Understanding how a tumour develops demystifies the process and highlights the importance of prevention and early detection. At its core, cancer is a disease of uncontrolled cell growth. Our bodies are made of trillions of cells that normally divide, mature, and die in an orderly way to keep us healthy. A tumour begins when this precise system goes awry. This article will serve as your clear, step-by-step guide to the fascinating and complex journey of how a single cell can transform into a tumour. We'll break down the science behind DNA mutations, explain how tumours build their own blood supply to grow, and distinguish between benign and malignant growths.
What is a Tumour? Benign vs. Malignant
Simply put, a tumour, or a neoplasm, is a mass of tissue that forms when cells divide and grow excessively. Not all tumours are cancerous. The critical distinction lies in their behaviour, which determines whether they are benign or malignant.
Consult a Top Oncologist for Personalised Advice
Understanding Benign Tumours
Benign tumours are the less dangerous cousins in the world of abnormal growth. They are characterised by:
Localised Growth: They grow slowly and remain confined to their original location. They do not invade surrounding tissues.
Encapsulation: They are often surrounded by a fibrous capsule that separates them from normal tissue.
Non-Cancerous: They are not considered cancer. Once removed, they typically do not grow back.
While usually harmless, a benign tumour can cause problems if it grows large enough to press on vital organs, nerves, or blood vessels. For example, a benign brain tumour can be serious due to the pressure it exerts within the confined space of the skull.
Understanding Malignant Tumours (Cancer)
Malignant tumours are what we commonly refer to as cancer. Their hallmarks are invasion and spread, making them potentially life-threatening.
Invasive Growth: Malignant cells can invade and destroy adjacent healthy tissues.
Metastasis: This is the most dangerous characteristic. Cancer cells can break away from the primary tumour, travel through the bloodstream or lymphatic system, and form new tumours (metastases) in other parts of the body.
The difference between benign and malignant tumour behaviour is the foundation of understanding cancer severity.
The Spark: How DNA Damage Starts a Tumour
The journey of how a tumour develops begins deep within our cells, in the DNA. DNA acts as the cell's instruction manual, containing genes that tell the cell how to function, when to divide, and when to die. Cancer is ultimately caused by mutations—typos or damage—to this instruction manual.
These mutations can be inherited or, more commonly, acquired during a person's life due to environmental factors like smoking, UV radiation, or simply random errors during normal cell division. The process of carcinogenesis (cancer formation) often involves mutations in two key types of genes:
Oncogenes: The Accelerator Pedal
Think of oncogenes as the accelerator pedal for cell growth. In their normal state (proto-oncogenes), they help cells divide when necessary. However, when a mutation permanently "jams" the accelerator pedal down, it signals the cell to divide uncontrollably, even when it shouldn't.
Tumour Suppressor Genes: The Brakes
If oncogenes are the accelerator, tumour suppressor genes are the brakes. They slow down cell division, repair DNA mistakes, and tell cells when it's time to die (a process called apoptosis). When these genes are mutated and disabled, the brakes fail. The cell loses its ability to control its growth and cannot fix genetic errors, allowing mutations to accumulate. A well-known example is the BRCA gene, which, when mutated, increases the risk of breast and ovarian cancer.
The Multi-Step Process of Tumour Development
Cancer rarely results from a single mutation. Instead, it's a multi-stage process where a cell accumulates a series of genetic hits over time. This explains why cancer risk increases with age.
Step 1: Initiation – The First Genetic Hit
Initiation is the first step where an external carcinogen (like tobacco smoke) or an internal error causes irreversible damage to a cell's DNA. This initial mutation might affect a proto-oncogene or a tumour suppressor gene. At this stage, the cell is damaged but not yet cancerous. It may lie dormant for years.
Step 2: Promotion – Building a Critical Mass
Promotion involves agents (promoters) that encourage the initiated cell to divide and multiply. Promoters themselves don't cause cancer but stimulate the growth of the already-initiated cell. This can include factors like hormones, chronic inflammation, or alcohol. During this phase, the cluster of mutated cells, now a microscopic tumour, continues to accumulate more mutations.
Step 3: Progression – Becoming Aggressive and Invasive
Progression is the final stage where the tumour becomes truly malignant. The cells become more genetically unstable and aggressive. They develop new mutations that allow them to invade nearby tissues. This is also when they gain the ability to metastasise. The tumour is now a complex ecosystem of diverse cells, some of which have the special skills needed to spread.
Fueling the Fire: How Tumours Create Their Own Blood Supply (Angiogenesis)
A tiny tumour can only grow to about the size of a pinhead (1-2 millimetres) without a dedicated blood supply. To grow larger, it needs oxygen and nutrients. This is where angiogenesis, the formation of new blood vessels, becomes critical.
Tumours are clever; they secrete special signals called angiogenic factors (e.g., VEGF - Vascular Endothelial Growth Factor). These factors trick the body into building a network of new blood vessels that directly feed the tumour, a process often called "tumour angiogenesis." This supply line allows the tumour growth to accelerate rapidly, enabling it to become a much larger, macroscopic mass. Drugs that block angiogenesis (antiangiogenic therapy) are an important part of modern cancer treatment, essentially starving the tumour.
The Dangerous Journey: How Cancer Spreads (Metastasis)
Metastasis is the primary cause of death from cancer. The process of cancer metastasis is a complex, inefficient journey that only a small number of cancer cells can complete. It involves several steps:
1. Invasion: Cancer cells break through the basement membrane (a barrier separating tissues) and invade nearby normal tissues.
2. Intravasion: The cells enter the bloodstream or lymphatic system.
3. Circulation: The cells travel through the body.
4. Arrest & Extravasion: The cells get stuck in small vessels of a distant organ and exit into the new tissue.
5. Colonisation: The most difficult step. The cells must adapt to the new environment, multiply, and trigger angiogenesis to form a new, metastatic tumour.
6, Common sites for metastasis include the lungs, liver, bones, and brain.
Common Risk Factors for Tumour Development
Understanding risk factors empowers prevention. While not everyone exposed will develop cancer, these factors increase the statistical probability.
Lifestyle Factors You Can Influence
Tobacco Use: The single largest preventable cause of cancer worldwide.
Diet: Diets high in processed meats, saturated fats, and low in fruits and vegetables are linked to a higher risk.
Alcohol: Excessive consumption is a risk factor for several cancers.
Physical Inactivity & Obesity: Linked to an increased risk of cancers like breast, colon, and endometrial.
Environmental and Occupational Exposures
UV Radiation: From the sun and tanning beds causes skin cancer.
Ionising Radiation: From radon gas, medical imaging (high doses), etc.
Carcinogens: Like asbestos (mesothelioma), benzene (leukaemia), and certain industrial chemicals.
Genetic Predisposition and Family History
Inherited mutations, such as in the BRCA1/2 genes, significantly increase risk. However, it's important to remember that only about 5-10% of all cancers are strongly hereditary.
Conclusion
Understanding how a tumour develops reveals cancer not as a single event, but as a complex, multi-stage process that often unfolds over years. This underscores the tremendous importance of lifestyle choices in prevention and the critical value of early detection through recommended screenings. While biology can seem daunting, this knowledge highlights that our bodies have powerful built-in safeguards, and modern medicine continues to develop targeted strategies to interrupt this process at various stages. If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation. They can assess your risk factors, recommend appropriate screenings like mammograms or colonoscopies, and provide peace of mind or a clear path forward. For necessary diagnostic tests, Apollo24|7 offers convenient home collection services.
Consult a Top Oncologist for Personalised Advice
Consult a Top Oncologist for Personalised Advice

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Praveen Kumar Garg
Surgical Oncologist
26 Years • MBBS, M.S.(Gen.Surg.), M.Ch.(OncoSurg.)
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr. Gopal Kumar
Head, Neck and Thyroid Cancer Surgeon
15 Years • MBBS, MS , FARHNS ( Seoul, South Korea ), FGOLF ( MSKCC, New York )
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Raja T
Oncologist
20 Years • MBBS; MD; DM
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)

Dr. Harsh J Shah
Surgical Oncologist
15 Years • MS, MCh (GI), DrNB (GI)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad