Guide to Cardiac Sciences Cardiac Surgery Ctvs/what Bypass Surgery
Learn what Coronary Artery Bypass Grafting (CABG) surgery is, how it works to restore blood flow to the heart, who needs it, and what to expect during recovery.

Written by Dr. Siri Nallapu
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 14th Jan, 2026

Introduction
Heart bypass surgery—formally called coronary artery bypass grafting or CABG—is one of the most common and effective cardiac surgeries performed worldwide. If you or a loved one has been told a bypass might be needed, it’s normal to have questions: What exactly happens in this operation? How is it different from stents? What are the risks, the recovery, and the results you can expect? In this practical guide from a cardiac sciences perspective, we’ll explain bypass surgery in plain language, including who needs it, how surgeons in CTVS (cardiothoracic and vascular surgery) teams perform it, and how to recover confidently.
You’ll learn when CABG is favored over angioplasty, how grafts like the left internal mammary artery (LIMA) improve blood flow, and what the hospital-to-home journey looks like. We’ll discuss medicines, diet, exercise, and long-term outcomes—plus how to choose the right center, estimate costs, and spot warning signs. Whether you’re preparing for surgery or comparing options, this evidence-based overview will help you make informed decisions and partner effectively with your care team.
Understanding Cardiac Bypass Surgery (CABG)
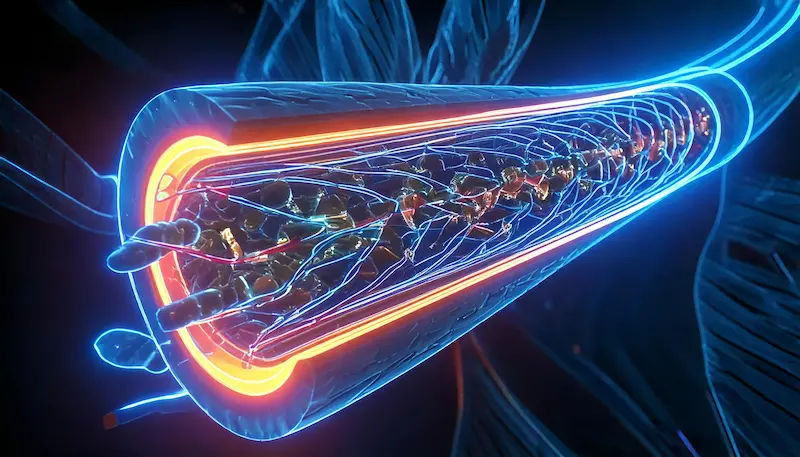
Bypass surgery aims to restore blood supply to heart muscle when coronary arteries are narrowed or blocked by
atherosclerosis (plaque). Surgeons create a “detour” around blockages using blood vessels (grafts) taken from your chest, arm, or leg. The most commonly used and durable arterial graft is the left internal mammary artery (LIMA), typically connected to the left anterior descending artery (LAD), the heart’s main supply route. This rerouting relieves angina, reduces heart attack risk, and can improve survival in select patients.
Cardiac sciences teams use CABG for people whose disease is too diffuse or complex for stents, or where evidence shows bypass provides better long-term outcomes—particularly in left main disease, triple-vessel disease, or diabetes. A seasoned CTVS team includes cardiac surgeons, cardiac anesthesiologists, perfusionists (heart-lung machine specialists), intensivists, cardiologists, specialized nurses, and rehabilitation experts. This multidisciplinary approach is central to safety, comfort, and recovery.
A simple way to think about it: blocked pipes starve your home of water; new piping around the blockage restores flow. In the heart, restoring flow means less chest pain, more exercise capacity, and fewer future emergencies. One unique insight from modern practice is the emphasis on complete revascularization—strategically bypassing all major critical narrowings—to improve durability and reduce the need for repeat procedures. Guidelines increasingly highlight this goal when feasible.
Who Needs Bypass Surgery—and When?
Your care team considers bypass when symptoms and tests point to significant, functionally important blockages.
Typical warning signs include exertional chest pain or pressure, shortness of breath, reduced exercise tolerance, or a
recent heart attack. Diagnosis involves a mix of tests: ECG, echocardiogram, stress tests, and, when needed, coronary angiography to map blockages. Advanced assessments like fractional flow reserve (FFR) or intravascular imaging may refine decisions.
Indications favoring CABG over stents (PCI) or medicines alone often include:
- Left main coronary disease or complex triple-vessel disease (especially high SYNTAX scores)
- Diabetes with multivessel disease, where CABG has shown better long-term outcomes than PCI in large trials and
guidelines - Diffuse disease where stents would be too numerous or less durable
- Prior stents with recurrent restenosis
- Concomitant valve disease needing surgical repair or replacement
Pre-surgery tests commonly include labs (blood count, kidney function, HbA1c), chest X-ray, carotid ultrasound if
stroke risk is suspected, and vein mapping for graft planning. If you’re arranging tests, Apollo 24|7 offers convenient home collections for labs such as lipid profile, HbA1c, and kidney function to support preoperative optimization. If your symptoms persist beyond two weeks or worsen, consult a doctor online with Apollo 24|7 for further evaluation.
Unique perspective: Decision-making should be shared. Ask your cardiologist and surgeon to walk you through heart team deliberations and show your angiogram images. Understanding your SYNTAX score (disease complexity) and patient factors (age, diabetes, kidney function) helps align choices with your goals.
How CABG Works: Techniques, Grafts, and the Operation Day
Graft choices matter. Arterial grafts (LIMA, right internal mammary artery, radial artery from the forearm) tend to last
longer than saphenous vein grafts from the leg. LIMA-to-LAD grafts show excellent patency, with about 90% remaining open at 10 years in many series, while saphenous vein graft patency is lower, prompting aggressive risk-factor control post-op. Your surgeon may recommend multiple arterial grafts depending on age, anatomy, and risk.
Techniques:
- On-pump CABG uses a heart-lung machine to circulate blood while the heart is still. It allows a quiet, bloodless field for
precise suturing. - Off-pump CABG is performed on a beating heart using stabilizers, potentially reducing certain complications in select
patients, though outcomes depend heavily on surgeon experience. - Minimally invasive or robotic CABG can be offered for suitable single-vessel (often LAD) disease or hybrid procedures
combining a surgical LIMA-LAD graft with stents elsewhere. These approaches use smaller incisions and may speed
recovery, but availability varies by center.
Operation day, step-by-step:
- Anesthesia and monitoring lines are placed.
- Incisions: a midline sternotomy (most common) or smaller side incision for minimally invasive cases.
- Grafts are harvested from the chest, arm, or leg.
- Bypasses are sewn around blockages, restoring downstream flow.
- The heart is restarted (if on-pump), the chest is closed with sternal wires, and you’re transferred to the ICU.
Unique insight: The strategy is customized—surgeons aim not just to add grafts but to maximize long-term benefit by prioritizing critical territories (like LAD) with the best graft (LIMA) and ensuring complete revascularization when safe. Ask if radial artery grafting is appropriate for you.
Consult a Top Orthopaedics
Risks, Recovery, and Rehabilitation
CABG is a major cardiac surgery, but for appropriate candidates, benefits typically outweigh risks. Potential complications include bleeding, infection (including sternal wound infection), atrial fibrillation (common and usually transient), kidney injury, stroke, heart attack, lung complications, and, rarely, death. In contemporary practice, operative mortality for elective, lower-risk patients is often in the 1–2% range, higher in urgent/high-risk groups. Your personal risk is estimated using tools like the STS risk score.
Recovery timeline:
- ICU and hospital: Most patients are extubated within hours and transition to the ward in 1–2 days. Hospital stay is
typically 5–7 days, depending on recovery and comorbidities. - At home: Expect fatigue and incision soreness for a few weeks. Walking daily, breathing exercises, and sternal
precautions (avoid heavy lifting, brace your chest when coughing) help healing. - Cardiac rehab: Supervised rehabilitation improves fitness, confidence, and outcomes. It usually starts within weeks of
discharge and continues for 6–12 weeks, tailored to your capacity.
Return to activities:
- Driving: Often after 4–6 weeks if cleared.
- Work: Desk jobs in 6–8 weeks; more strenuous roles may take longer.
- Exercise: Gradual progression from walking to moderate aerobic activity; resistance training is added under guidance.
Unique perspective: Track your progress with simple metrics—daily steps, a 6-minute walk distance, or heart rate recovery. Set small, achievable goals. If you notice new chest pain, breathlessness, fever, wound redness, or leg swelling, seek medical advice promptly. If your condition does not improve after following recovery guidance, book a physical visit to a doctor with Apollo 24|7.
Living Well After Surgery
Medicines after CABG:
- Antiplatelet therapy (aspirin; sometimes dual therapy with clopidogrel/other agents after acute coronary syndrome)
helps keep grafts open. - High-intensity statins lower LDL cholesterol, stabilizing plaque and improving graft outcomes. Many guidelines
recommend LDL targets below 55–70 mg/dL for very high-risk patients. - Beta-blockers, ACE inhibitors/ARBs, and SGLT2 inhibitors (in diabetics or those with heart failure) may be prescribed
based on your profile.
Lifestyle pillars:
- Nutrition: Emphasize vegetables, fruits, whole grains, legumes, nuts, olive oil, and lean proteins; limit sodium, added
sugars, and processed meats. A Mediterranean-style pattern is heart-friendly. - Exercise: Aim for 150 minutes/week of moderate activity plus resistance training; cardiac rehab helps you get there
safely. - Sleep and stress: Sleep 7–9 hours; consider mindfulness, yoga, or cognitive behavioral strategies for anxiety or mood
changes common after major surgery. - Smoking cessation: Absolute priority—quitting dramatically improves survival and graft patency.
Long-term outcomes:
- Many patients enjoy better quality of life, fewer angina episodes, and improved survival in the right indications. LIMA-
LAD grafts deliver durable benefit, while vein grafts need vigilant risk-factor control. - Regular follow-up includes clinical review and, when symptoms change, stress testing or imaging.
Unique insight: Think “arteries plus habits.” Arterial grafts give you a durable mechanical fix; lifestyle and medication provide the biologic protection that keeps all arteries—native and grafted—healthy for the long run.
Making the Decision: Choosing Your Cardiac Sciences Center
What to look for?:
- Experience and volume: Centers and surgeons with higher CABG volumes tend to have better outcomes; ask for their
annual case numbers and outcomes relative to benchmarks. - Multidisciplinary heart team: Cardiologists, surgeons, anesthesiologists, imaging specialists, and rehab staff
collaborating on your case. - Options suite: Availability of arterial grafting expertise, off-pump, minimally invasive/robotic CABG, and hybrid
revascularization. - Quality and safety metrics: STS/registry participation, infection rates, readmission rates, and patient satisfaction.
Costs and insurance:
- Costs vary by country, hospital type, room category, length of stay, and complexity (number of grafts, complications).
Ask for a detailed estimate covering surgeon/anesthesia fees, ICU, implants, tests, and rehab. - Check insurance coverage for surgery and cardiac rehab. Clarify out-of-pocket costs and cashless options.
Questions to ask:
- Why CABG vs stents or medicines in my case?
- How many similar surgeries have you done this year?
- What grafts will you use? Will I receive a LIMA-to-LAD graft?
- What is my personalized risk and recovery plan?
- How will we manage my diabetes/kidney disease if present?
Unique perspective: Consider a second opinion if recommendations vary. Different centers may offer minimally invasive approaches or hybrid options that fit your goals and anatomy.
Myths vs Facts About Bypass Surgery
- Myth: “Stents are always better because they’re less invasive.”
- Fact: For complex multivessel disease, left main disease, or diabetes, CABG often yields better long-term outcomes and
fewer repeat procedures. - Myth: “All grafts fail quickly.”
- Fact: Arterial grafts like LIMA can remain open for decades; lifestyle and medicines improve results.
- Myth: “You can’t be active after heart surgery.”
- Fact: Most people return to regular exercise with cardiac rehab and medical clearance, often with better stamina than
before. - Myth: “CABG cures heart disease forever.”
- Fact: It bypasses existing blockages; without risk-factor control, new disease can develop.
When to Seek Medical Help?
Pre-op red flags:
- Worsening chest pain, shortness of breath at rest, fainting, or signs of a heart attack warrant urgent care.
- New swelling, sudden weight gain, or palpitations should be reported.
Post-op warning signs:
- Fever, chills, wound redness or drainage, chest pain not relieved by rest, new shortness of breath, leg swelling/redness
(clot risk), or confusion require prompt attention. - If symptoms persist beyond two weeks after discharge, consult a doctor online with Apollo 24|7 for further evaluation
or arrange a physical visit as advised.
Conclusion
Bypass surgery is a cornerstone of cardiac sciences, offering durable relief from angina and improving long-term outcomes for many people with complex coronary artery disease. Understanding the “why” and “how” empowers you to make confident decisions: CABG is generally favored in left main and multivessel disease, particularly in diabetes, and when complete revascularization is feasible. Modern CTVS teams tailor the approach—graft selection, on- vs off-pump, and minimally invasive options—to your anatomy and goals.
Recovery is a journey, not a sprint. With structured cardiac rehabilitation, evidence-based medicines, and heart-healthy habits, most patients return to active lives—often with more energy than before. Your choices after surgery—regular follow-ups, LDL control, blood pressure and sugar management, exercise, and smoking cessation—are as important as the operation itself for long-term success.
If you’re considering surgery, ask about center and surgeon experience, graft strategy (including LIMA and radial artery use), and your personalized risk and recovery plan. If you have ongoing symptoms or new concerns, consult a doctor online with Apollo 24|7 or book an in-person visit for timely support. For pre-op optimization and follow-up, Apollo 24|7 offers a convenient home collection for labs like lipid profile and HbA1c. With the right information and a strong care team, you can navigate bypass surgery with clarity and confidence.
Consult a Top Orthopaedics
Consult a Top Orthopaedics

Dr. Naveen Palla
Orthopaedician
18 Years • MS
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila
(75+ Patients)

Dr. B. Harsha Vardhana Reddy
Orthopaedician
10 Years • "#MBA (Hospital Administration) – ICFAI University – 2021 #DNB (Orthopaedics) – Continental Hospital, Hyderabad – 2020 #Fellowship in Arthroscopy – Continental Hospital, Hyderabad – 2018 #Fellowship in Arthroplasty – Continental Hospital, Hyderabad – 2017 #D.Ortho – Dr. G.S. Kulkarni Orthopaedic Institute, Miraj (MUHS) – 2015 #MBBS – K.V.G Medical College, Bangalore (RGUHS) – 2012"
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr. Prashanth Reddy A
Orthopaedician
13 Years • "2006-2012 MBBS CHALMEDA ANAND RAO INSTITUTE OF MEDICAL SCIENCES -KARIMNAGAR,TELANGANA 2013- 2016 DNB Ortho Care Hospitals - Banjara Hills,Hyderabad 2018-2021 M.Ch (Hip & knee) EDGEHILL UNIVERSITY-WRIGHTINGTON HOSPITAL - WRIGHTINGTON,UK"
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr. Surendra Yellapu
Orthopaedician
8 Years • MBBS: Konaseema Inst. of Medical Sciences & Research Foundation in Amalapuram, Andhra Pradesh, 2013 • MS: Orthopaedics in Alluri Sitarama Raju Academy of Medical Sciences, 2020
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila

Dr. Mukkolu Satish
Orthopaedician
10 Years • MBBS: AMC, Dr.NTR University of Health Sciences in Vijayawada, Andhra Prades 2010, MS: 2015 Orthopaedics Andhra Medical College, VSP
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila
Consult a Top Orthopaedics

Dr. Naveen Palla
Orthopaedician
18 Years • MS
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila
(75+ Patients)

Dr. B. Harsha Vardhana Reddy
Orthopaedician
10 Years • "#MBA (Hospital Administration) – ICFAI University – 2021 #DNB (Orthopaedics) – Continental Hospital, Hyderabad – 2020 #Fellowship in Arthroscopy – Continental Hospital, Hyderabad – 2018 #Fellowship in Arthroplasty – Continental Hospital, Hyderabad – 2017 #D.Ortho – Dr. G.S. Kulkarni Orthopaedic Institute, Miraj (MUHS) – 2015 #MBBS – K.V.G Medical College, Bangalore (RGUHS) – 2012"
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr. Prashanth Reddy A
Orthopaedician
13 Years • "2006-2012 MBBS CHALMEDA ANAND RAO INSTITUTE OF MEDICAL SCIENCES -KARIMNAGAR,TELANGANA 2013- 2016 DNB Ortho Care Hospitals - Banjara Hills,Hyderabad 2018-2021 M.Ch (Hip & knee) EDGEHILL UNIVERSITY-WRIGHTINGTON HOSPITAL - WRIGHTINGTON,UK"
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr. Surendra Yellapu
Orthopaedician
8 Years • MBBS: Konaseema Inst. of Medical Sciences & Research Foundation in Amalapuram, Andhra Pradesh, 2013 • MS: Orthopaedics in Alluri Sitarama Raju Academy of Medical Sciences, 2020
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila

Dr. Mukkolu Satish
Orthopaedician
10 Years • MBBS: AMC, Dr.NTR University of Health Sciences in Vijayawada, Andhra Prades 2010, MS: 2015 Orthopaedics Andhra Medical College, VSP
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila
More articles from Blocked Blood Vessels
Frequently Asked Questions
Is bypass surgery better than stents?
It depends on your disease pattern. For left main, triple-vessel, or diabetic multivessel disease, bypass surgery often provides better long-term outcomes than PCI (stents). Shared decision-making with your heart team is key.
How long do bypass grafts last?
LIMA arterial grafts can remain open for decades; saphenous vein grafts have lower long-term patency. Medications and lifestyle changes significantly improve graft longevity.
How long will recovery take after cardiac surgery?
Many people leave the hospital in 5–7 days, resume light activities in 2–4 weeks, and return to work in 6–8 weeks, supported by cardiac rehabilitation. Timelines vary by age, health, and surgery complexity.
What medications will I need after CABG?
Most patients take aspirin, a high-intensity statin, and often a beta-blocker. Depending on your condition, you may need ACE inhibitors/ARBs or dual antiplatelet therapy, especially after a recent heart attack.
What are the warning signs after heart bypass surgery?
Fever, wound redness or drainage, new chest pain, shortness of breath, leg swelling/redness, or persistent palpitations need prompt evaluation. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.