Guide to Frequently Asked Questions Brain Aneurysms
Know about brain aneurysm, what it is, causes, risks, symptoms, diagnosis, screening, treatment options and preventive and lifestyle. Learn about life after surgery and more.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026
Introduction
A brain aneurysm sounds frightening, and the internet doesn’t always make things clearer. What exactly is it? How common is it? Which symptoms should send you to the emergency room—and when is watchful waiting safe? This guide brings together trusted answers to your most pressing questions about brain aneurysms, from symptoms and diagnosis to treatment choices and recovery. You’ll learn how risk factors like smoking and high blood pressure raise your chances, what “unruptured” vs “ruptured” really means, how tests like CT angiography and MR angiography work, and what living well looks like after repair. If symptoms persist or you’re unsure about next steps, you can consult a doctor online with Apollo24|7 for timely guidance and, when appropriate, arrange an in‑person visit. By the end, you’ll have a clear, compassionate roadmap to navigate brain aneurysms with confidence
Consult a Top Neurologist for Personalised Advice
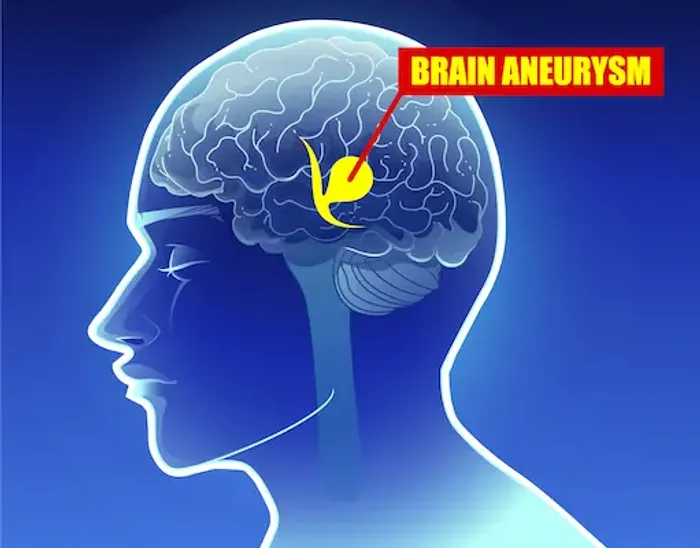
Brain aneurysm basics: What they are and the main types
A brain aneurysm is a bulge or ballooning in a blood vessel wall within the brain. Most form at branching points of arteries where flow is turbulent and the vessel wall is naturally thinner. Over time, factors like high blood pressure and smoking can weaken the wall, allowing it to balloon. Many aneurysms never cause symptoms; others can press on nearby structures or, rarely but urgently, rupture and bleed around the brain—a medical emergency called subarachnoid haemorrhage (SAH).
Types matter because they influence risk and treatment:
- Saccular (berry) aneurysms are the most common, resembling a small sac on the side of an artery. These are typically the ones discussed in screening and repair decisions [3].
- Fusiform aneurysms cause a spindle‑shaped widening of the vessel itself and may relate more to vessel wall disease.
- Mycotic (infectious) aneurysms, uncommon, result from infection weakening the vessel wall.
Size and location also guide decisions. Small aneurysms (<5–7 mm) in the front circulation often carry a lower immediate risk of rupture than large or irregularly shaped aneurysms or those at the posterior communicating artery or basilar tip. Advanced endovascular options (coiling, flow diverter stents) and surgical clipping are tailored to aneurysm type, shape, and neck width. Understanding these basics helps explain why two people with “brain aneurysms” might receive very different recommendations ranging from periodic imaging to urgent repair..
How common are brain aneurysms, and who is at risk?
Brain aneurysms are more common than many realise: about 1 in 50 people (around 2–3%) have an unruptured
aneurysm, often discovered incidentally during scans done for other reasons. The annual rate of rupture is low overall, but because the consequences can be severe, recognising risk factors is crucial. In the U.S., roughly 30,000 people per year experience a rupture, and about 10–15% die before reaching the hospital; among survivors, neurologic disability is common.
Risk factors fall into two broad categories:
- Non‑modifiable: female sex (slightly higher risk), age (most aneurysms are identified in adults 35–60), and certain inherited conditions like autosomal dominant polycystic kidney disease (ADPKD) and Ehlers‑Danlos syndrome.
- Modifiable: cigarette smoking, high blood pressure, heavy alcohol use, and stimulant drugs (e.g., cocaine), all of which increase the formation and rupture risk. Smoking and hypertension together substantially magnify risk.
Family history matters. Having two or more first‑degree relatives (parent, sibling, child) with aneurysm or aneurysmal SAH raises your risk; many experts advise screening in such families with MR angiography (MRA) or CT angiography (CTA) at intervals, even if you have no symptoms [4][8]. For most people without family history or syndromic risk, routine screening is not recommended. Knowing where you fit on the risk spectrum helps you and your clinician decide whether to screen, monitor, or act.
Symptoms: Unruptured vs ruptured, how to recognise the warning signs
Most unruptured aneurysms cause no symptoms. When they do, it’s usually from size or location—for example, an
aneurysm near the eye nerves can cause drooping eyelid, double vision, or a dilated pupil. Chronic headaches are common in the general population and usually not due to an aneurysm, but a new pattern of severe headaches, especially with neurologic symptoms (vision changes, numbness, weakness), deserves evaluation.
A “sentinel headache” (a brief warning leak) can occur days to weeks before a major rupture. It’s often described as a sudden, severe headache different from any prior headache, sometimes with neck pain, light sensitivity, or nausea. If you or someone you’re with experiences the “worst headache of your life,” especially with fainting, confusion, stiff neck, vomiting, vision loss, or weakness, call emergency services immediately. Ruptured aneurysms cause subarachnoid haemorrhage, which can be rapidly life‑threatening and benefits from early neurocritical care.
When to call vs consult:
- Call emergency services now for a thunderclap headache, loss of consciousness, seizure, sudden neurological deficits, or
severe headache with neck stiffness. - For persistent or worsening headaches, new neurologic symptoms, or questions about your risk, consult a doctor online
with Apollo24|7 for triage and guidance. If your condition does not improve or red flags appear, book a physical visit promptly.
Diagnosis and screening: Tests you may need and why
The choice of test depends on urgency and the question at hand.
Emergency assessment:
- Non‑contrast head CT is the first‑line test if a ruptured aneurysm (SAH) is suspected. Within six hours of onset, modern
CT can be highly sensitive for detecting SAH [11]. After that window, sensitivity decreases. - If CT is negative but suspicion remains high, a lumbar puncture can detect blood breakdown products in cerebrospinal fluid, confirming SAH even when CT is normal.
Screening:
- People with two or more first‑degree relatives affected by aneurysm/SAH, or those with certain genetic conditions (e.g., ADPKD), can discuss periodic screening MRA/CTA with their clinician.
- Routine screening is not recommended for the general population without risk factors.
If you’re unsure which test you need, a clinician can help weigh factors like kidney function, allergies, claustrophobia, and the need for speed. You can consult a doctor online with Apollo24|7 to review symptoms and decide on the most appropriate next step.
Treatment choices: Observe or repair?
Not every brain aneurysm needs immediate repair. The decision balances the risk of rupture against the risks of
intervention, factoring in aneurysm size, shape (irregular or “daughter sacs” raise concern), location, your age/health, and your preferences [4][5].
Watchful waiting:
- Small, asymptomatic aneurysms—especially in the front part of the circulation—are often monitored with periodic MRA/CTA, along with aggressive risk‑factor control (stop smoking, control blood pressure).
- Follow‑up imaging intervals vary (often 6–12 months initially, then every 1–2 years).
Endovascular options:
- Coiling: Through a groin or wrist artery, a catheter delivers soft platinum coils into the aneurysm sac to promote
clotting and isolate it from circulation. For many ruptured aneurysms, coiling is associated with lower disability at 1
year compared with clipping (ISAT trial), though re‑treatment rates can be higher. - Stent‑assisted coiling and flow diverter stents: Used for wide‑necked or complex aneurysms, flow diverters redirect blood along the parent artery, promoting aneurysm healing over time.
- The WEB device (intrasaccular flow disruptor) is another option for some bifurcation aneurysms in specialised centres.
Surgical clipping:
A neurosurgeon performs a craniotomy to place a small clip across the aneurysm neck, permanently excluding it from
circulation. Clipping is durable and preferred in certain locations or anatomies and for some younger patients.
Choosing a centre and specialist:
- Outcomes are generally better at high‑volume centres with multidisciplinary teams (neurosurgery, interventional neuroradiology, neurocritical care). Ask about your team’s annual case volumes and complication rates.
- When time allows, consider a second opinion; telemedicine can make this convenient.
Recovery and living well after aneurysm repair or rupture
Hospital care after rupture focuses on preventing complications:
- Vasospasm (narrowing of brain arteries) can reduce blood flow for about days 3–14 after SAH. Nimodipine, a calcium
channel blocker, reduces poor neurologic outcomes after SAH and is standard therapy [10][13]. - Other risks include hydrocephalus (fluid buildup), seizures, hyponatremia, and infections. ICU monitoring enables early detection and treatment.
Rehabilitation:
- Many survivors experience fatigue, memory or attention difficulties, mood changes, or headaches. Early physical,
occupational, and speech therapy accelerates recovery, and neuropsychological support helps address
cognitive/emotional effects [3][6]. - Return to work and driving are individualised; some people return in weeks after elective unruptured aneurysm repair,
while post‑SAH recovery can take months. Start with light activities and increase as advised by your team.
Living with an unruptured aneurysm:
- Daily life usually includes normal activity, with advice to avoid smoking, control blood pressure, and limit heavy
straining. Most people can fly, exercise moderately, and have sex safely once cleared by their clinician [2][5]. - Pregnancy: Many can safely carry a pregnancy after individualised counselling with obstetrics and neurosurgery. Plans
should address the delivery mode based on aneurysm status and overall obstetric factors.
Support for caregivers:
Caregivers can help structure routines, track medications, and watch for warning signs (worsening headaches, confusion, weakness, fever). Support groups (online and local) provide valuable practical and emotional help.
If recovery stalls, new symptoms appear, or you need coordinated follow‑up, book a visit with a doctor. If accessing care is a challenge, Apollo24|7 can arrange teleconsults and guide you to in‑person services.
Prevention and lifestyle: Lowering your risk day to day
While you can’t change your age or genetics, you can meaningfully reduce aneurysm formation and rupture risk:
- Control blood pressure. Aim for targets your clinician recommends; take medications consistently. Home BP monitors
help. If you need lab monitoring for conditions like diabetes or cholesterol, Apollo24|7 offers convenient home
collection for tests such as lipid profile or HbA1c. - Stop smoking. This is the single most important modifiable factor; cessation lowers both formation and rupture risk [2]
[6]. Combine counselling, nicotine replacement, and medications if needed. - Moderate alcohol; avoid cocaine and other stimulants, which markedly raise haemorrhage risk.
- Exercise regularly and manage stress. Most people with unruptured aneurysms can do moderate exercise. Build
gradually and avoid sudden, extreme straining unless your doctor advises otherwise. - Headache hygiene: sleep regularly, hydrate, and manage triggers. Seek care for new or worsening patterns.
Related terms: brain aneurysm prevention tips; when to see a doctor for a severe headache.
Costs, access, and getting the right care
Costs vary widely by country, insurance, and procedure type. In general, surgical clipping and endovascular procedures
can be expensive due to specialised teams, devices, and hospital stays. Up‑front costs may be higher for flow diverter
stents, but they can reduce re‑treatments in suitable cases. Ask your insurer about coverage for imaging, inpatient care,
and rehabilitation.
Access and second opinions:
- If time allows, seek a second opinion at a comprehensive stroke or high‑volume neurovascular centre. Telemedicine
makes it easier to review imaging and options without travel. - Apollo24|7 can facilitate online consultations for second opinions, ongoing blood pressure and medication
management, and timely referrals. If your condition does not improve after trying these methods, book a physical visit
to a doctor with Apollo24|7.
Conclusion
Brain aneurysms sit at the intersection of uncommon but serious conditions. The good news: most aneurysms never
rupture, and today’s diagnostic tools and treatments are safer and more precise than ever. The essentials to remember
are simple. First, know the red flags—sudden, severe headache unlike any before, especially with neurologic
symptoms—and seek emergency care without delay. Second, understand your personal risk factors. Stopping smoking and controlling blood pressure are the two most powerful steps you can take. Third, if an aneurysm is found, decisions about observation versus repair depend on size, shape, location, and your overall health. Finally, recovery is a journey. Plan for physical and cognitive rehabilitation, ask your care team about activity, travel, and work, and make follow‑up imaging a priority.
Consult a Top Neurologist for Personalised Advice
Consult a Top Neurologist for Personalised Advice

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(100+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr Rajashekar Mummadi
Neurologist
3 Years • MBBS, DNB General Medicine, DRNB Neurology
Hyderabad
Dr Ram's Neuro Clinic, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
Consult a Top Neurologist for Personalised Advice

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Aditendraditya Singh Bhati
Neurosurgeon
21 Years • MBBS(2004), DNB Neurosurgery(2014); MNAMS; Fellow Skull Base Endoscopy (Italy), Fellow Extended Skull Base ( Weill Cornell, USA), Fellow ZAP-X Radiosurgery. Member of American Association of Neurological Surgeons
Delhi
Apollo Hospitals Indraprastha, Delhi
(100+ Patients)

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr Rajashekar Mummadi
Neurologist
3 Years • MBBS, DNB General Medicine, DRNB Neurology
Hyderabad
Dr Ram's Neuro Clinic, Hyderabad

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)
More articles from Brain Aneurysm
Frequently Asked Questions
1) Is a sudden, severe headache always a ruptured brain aneurysm?
No. Most severe headaches are not aneurysms, but a thunderclap headache (peaking in seconds) can signal subarachnoid haemorrhage. Treat it as an emergency and seek immediate care. If symptoms persist beyond two weeks without red flags, consult a doctor online with Apollo24|7 for further evaluation. Related term: when to see a doctor for a severe headache.
2) Do small brain aneurysms always need surgery?
Not always. Many small, unruptured aneurysms—especially in the front circulation—can be observed with periodic imaging and strict control of blood pressure and smoking cessation. Your specialist will tailor the follow‑up frequency. Related term: small brain aneurysm follow‑up guidelines.
3) Which is better: coiling or clipping?
It depends on your aneurysm’s anatomy and your health. For many ruptured aneurysms, endovascular coiling had better 1‑year outcomes than clipping in the ISAT trial, but clipping can be preferred for certain locations or patient profiles. Discuss both options and your team’s experience. Related term: endovascular coiling vs surgical clipping outcomes.
4) Can I exercise, fly, or have sex with an unruptured aneurysm?
Most people can do these activities after individualised advice from their clinician. Moderate exercise is encouraged; avoid extreme straining unless cleared. Commercial air travel is generally safe when stable. Related term: brain aneurysm prevention tips.
5) Should my family be screened for brain aneurysms?
If you have two or more first‑degree relatives with aneurysm or aneurysmal SAH, screening with MRA/CTA may be advised. Otherwise, routine screening is not recommended for the general population. Related term: screening for brain aneurysm family history.
.webp)
