Neurodegenerative Diseases: Types, Causes, and Early Signs
Learn about neurodegenerative diseases—their types, causes, risk factors, and early warning signs. Discover how conditions like Alzheimer’s and Parkinson’s develop and when to seek medical help.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026

Introduction
Have you or a loved one experienced memory lapses, a slight tremor, or unexplained changes in mood? While these can be a normal part of ageing, they are also potential early warning signs of a deeper issue. Neurodegenerative diseases represent a group of debilitating disorders characterised by the progressive loss of structure or function of neurons, the building blocks of our nervous system. These conditions, including Alzheimer’s and Parkinson’s disease, can feel overwhelming, but understanding them is the first step towards empowerment. This article will demystify these complex diseases. We’ll explore what they are, delve into the biological mechanisms that lead to their development, list the most common types, and outline the critical early signs to watch for. Our goal is to provide you with clear, actionable knowledge to help you navigate health concerns and know when to seek professional guidance.
What Are Neurodegenerative Diseases? The Basics
Neurodegenerative diseases are a collection of disorders primarily affecting the neurons in the human brain. Neurons are specialised cells designed to transmit information to other nerve cells, muscles, or gland cells. Unlike other cells in the body, neurons generally do not regenerate after injury or death. This makes the brain and spinal cord particularly vulnerable.
The Common Thread: Progressive Nerve Cell Damage
The defining feature of all neurodegenerative diseases is their progressive nature. This means the condition worsens over time, as more and more neurons become damaged and die. This neuronal loss disrupts the complex communication networks within the brain, leading to the problems with movement (called ataxias), mental functioning (called dementias), and other neurological deficits that characterise these disorders. The specific symptoms a person experiences depend entirely on which type of neuron is being affected and in which region of the brain the degeneration is occurring.
Unravelling the Causes: What Triggers Neurodegeneration?
The exact initial trigger for most neurodegenerative diseases remains an active area of research. However, scientists have identified several key interconnected processes that contribute to the damage and death of nerve cells.
The Genetic Blueprint: Inherited Mutations
For some diseases, like Huntington’s disease, a single inherited genetic mutation is the direct cause. If a parent has the gene, a child has a 50% chance of inheriting it and developing the disease. In other cases, such as early-onset Alzheimer’s, specific gene variants (like APP, PSEN1, and PSEN2) greatly increase risk. More commonly, genes like APOE-e4 act as risk factors, making a person more susceptible but not guaranteeing they will develop the condition.
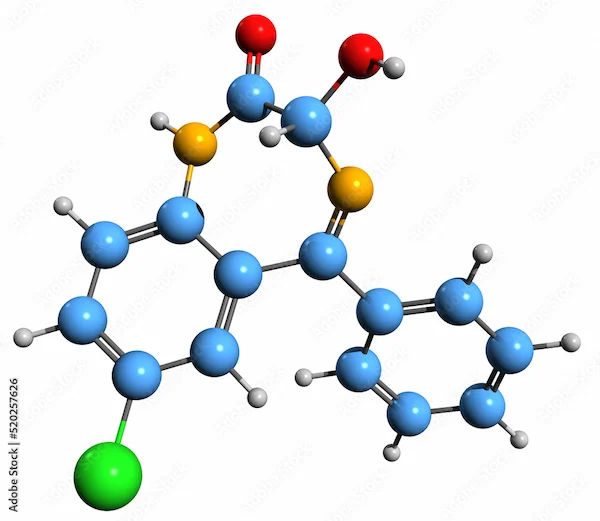
Protein Misfolding: A Cellular Traffic Jam
A hallmark of many neurodegenerative conditions is the accumulation of misfolded proteins in and around neurons. These malfunctioning proteins clump together, forming toxic aggregates that disrupt cellular function.
In Alzheimer’s disease, it’s amyloid-beta plaques and tau tangles.
In Parkinson’s disease, it’s clumps of a protein called alpha-synuclein, known as Lewy bodies.
In ALS and frontotemporal dementia, it’s the TDP-43 protein.
These clumps interfere with neuron communication, activate inflammatory responses, and ultimately lead to cell death.
Oxidative Stress: The Rusting of the Brain
The brain is highly metabolically active, consuming vast amounts of oxygen. This process naturally generates free radicals—unstable molecules that can damage cells. Normally, the body neutralises them with antioxidants. When the balance is upset, oxidative stress occurs, leading to damage to neurons’ lipids, proteins, and DNA. This “rusting” is a significant contributor to the progressive nerve cell damage seen in these disorders.
Mitochondrial Dysfunction: The Power Plant Failure
Mitochondria are the powerhouses of every cell, including neurons. They generate the energy needed for the cell to survive and function. In many neurodegenerative diseases, mitochondrial function breaks down. Without adequate energy, neurons cannot maintain their health, leading to dysfunction and apoptosis (programmed cell death). This is particularly relevant in Parkinson’s disease, where toxins that inhibit mitochondrial complex I have been linked to the condition.
Consult a Neurologist for Personalised Advice
Major Types of Neurodegenerative Diseases
While there are dozens of rare disorders, a few major types account for the majority of cases.
Alzheimer’s Disease: The Most Common Culprit
Alzheimer’s is the most prevalent neurodegenerative disease, accounting for 60–80% of dementia cases. It primarily affects brain regions involved in memory, like the hippocampus and entorhinal cortex.
Key Signs and Affected Brain Regions
Early signs include difficulty remembering recent conversations, names, or events, followed by apathy and depression. Later, impaired communication, disorientation, and behavioural changes occur as the disease spreads to the cerebral cortex.
Parkinson’s Disease: Beyond the Tremors
Parkinson’s disease is primarily a movement disorder caused by the degeneration of dopamine-producing neurons in a region of the brain called the substantia nigra.
Key Signs and the Role of Dopamine
The classic motor symptoms include a resting tremor, slowness of movement (bradykinesia), rigidity, and postural instability. These occur because the loss of dopamine disrupts the brain’s ability to control movement smoothly. Non-motor symptoms, such as loss of smell, sleep disorders, and cognitive changes, are also common and can appear years before motor issues.
Amyotrophic Lateral Sclerosis (ALS): The Attack on Motor Neurons
ALS, also known as Lou Gehrig’s disease, is a progressive disease that attacks the nerve cells (motor neurons) responsible for controlling voluntary muscles. As these neurons die, the brain loses its ability to initiate and control muscle movement, leading to paralysis.
Huntington’s Disease: A Genetic Certainty
Huntington’s disease is an inherited, autosomal dominant disorder caused by a defect on chromosome 4. It causes the progressive breakdown of nerve cells in the brain, particularly in the basal ganglia, which control movement, and the cortex, which controls thought, perception, and memory. Symptoms include uncontrolled movements (chorea), emotional problems, and loss of cognition.
Other Notable Neurodegenerative Conditions
Frontotemporal Dementia (FTD): Affects the frontal and temporal lobes of the brain, leading to changes in personality, behaviour, and language.
Spinal Muscular Atrophy (SMA): An inherited disorder that affects motor neurons in the spinal cord, leading to muscle wasting and weakness.
Multiple System Atrophy (MSA): A rare disorder that affects both the autonomic nervous system and movement.
Recognising the Early Signs and Symptoms
Early detection is crucial for managing these diseases. The signs can be subtle and are often mistaken for normal ageing.
Cognitive and Memory Warning Signs
Memory loss that disrupts daily life (especially recently learned information).
Challenges in planning or solving problems.
Difficulty completing familiar tasks.
Confusion with time or place.
Physical and Motor Warning Signs
Tremors or shaking, especially at rest.
Stiffness of limbs and slowness of movement (bradykinesia).
Changes in handwriting, often becoming smaller.
Frequent stumbling or loss of balance.
Muscle weakness or twitching.
Behavioural and Psychological Changes
Withdrawal from work or social activities.
Changes in mood and personality, such as increased anxiety, depression, or irritability.
Loss of initiative or apathy.
If you or a loved one are experiencing persistent symptoms beyond typical age-related changes, it is essential to consult a doctor for a professional evaluation. You can book an online consultation with an experienced neurologist on Apollo24|7 to discuss your concerns from the comfort of your home.
Key Risk Factors You Should Know
Understanding risk factors can help in awareness and potential prevention strategies.
Unmodifiable Risk Factors: Age, Genetics, and Sex
Age: The single greatest risk factor for most neurodegenerative diseases. The incidence rises dramatically after age 65.
Genetics: A family history of a specific disease increases risk.
Sex: Some diseases show a sex bias; for example, Alzheimer’s is more common in women, while Parkinson’s is more common in men.
Modifiable Risk Factors: Lifestyle and Environment
Cardiovascular Health: Hypertension, heart disease, stroke, diabetes, and high cholesterol all increase risk by affecting blood flow to the brain.
Head Trauma: A history of significant head injuries is a known risk factor.
Lifestyle: Lack of physical exercise, poor diet, smoking, and excessive alcohol consumption are linked to higher risk.
Environmental Toxins: Exposure to certain pesticides, herbicides, and heavy metals has been implicated in some studies, particularly for Parkinson’s.
Conclusion
Navigating the world of neurodegenerative diseases can be complex, but knowledge is a powerful tool. Understanding the biological mechanisms—from genetic predispositions to protein misfolding—helps demystify why these conditions develop. Recognising the early warning signs empowers individuals and families to seek timely medical advice, which is critical for accessing treatments that can slow progression and manage symptoms. While these diseases present significant challenges, ongoing research continues to advance our understanding and develop new therapeutic strategies. Maintaining a brain-healthy lifestyle—managing cardiovascular risk, staying physically and mentally active, and eating a balanced diet—is the best proactive step you can take for your neurological health. If you have concerns based on the signs discussed, do not hesitate to seek professional guidance. Early intervention can make a substantial difference in the long-term management of these conditions. You can schedule a physical visit with a
Consult a Neurologist for Personalised Advice
Consult a Neurologist for Personalised Advice

Dr. Ranjith G
Neurologist
10 Years • DM (Neurology) FSIN (Fellowship in stroke and intervention neurology) MD (Internal Medicine)
Hyderabad
Apollo Hospitals Financial District, Hyderabad
Dr Venkata Sumanth Chava
Neurologist
4 Years • "• DM neurology at Jawaharlal Nehru medical college, KLE academy of higher education and research, Belagavi. • MD internal medicine at JSS medical college, JSS academy of higher education and research, Mysuru. • MBBS at Prathima institute of medical sciences, Dr NTR university of health sciences, Karimnagar."
Hyderabad
Apollo Hospitals Financial District, Hyderabad

Dr. Saravanan P
Neurologist
11 Years •
Karur
Apollo Hospitals Allwyn Nagar, Karur
(25+ Patients)

Dr. Jitendra Nishikant Shukla
Neurologist
5 Years • MBBS DNB DNB (Neuro)
Nashik
Apollo Hospitals Nashik, Nashik
(25+ Patients)

Dr Justin Thomas
Neurologist
10 Years • MD DM NEUROLOGY
Bhopal
Apollo Sage Hospitals, Bhopal
More articles from Brain Degenerative Disorders
Frequently Asked Questions
What is the difference between dementia and Alzheimer’s?
Dementia is an umbrella term for a set of symptoms that include memory loss and cognitive decline severe enough to interfere with daily life. Alzheimer’s disease is the most common specific cause of dementia, accounting for the majority of cases. Not all dementia is Alzheimer’s.
Can you prevent neurodegenerative diseases?
While there is no guaranteed prevention, you can significantly reduce your risk by addressing modifiable factors. This includes managing blood pressure and cholesterol, maintaining a healthy weight, exercising regularly, engaging in cognitive activities, eating a Mediterranean-style diet, and avoiding smoking and excessive alcohol.
Are tremors always a sign of Parkinson’s disease?
No, not all tremors indicate Parkinson’s. Essential tremor is a common, often inherited condition that is typically action-based (happens when you move your hands). The classic Parkinson’s tremor is a “resting tremor,” meaning it occurs when the muscle is relaxed and often diminishes with voluntary movement. A neurologist can help differentiate between them.
Is neurodegenerative disease hereditary?
It depends on the specific disease. Huntington’s disease is directly inherited. For others like Alzheimer’s and Parkinson’s, most cases are “sporadic” with no clear family link. However, having a family history does increase your risk, suggesting a genetic predisposition combined with environmental factors.
What tests are used to diagnose these conditions?
There is no single test. Diagnosis involves a comprehensive approach: a detailed medical history, neurological exams, cognitive tests, blood tests (to rule out other causes like vitamin deficiencies), and brain imaging scans like MRI or CT. In some cases, genetic testing or cerebrospinal fluid analysis may be used. Apollo24|7 offers convenient home collection for blood tests that can help rule out other conditions as part of the diagnostic process.