A Guide to Laser Thermal Therapy for Brain Tumours
Discover how laser interstitial thermal therapy (LITT) offers a minimally invasive, precise treatment for brain tumours, enabling faster recovery and reduced risk compared to traditional surgery.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026

Introduction: A Minimally Invasive Revolution in Neurosurgery
Facing a brain tumour diagnosis is a daunting experience, often accompanied by the fear of complex brain surgery. However, advancements in medical technology have led to groundbreaking, less invasive options. One such innovation is laser interstitial thermal therapy (LITT), a procedure that is changing the landscape of neurosurgery. Often described as "laser ablation," this technique offers a precise and targeted way to destroy tumour cells with minimal impact on the surrounding healthy brain tissue. Imagine treating a deep-seated brain tumour not with a large incision and a long recovery, but with the pinpoint accuracy of a laser beam, all while the surgeon watches the process in real-time on an MRI screen. This article serves as a comprehensive guide to understanding how laser thermal therapy works, who it can help, and what the benefits and recovery process entail. We will demystify the science, walk you through the procedure step-by-step, and compare it to traditional methods, empowering you with the kno
What is Laser Interstitial Thermal Therapy (LITT)?
Laser interstitial thermal therapy (LITT) is a state-of-the-art, minimally invasive surgical technique used to ablate, or destroy, abnormal tissue in the brain, including tumours. The term "interstitial" means the procedure works from within the tissue itself, rather than removing it from the outside.
The Core Principle: Precise Heat to Destroy Tumour Cells
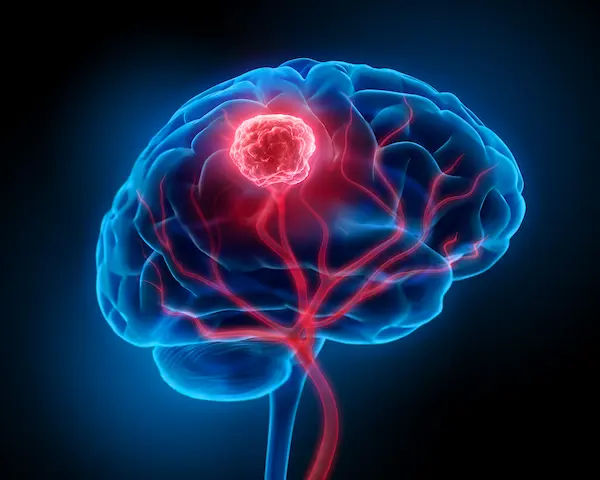
At its heart, LITT is elegantly simple. It uses the power of controlled heat to eliminate tumour cells. A very thin, flexible laser fibre, about the size of a toothpick, is guided precisely to the target area within the brain. Once in place, the laser emits light energy that is converted into heat. This heat raises the temperature of the tumour cells to a point where they are irreversibly damaged and ultimately die—a process known as thermal ablation. The key is the exquisite control over the heat's spread, which allows neurosurgeons to destroy the tumour while sparing the critical healthy brain tissue just millimetres away.
MR-Guided LITT: Seeing the Treatment in Real-Time
What makes LITT exceptionally safe and effective is its integration with magnetic resonance imaging (MRI). This combination is often called MR-guided LITT (MRgLITT). Throughout the entire procedure, the patient is inside an MRI scanner. This provides the surgical team with continuous, real-time temperature maps of the brain. They can see exactly how the heat is dispersing and can instantly adjust the laser's power to ensure only the intended tumour tissue is ablated. This real-time feedback loop is a critical safety feature, making laser ablation brain surgery a highly controlled and precise intervention.
Consult a Neuro-oncologist for the best advice
How Does the LITT Procedure Work? A Step-by-Step Guide
Understanding the procedure can alleviate much of the anxiety associated with it. Here’s a breakdown of what happens during a typical LITT treatment.
Step 1: Preoperative Planning and Imaging
Weeks or days before the procedure, you will undergo high-resolution MRI or CT scans. These images are uploaded into a sophisticated computer navigation system, which creates a 3D map of your brain. Using this map, your neurosurgeon plans the safest and most direct pathway to reach the tumour, determining the exact entry point on the skull and the trajectory for the laser catheter.
Step 2: The Day of the Procedure – Anaesthesia and Guidance
On the day of surgery, you will be placed under general anaesthesia. A small incision (about 1/4 inch) is made in the scalp, and a tiny burr hole is drilled through the skull. Using the pre-planned surgical navigation, a narrow catheter (a protective sheath) is carefully advanced through the burr hole until its tip rests within the centre of the tumour.
Step 3: Laser Insertion and Real-Time Ablation
Once the catheter is perfectly positioned, the laser fibre is inserted through it. The MRgLITT procedure then begins in earnest. You are moved into the MRI scanner, and the laser is activated in short pulses. The surgical team monitors the thermal ablation in real-time on their screens, watching as colour-coded maps show the heat effectively destroying the tumour. They can stop the laser at any moment to ensure the ablation zone conforms exactly to the tumour's shape.
Step 4: Confirmation and Completion
After the ablation is complete, a final MRI scan is performed to confirm that the entire target area has been treated. The laser fibre and catheter are then gently removed. The small incision is closed with stitches or surgical glue, often leaving only a minimal scar. The entire process typically takes a few hours, depending on the size and location of the tumour.
Who is a Candidate for Laser Ablation Brain Surgery?
LITT is not a one-size-fits-all solution, but it is an excellent option for many patients with specific types of brain lesions.
Ideal Conditions for LITT Treatment
LITT treatment works best for specific brain conditions—these are the ideal conditions for its use:
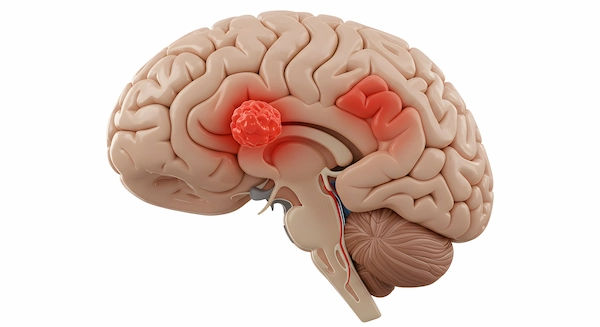
Deep-Seated or Hard-to-Reach Tumours: LITT is particularly valuable for tumours located deep within the brain, where traditional surgery would require navigating through critical functional areas, posing a high risk of neurological damage.
Recurrent Tumours: For tumours that have returned after previous radiation therapy or surgery, LITT offers a new treatment avenue without the risks associated with re-operation in scarred tissue.
Radiation-Necrosis: This is a condition where previously irradiated brain tissue becomes damaged and swollen. LITT can effectively ablate this necrotic tissue, relieving symptoms.
Certain Types of Brain Metastases: Tumours that have spread to the brain from other cancers (metastases) are often well-defined and suitable for laser ablation.
Epilepsy Foci: LITT is also used to ablate small areas of brain tissue responsible for triggering seizures that do not respond to medication.
When LITT Might Not Be the Best Option
LITT may be less suitable for very large tumours (typically over 3-4 cm), tumours that are diffuse and lack clear borders, or cases where a tissue sample for biopsy is the primary goal. The decision is always made by a multidisciplinary team. Consulting a neurosurgeon online with Apollo24|7 can be a good first step to understand if you are a potential candidate for this procedure.
Key Benefits of Choosing Laser Thermal Therapy
The advantages of LITT over traditional brain surgery are significant and contribute to its growing popularity.
Minimally Invasive Advantages: Smaller Incision, Less Disruption
Unlike a craniotomy, which requires a large incision in the scalp and the removal of a section of skull bone (bone flap), LITT requires only a tiny burr hole. This results in less blood loss, a lower risk of infection, and minimal disruption to the patient's body.
Precision and Safety: Protecting Healthy Brain Tissue
The real-time MRI guidance is the cornerstone of LITT's safety. This precision is paramount for treating tumours near critical areas that control speech, movement, or vision. The ability to create a custom-shaped ablation zone that matches the tumour exactly helps preserve neurological function.
Faster Recovery and Shorter Hospital Stay
Because LITT is less invasive, the recovery time is dramatically shorter. Many patients are discharged from the hospital within 1 to 2 days after the procedure, compared to a week or more for a craniotomy. They can return to their normal daily activities much sooner, which significantly improves their quality of life during treatment.
Potential Risks and Considerations of LITT
While LITT is generally very safe, like any surgical procedure, it carries potential risks. These can include:
Swelling (Oedema): The brain may swell in response to the treatment, which is typically managed with medication.
Neurological Deficits: There is a small risk of temporary or permanent neurological changes, such as weakness or speech difficulties, though the risk is lower than with traditional surgery.
Bleeding or Infection: These are risks with any surgery, but the small incision site makes them less common.
Incomplete Ablation: In some cases, not all tumour cells may be destroyed, potentially requiring further treatment.
It's essential to discuss these risks in detail with your neurosurgeon to make an informed decision.
What to Expect: The Recovery Process After LITT
Recovery from LITT surgery is typically swift. Patients often spend one night in the hospital for observation. They may experience a headache or fatigue for a few days, which is normal. Most people can resume light activities within a week. Follow-up MRI scans are scheduled periodically to monitor the treatment site and ensure the tumour is responding as expected. The faster recovery time is one of the most appreciated benefits among patients.
LITT vs. Traditional Craniotomy: A Clear Comparison
| Feature | Laser Interstitial Thermal Therapy (LITT) | Traditional Craniotomy |
| Incision | Small burr hole (keyhole) | Large scalp incision and bone flap removal |
| Invasiveness | Minimally invasive | Highly invasive |
| Hospital Stay | 1-2 days | 5-7 days or more |
| Recovery Time | Weeks | Months |
| Precision | High, with real-time MRI control | High, but reliant on the surgeon’s view and feel |
| Ideal For | Deep, recurrent, or well-defined tumours | Large, accessible tumours requiring debulking |
The Future of Brain Tumour Treatment with Laser Technology
Research into LITT is ongoing, with studies exploring its use for a wider range of brain conditions and in combination with other therapies like immunotherapy and chemotherapy. The technology itself continues to evolve, with improvements in laser fibre design and MRI software promising even greater precision and safety in the future.
Conclusion: Is LITT the Right Choice for You or Your Loved One?
Laser interstitial thermal therapy represents a significant leap forward in the compassionate and effective treatment of brain tumours. By offering a less invasive path with a faster recovery, it reduces the physical and emotional burden on patients and their families. However, the decision to pursue LITT is a highly personal and complex one that depends on the specific type, size, and location of the tumour, as well as the patient's overall health. The most important step is to have a detailed conversation with a qualified neurosurgical team. They can provide a comprehensive evaluation and explain whether this advanced laser thermal therapy is the most appropriate strategy for your unique situation. If you have received a diagnosis and are evaluating treatment options, booking a physical visit to a specialist with Apollo24|7 can connect you with the expert care you need.
Consult a Neuro-oncologist for the best advice
Consult a Neuro-oncologist for the best advice

Dr. Amit Choraria
Surgical Oncologist
18 Years • MBBS, MS (Surgery) Fellow, Surgical Oncology, Tata Medical Center (FSO) Fellow, European Board of Surgery (Surgical Oncology) (FEBS) Fellow, Minimal Access Surgery (FMAS) Fellow, Indian Association of Gastrointestinal Endosurgeons (FIAGES) UICC Fellow, Royal Marsden NHS, London, UK Visiting Scholar, Plastic Reconstructive Surgery, CGMH, Taiwan Fellow, Robotic Surgical Oncology, Vattikuti Foundation, USA
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata
(75+ Patients)

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr Devashish Tripathi
Radiation Specialist Oncologist
20 Years • MBBS, PLAB, MRCP (UK)- General Medicine, FRCR (Oncology), Certificate of Completion of Training (CCT)- Clinical Oncology
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Harsh J Shah
Surgical Oncologist
15 Years • MS, MCh (GI), DrNB (GI)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
More articles from Brain Tumor
Frequently Asked Questions
1. Is LITT considered a cure for brain tumours?
LITT is a highly effective treatment for destroying visible tumour tissue, but it is not always a cure. Its goal is often to achieve local tumour control, alleviate symptoms, and improve quality of life. For malignant tumours, it may be part of a larger treatment plan that includes radiation or chemotherapy.
2. How long do the effects of the laser ablation last?
The ablated tumour tissue is permanently destroyed. The long-term success depends on the tumour type. Follow-up scans are essential to monitor for any potential recurrence. For many patients, the results are long-lasting.
3. What is the success rate of laser ablation for glioblastoma?
For well-selected cases of recurrent glioblastoma, studies have shown that LITT can provide effective local control and extend survival with a favourable safety profile. However, success rates vary and should be discussed with your neurosurgeon in the context of your specific case.
4. Does insurance cover the cost of laser ablation brain surgery?
Most major insurance providers, including Medicare, cover LITT when it is deemed medically necessary. Prior authorisation is typically required. It's best to check with your insurance company and the hospital's billing department for specific details.
5. Are there any activity restrictions after LITT?
Patients are generally advised to avoid strenuous activities, heavy lifting, and driving for a few weeks after the procedure. Your medical team will provide specific instructions based on your individual recovery progress.