Interventional Radiology: Everything You Need To Know!
Discover the principles, benefits, risks, and advancements of interventional radiology, a minimally invasive medical speciality that uses imaging techniques to diagnose and treat various conditions.

Written by
Last updated on 3rd Jul, 2025
Interventional radiology (IR) is a subspecialty of radiology that uses minimally invasive procedures to diagnose and treat various conditions. It leverages imaging technologies like X-ray, computed tomography (CT) scan, ultrasound and magnetic resonance imaging (MRI) to provide the ideal solutions to many health problems.
Since the 1960s, interventional radiologists have explored alternatives to open surgery. Advances in imaging and surgical technology over the past two decades have significantly progressed the field. This article discusses what interventional radiology is, why it is useful, what can go wrong, and where it is used in the world of contemporary medicine.
Common Techniques and Procedures of Interventional Radiology
In the interventional radiology (IR) technique, interventional radiologists perform a wide range of procedures, including:
Angiography: Interventional radiologists perform an angiography, which is a type of X-ray study. This helps diagnose areas for blockage or narrowing in arteries.
Angioplasty: An angioplasty, a thin-walled, balloon-tipped catheter, is used, and it is injected inside a blood vessel to unblock the narrowing blockages and bring back the regular flow of blood inside the blood vessel.
Embolisation: Embolisation is done by infusing a substance via a catheter to cut blood supply in certain vessels. It is mainly utilised to control bleeding or treat tumours by preventing the supply of blood to the tumour.
Gastrostomy Tube Placement: For patients who cannot take food orally, interventional radiologists insert a feeding tube into the stomach. This procedure is used effectively to feed people who have swallowing disorders or any other conditions.
Intravascular Ultrasound: Interventional radiologists also use an ultrasound to get a clear view of blood vessels and identify certain problems within them, such as narrowing or plaque formation. It plays a role in diagnosing and planning the treatment of vascular disorders.
Stent Placement: A stent is a small coil placed into the blood vessels to regularise the blood flow at the locations of blockages. This process assists in alleviating the blood supply of the affected organ, which may be chronically deprived due to obstruction or constriction of its blood vessels, mainly arteries.
Foreign Body Removal: When foreign objects are trapped in blood vessels, interventional radiologists employ catheters to eliminate such objects.
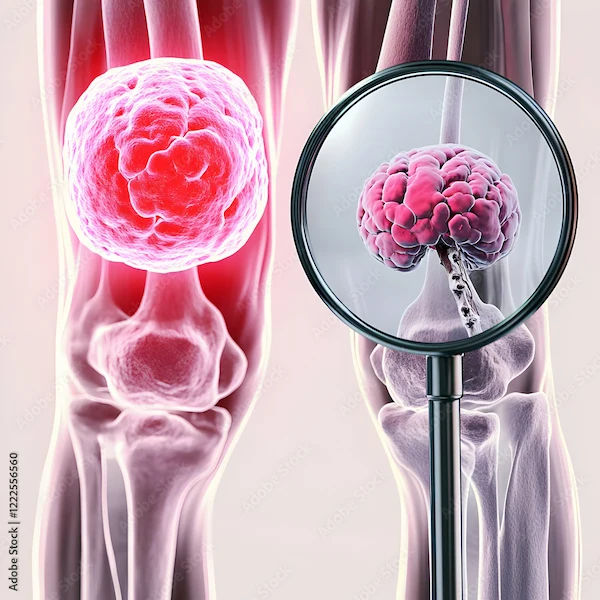
Needle Biopsy: Interventional radiologists can directly insert a small needle into a specific section of the body in order to extract samples of tissue. This method is less invasive than surgeries.
Inferior Vena Cava (IVC) Filter Placement: In this process, a small filter is implanted in the inferior vena cava in order to filter out any clots that may have formed in the body from reaching the lungs. This process helps lessen the risk of pulmonary embolism in patients.
Intraluminal Deposits of Clot Dissolving Medicines: The doctor often uses clot-busting drugs, which are tissue plasminogen activator medications. These are the drugs which dissolve in blood clots and regulate the flow of blood to arms, limbs, or other organs of the body.
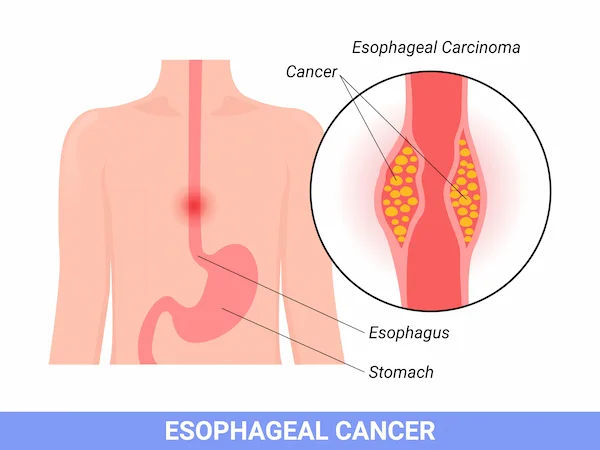
Catheter Insertions: For some instances, cancer medications are given by interventional radiologists directly to tumour sites via catheters. This targeted therapy allows for a more effective approach by directly addressing cancers at the affected site.
Cancer Treatment: At times, interventional radiology doctors inject cancer medications into the bodies using catheters and directly to the tumour regions. Such treatment is also effective for cancer since it targets the areas where it will have the most impact.
Benefits of Interventional Radiology
Here are the key advantages of interventional radiology (IR):
Enhanced Effectiveness
The interventional radiology (IR) technique has enabled radiologists to view patients’ disorders clearly during procedures, thereby improving diagnostic accuracy and better treatment outcomes.
Reduced Risks
Interventional radiology (IR) concerns itself with less blood loss and has fewer chances of getting infected than surgery. It is safer for those at higher risk of anaesthesia since only local anaesthesia or minor sedation is applied. It also reduces the probability of damaging the surrounding healthy cells or tissues.
Outpatient vs. Inpatient Stays
All the interventional radiology (IR) processes are performed on an outpatient basis. Hence, patients are discharged immediately after the procedure.
Lower Costs
Outpatient procedures often cost significantly less compared to that of inpatient hospital admission.
Less Pain
Interventional radiology (IR) procedures are minimally invasive. This is why there is no need to suture, apply staples, or use a large dressing. Local anaesthesia is used routinely, and so there is minimal pain during or after the procedure.
Faster Recovery
Interventional radiology (IR) procedures are less invasive, and recovery time is short. The patients get back into their daily lives faster than when they do so after conventional surgery.
Versatility
Interventional radiology (IR) can be used to identify various medical conditions, such as heart problems, liver disorders, kidney diseases, and cancer.
Risks and Complications Associated with Interventional Radiology
The following are the major risks and complications associated with interventional radiology (IR):
Haemorrhage
The complication of excessive bleeding may occur during or after interventional radiology procedures and lead to haemorrhage in vessels. These must be addressed quickly by performing an embolisation process. In severe circumstances, the problem could require surgery.
Infection
Surgery uses an invasive technique, which may expose the patient to infection risks at the point of needle insertion or at the organ that was targeted. The best prevention is the use of prophylactic antibiotics and using sterile measures where necessary.
Allergic Reactions
Contrast media such as iodinated contrast agents applied during many interventional radiology (IR) procedures can cause allergies from mild to severe, including anaphylactic reactions.
Organ Perforation
Although quite rare, perforation of organs can occur in processes such as biopsies or catheter placements. To avoid this situation, it is advised that the doctors perform imaging tests with accuracy and handle instruments with great care.
Radiation-Related Complications
Risks such as radiation dermatitis or increased cancer occurrence might be experienced by patients if exposed to radiation for long or frequently.
Emerging Procedures and Future Prospects in Interventional Radiology
The future of interventional radiology is greatly influenced by newer technologies that increase accuracy, decrease risk, and improve patient outcomes. Here are some examples of evolving technologies that could transform interventional radiology (IR):
Robotics: Robotic systems are enhancing the accuracy of complicated medical procedures such as biopsy, tumour resection, and stent placements. They also decrease the radiologist's exposure to ionising radiation and improve safety.
Nanotechnology: The use of nanoparticles allows drug delivery to the affected area or tumour site, causing minimal damage to the healthy tissues. This emerging technique is going to allow a future of more efficient and less harmful treatment.
Artificial Intelligence (AI): Artificial Intelligence (AI) has been increasing the accuracy of diagnosis and treatments by analysing medical images and helping radiologists. Predictive model algorithms determine patients at a higher risk for adverse postoperative complications and optimise their care.
3D Printing: A facility for 3D (three-dimensional) printing opens the path for creating models tailored to individual patients, which plays a vital role in ensuring a smooth treatment and decreasing procedural risk.
Conclusion
Interventional radiology (IR) has effectively replaced traditional diagnostic approaches to many diseases by providing less invasive treatments. Its advantages include reduced recovery time, fewer complications, and lower healthcare costs. With ongoing advancements, interventional radiology (IR) is expected to play an even more prominent role in both diagnosing and treating a wide range of diseases and conditions across medical science.
Consult Top Radiation Oncologist
Consult Top Radiation Oncologist

Dr. Rupam Manna
Radiation Specialist Oncologist
4 Years • MBBS MD(RADIO THERAPY)
Barasat
Diab-Eat-Ease, Barasat
Dr. Priya C
Radiation Specialist Oncologist
9 Years • MBBS
Bengaluru
Solasta Aesthetics, Bengaluru

Dr. Jayprakash Neema
Radiation Specialist Oncologist
37 Years • MD - Radiation Oncology
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad

Dr Devashish Tripathi
Radiation Specialist Oncologist
20 Years • MBBS, PLAB, MRCP (UK)- General Medicine, FRCR (Oncology), Certificate of Completion of Training (CCT)- Clinical Oncology
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Suman Das
Radiation Specialist Oncologist
13 Years • MD
Chinagadila
Apollo Hospitals Health City Unit, Chinagadila