Guide to Clubfoot Deformity What Do You Need Know
A comprehensive guide for parents on clubfoot—understand its causes, diagnosis, and effective treatments like the Ponseti method, ensuring a healthy, active future for your child.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026
Introduction
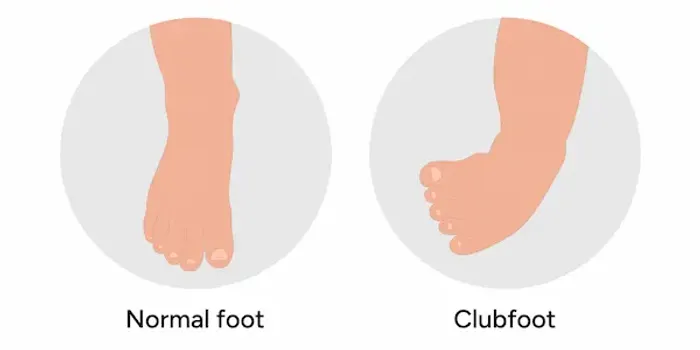
Seeing your newborn’s feet turned inward and downward can be an alarming moment for any parent. Clubfoot, known medically as congenital talipes equinovarus, is a common birth defect that affects a child's foot and ankle. But here’s the most important thing to know: clubfoot is highly treatable. With modern, non-surgical techniques, children born with this condition can go on to run, play, and lead fully active lives without any long-term disability. This guide will walk you through everything you need to know—from understanding what clubfoot is and what causes it, to the details of the highly effective Ponseti method of treatment. We’ll also address the emotional journey, providing reassurance and practical advice for navigating this manageable condition. If you suspect your child has a foot deformity, consulting a paediatric orthopaedist is the crucial first step.
What Exactly is Clubfoot?
Clubfoot is a congenital foot deformity, meaning it is present at birth. It involves the foot being twisted out of its normal position, resembling the head of a golf club—hence the name. The condition can affect one foot (unilateral) or both feet (bilateral). It is not a painful condition for the infant, but if left untreated, it can lead to significant difficulty walking and long-term physical problems.
The Medical Definition of Talipes Equinovarus
The medical term, talipes equinovarus, precisely describes the deformity:
- Talipes: Refers to the ankle (talus) and foot (pes).
- Equinus: The foot is pointed downward, like a ballerina's en pointe position, due to a tight Achilles tendon.
- Varus: The heel is turned inward, and the front half of the foot (forefoot) is also adducted, or curved inward.
This combination of positions makes the foot rigid and unable to be moved into a normal alignment without professional intervention.
How Common is Clubfoot?
Clubfoot is one of the most common congenital musculoskeletal conditions. According to the American Academy of Orthopaedic Surgeons (AAOS), it occurs in approximately 1 in every 1,000 live births. It is twice as common in males as in females. If one child in a family has clubfoot, the risk of a subsequent sibling also having it increases to about 1 in 30, highlighting a genetic component.
Consult a Paediatrician or Orthopaedist for the best advice
Recognising the Signs of Clubfoot
Identifying clubfoot is typically straightforward due to its distinctive appearance. It is often diagnosed prenatally during a routine ultrasound or immediately after birth during the newborn physical exam.
The Classic Physical Appearance
The affected foot has several characteristic features:
- The foot is turned inward and downward.
- The heel is often small and turned inward.
- The calf muscles on the affected leg may be underdeveloped and slightly smaller.
- The foot may appear shorter and wider than a typical foot.
Is Clubfoot Painful for the Baby?
A crucial point of reassurance for parents is that clubfoot itself is not painful for the infant. The baby has been positioned this way in the womb and is accustomed to it. The discomfort associated with clubfoot arises later in life if it is not treated, as walking on the side of the foot can cause painful calluses, arthritis, and an inability to wear normal shoes.
Unraveling the Causes: Why Does Clubfoot Happen?
Despite being a well-known condition, the exact cause of clubfoot is not fully understood. It is considered "idiopathic" in most cases, meaning there is no single identifiable cause. However, research points strongly to a combination of genetic and environmental factors.
The Role of Genetics and Family History
Genetics play a significant role. The condition tends to run in families, and specific gene variations are believed to increase susceptibility. It's not a simple inheritance pattern like eye color, but rather a complex interplay of multiple genes.
Identifying Risk Factors
Certain factors can increase the risk of a baby being born with clubfoot. They are:
- Family History: Having a parent or sibling with clubfoot.
- Sex: Being male.
- Prenatal Environment: Maternal smoking during pregnancy and having insufficient amniotic fluid (oligohydramnios) are considered potential risk factors.
- Other Conditions: Clubfoot can be associated with other neuromuscular conditions like spina bifida (this is known as syndromic clubfoot).
Getting a Diagnosis: What to Expect
Diagnosis is a key step that often begins before birth.
Prenatal Ultrasound Detection
In many cases, clubfoot can be detected during a second-trimester ultrasound, usually around the 20-week mark. While this early news can be worrying for expectant parents, it provides valuable time to learn about the condition, connect with specialists, and understand the treatment plan that will begin shortly after birth.
The Postnatal Physical Examination
After birth, a paediatrician or a paediatric orthopaedic specialist will confirm the diagnosis through a physical examination. They will gently manipulate the foot to assess its flexibility and rule out other conditions, such as positional clubfoot (which is more flexible and often resolves on its own). X-rays are rarely needed for a newborn diagnosis but may be used later to monitor bone alignment during treatment.
The Gold Standard: The Ponseti Method of Treatment
The Ponseti method, developed by Dr. Ignacio Ponseti in the 1950s, has revolutionised clubfoot treatment. It is a gentle, non-surgical technique with a success rate of over 95% when performed correctly and followed by proper bracing. The entire process for clubfoot treatment in newborns typically starts within the first few weeks of life.
Phase 1: Gentle Manipulation and Casting
The first phase involves weekly visits to a trained specialist. They will gently stretch and manipulate the baby's foot toward the correct position. A long-leg plaster cast is then applied from the toes to the upper thigh to hold the correction. This process is repeated weekly for about 4-8 weeks, with each cast gradually improving the foot's alignment.
The Tenotomy Procedure: A Minor but Crucial Step
In over 90% of cases, a minor procedure called a percutaneous Achilles tenotomy is needed. After the casting has corrected the foot's position as much as possible, the tight Achilles tendon is still preventing the heel from coming down. The doctor will make a tiny incision to clip the tendon, allowing it to lengthen naturally. This is a quick procedure, often done with local anesthetic, and casting continues for another 3 weeks to allow the tendon to heal at the proper length.
Phase 2: The Importance of Bracing (The Foot Abduction Brace)
This is the most critical phase for long-term success. Once the foot is fully corrected, the child must wear a foot abduction brace (also called a Denis Browne bar) to prevent relapse. The brace consists of shoes attached to a bar. For the first 3-4 months, the brace is worn 23 hours a day. After that, it is worn during naps and at night (typically 12-14 hours a day) until the child is around 4-5 years old. Adherence to this bracing protocol is essential.
Looking Beyond Ponseti: Other Treatment Options
While the Ponseti method is the global standard, other approaches exist.
The French Functional Method
This method involves daily stretching, taping, and splinting performed by a physical therapist. It requires an immense commitment from parents but can be effective in some cases. It is less commonly used than the Ponseti method due to the high level of daily involvement needed.
When is Clubfoot Surgery Necessary?
Surgery for clubfoot is now reserved for complex cases, feet that do not respond fully to the Ponseti method, or recurrent deformities. Surgical procedures aim to release the tight joints and tendons in the foot. While often successful, surgery can lead to stiffness and arthritis later in life, which is why the non-surgical Ponseti method is preferred as the first line of treatment.
Life After Treatment: Long-Term Outlook and Care
With successful early treatment, the long-term outlook for a child with clubfoot is excellent.
What to Expect as Your Child Grows
Children who complete the Ponseti method and bracing protocol typically have feet that function normally. The treated foot may be slightly smaller and less flexible than the other, and the calf muscle may remain smaller. However, these differences are usually minor and do not impact function. Regular follow-ups with the orthopaedic doctor are important until the child stops growing.
Activities and Sports for Children with Treated Clubfoot
There are virtually no limitations. Children with successfully treated clubfoot can participate in all activities, including running, jumping, and playing sports. Many become accomplished athletes. The goal of treatment is to provide a pain-free, functional, and plantigrade foot (a foot that stands flat on the ground)—and the Ponseti method achieves this for the vast majority.
A Parent's Support Guide: Coping and Finding Resources
Receiving a clubfoot diagnosis can be emotionally challenging. Connecting with other parents through support groups (online or in-person) can be incredibly helpful. Organisations like STEPS worldwide provide valuable resources, information, and a community of families who have navigated the same journey. Remember, you are not alone, and you are your child's best advocate.
Conclusion
A clubfoot diagnosis is the beginning of a manageable medical journey, not a life sentence of limitation. Thanks to the pioneering work of Dr. Ponseti, today's treatments are gentle, effective, and non-invasive. The path requires commitment, especially during the bracing phase, but the reward is seeing your child walk, run, and play without a second thought to their early childhood treatment. By seeking care from a qualified specialist, following the treatment plan diligently, and connecting with a support network, you can ensure your child has every opportunity for a healthy, active future. If your child has been diagnosed, take a deep breath, gather information, and take the first step by connecting with a healthcare professional who can guide you on this well-trodden path to success.
Consult a Paediatrician or Orthopaedist for the best advice
Consult a Paediatrician or Orthopaedist for the best advice

Dr Vikas P Birla
Orthopedics-Sports Medicine
13 Years • MBBS, DNB, MNAMS, Fellowship in Shoulder and Sports Injury
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr Abhishek Nandi
Paediatric Orthopaedician
10 Years • MBBS, M.S. ortho (JIPMER), Fellow Paed Ortho (CMC Vellore), Post- Doctoral Fellow Paed Ortho( MGR U) Speciality- Paediatric fractures, Bone and joint infection, Deformity correction, Bony tumour, Cerebral Palsy, Limb Reconstruction
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata

Dr. Praveen Podali
Orthopaedician
9 Years • MBBS,MS ,Fellowship in joint replacement,Fellowship in arthroscopy and sports medicine
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Preetham Raj Chandran
Orthopaedician
10 Years • MBBS, MS(ORTHO)FIJR(SIAA),FIRJR,FIASM
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Abhey Wasdev
Orthopaedician
12 Years • MBBS, MS - Orthopaedics, FIASM (FRGUHS/ISAKOS), Fellowship in Arthroscopy, Sports Injury, Joint Preservation Surgery and Regenerative Medicine
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
Consult a Paediatrician or Orthopaedist for the best advice

Dr Vikas P Birla
Orthopedics-Sports Medicine
13 Years • MBBS, DNB, MNAMS, Fellowship in Shoulder and Sports Injury
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr Abhishek Nandi
Paediatric Orthopaedician
10 Years • MBBS, M.S. ortho (JIPMER), Fellow Paed Ortho (CMC Vellore), Post- Doctoral Fellow Paed Ortho( MGR U) Speciality- Paediatric fractures, Bone and joint infection, Deformity correction, Bony tumour, Cerebral Palsy, Limb Reconstruction
Kolkata
Apollo Multispeciality Hospitals , Kolkata, Kolkata

Dr. Praveen Podali
Orthopaedician
9 Years • MBBS,MS ,Fellowship in joint replacement,Fellowship in arthroscopy and sports medicine
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Preetham Raj Chandran
Orthopaedician
10 Years • MBBS, MS(ORTHO)FIJR(SIAA),FIRJR,FIASM
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Abhey Wasdev
Orthopaedician
12 Years • MBBS, MS - Orthopaedics, FIASM (FRGUHS/ISAKOS), Fellowship in Arthroscopy, Sports Injury, Joint Preservation Surgery and Regenerative Medicine
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru
Frequently Asked Questions
1. Can clubfoot correct itself without treatment?
No, clubfoot is a rigid deformity that will not correct on its own. Without treatment, it leads to significant walking difficulties and pain later in life. Early intervention is crucial.
2. What is the difference between clubfoot and metatarsus adductus?
Metatarsus adductus is a much more common and less severe condition where only the front part of the foot is turned inward. The heel is in a normal position, and the foot is generally flexible. It often resolves without treatment, unlike true clubfoot.
3. What happens if my child doesn't wear the clubfoot brace as prescribed?
The risk of the clubfoot relapsing (returning) is very high without consistent bracing. Relapsed clubfoot is more challenging to treat and may require additional casting or even surgery. The brace is essential for maintaining the correction achieved through casting.
4. Are there any specific exercises for clubfoot we can do at home?
Your orthopaedic specialist will guide you on any specific stretches. It is generally not recommended for parents to perform aggressive stretching on their own, as it can be counterproductive. The most important 'homework' is consistent brace wear.
5. Will my child be able to wear normal shoes after treatment?
Yes, absolutely. Once the bracing phase is complete, children who have undergone successful treatment can wear regular, off-the-shelf shoes without any problem.