Signs Of Dengue Fever Diagnosis And Prevention
Learn how to recognise dengue fever early, understand diagnostic tests, manage mild cases at home, and prevent mosquito bites. Stay safe with expert guidance and practical tips.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. Vasanthasree Nair MBBS
Last updated on 13th Jan, 2026

Introduction
Dengue fever is a mosquito-borne viral infection that can range from a mild, flu-like illness to a serious, life-threatening condition. With millions of cases reported globally each year, outbreaks are becoming more frequent and widespread, especially in urban and semi-urban areas. Recognizing the early signs of dengue, understanding how diagnosis works, and taking smart prevention steps can make a real difference—for you, your family, and your community.
In this guide, we’ll walk you through the signs and symptoms of dengue fever, how doctors diagnose dengue, and practical steps to prevent mosquito bites and reduce breeding sites around your home. We’ll also cover key warning signs of severe dengue, when to seek medical care, how to care for mild illness at home, and effective prevention strategies supported by public health experts. Throughout, we include insights you won’t always find in standard articles—like how to time your lab tests, a day-by-day “fever timeline,” and simple ways to monitor your health at home. If symptoms persist beyond two weeks or you’re unsure about your diagnosis, consult a doctor online with Apollo 24|7 for further evaluation. For lab tests, Apollo 24|7 also offers convenient home collection services.
What Is Dengue Fever?
Dengue is a viral infection caused by four related viruses (DENV-1 to DENV-4) and spread through the bite of infected Aedes mosquitoes, mainly Aedes aegypti and Aedes albopictus. These mosquitoes prefer to feed during the day—especially early morning and late afternoon—and breed in small quantities of clean, stagnant water. Because dengue has four serotypes, a person can be infected more than once. Secondary infection with a different serotype can carry a higher risk of severe disease due to the way the immune system responds.
Unlike many mosquito-borne diseases, dengue transmission is tightly linked to human behavior and urban infrastructure—small containers like flower pot trays, roof gutters, and discarded caps can become breeding sites. Tackling these micro-habitats can meaningfully lower local mosquito density.
The Dengue Virus (DENV-1 to DENV-4) in Simple Terms
Each serotype triggers immunity to itself, but not to the others. Over a lifetime, multiple infections are possible. This explains why communities can experience repeated outbreaks as different serotypes circulate.
How Dengue Spreads: The Aedes Mosquito
Aedes mosquitoes tend to rest indoors, bite during the day, and fly short distances. That means your immediate surroundings matter most for prevention—home, school, and workplace.
Why Urban and Semi-Urban Settings Are High Risk
High population density, irregular water supply (leading to stored water), and solid waste accumulation create ideal
conditions. Even a bottle cap can hatch larvae within a week under warm conditions.
How Common Is Dengue? Global and Local Picture
Dengue is endemic in more than 100 countries across Asia, the Americas, Africa, and the Western Pacific. Warmer
temperatures, urbanization, and travel have contributed to expanding risk. Seasonal peaks often align with monsoon or
rainy seasons, though transmission can persist beyond.
Recent Outbreaks and Seasonal Trends
- Cases rise during and shortly after rainy seasons when breeding sites are plentiful.
- Some regions report off-season spikes tied to water storage practices, construction activities, or unusual weather patterns.
Who Is Most at Risk
- People living in or traveling to endemic areas.
- Children, older adults, and those with certain chronic conditions may face increased risk of complications.
- Residents of dense urban neighbourhoods with poor waste management.
Communities can anticipate dengue seasons. A pre-season “source reduction sprint”—neighbourhood clean-ups, gutter
clearing, fixing leaks—two to four weeks before rains can blunt the first wave of cases.
Early Symptoms: How to Recognize Dengue
Dengue typically starts abruptly after an incubation period of 4–10 days following a mosquito bite. The most common
early symptom is high fever, often accompanied by severe headache (especially behind the eyes), muscle and joint pain,
nausea, vomiting, and a rash. Many people describe it as “breakbone fever” due to the intense muscle and bone pain.
Mild bleeding (nose, gums) can occur.
Typical Onset and “Fever Timeline”
- Day 0–2: Sudden high fever, severe headache, body aches, fatigue, loss of appetite; sometimes a flushed face or mild
rash. - Day 3–6: Fever may persist; gastrointestinal symptoms (nausea, vomiting, abdominal discomfort) can intensify.
- Day 4–7 (“Critical Phase”): Even if fever drops, watch for warning signs like severe abdominal pain, persistent vomiting, bleeding, lethargy, restlessness, or signs of dehydration.
- Day 7–10 (“Recovery Phase”): Appetite returns, rash may peel or itch, energy gradually improves.
Don’t assume recovery just because the fever subsides around day 4–6. The 24–48 hours after fever falls can be the most critical.
Common Symptoms vs Less Common Ones
Common: High fever, severe headache, retro-orbital pain, myalgia, arthralgia, nausea/vomiting, rash, mild bleeding.
Less Common: Significant liver enlargement, severe lethargy, confusion—these require urgent assessment.
Severe Dengue: Warning Signs You Shouldn’t Ignore
Severe dengue can involve plasma leakage leading to shock, severe bleeding, and organ impairment. It usually develops
around day 3–7 of illness.
Red Flags in Days 3–7 of Illness
- Severe abdominal pain or tenderness
- Persistent vomiting
- Bleeding (nose, gums, black stools) or unusual bruising
- Lethargy, restlessness, or confusion
- Rapid breathing, cold clammy skin, or narrowing pulse pressure
- Decreased urine output or dark urine
When to Seek Urgent Care
If any warning signs appear, go to a hospital immediately. Severe dengue can progress quickly, and timely IV fluids and monitoring can be life-saving.
Home pulse pressure checks can help: if the difference between systolic and diastolic falls below 20–25 mmHg along with symptoms, seek urgent care.
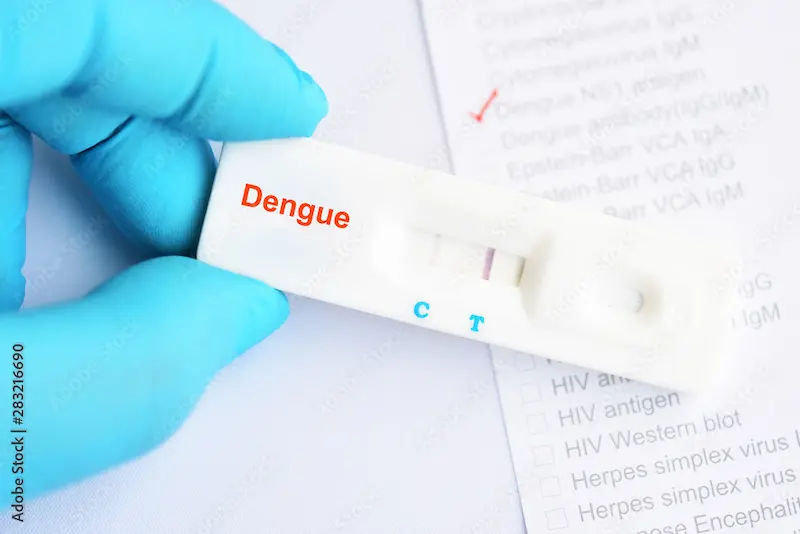
Dengue Diagnosis: Tests, Timing, and Accuracy
Diagnosing dengue relies on a combination of clinical assessment and lab tests. Timing matters greatly for accuracy.
NS1 Antigen and RT–PCR (Early-Phase Tests)
- NS1 antigen test: Most useful within the first 1–5 days of fever.
- RT–PCR: Detects viral RNA, best within days 1–5; can also identify the serotype.
IgM/IgG Antibody Tests (Later-Phase Tests)
- IgM: Detectable around day 4–5 of illness, peaking around week 2.
- IgG: Indicates past infection; high or rising IgG may suggest secondary infection.
How to Time Your Test for Best Results
- Days 1–5: NS1 and/or RT–PCR preferred.
- Day 5 onward: IgM/IgG antibodies more reliable; repeat test if needed.
Keeping a “fever day count” in your phone notes helps your doctor interpret test results correctly. Home collection for dengue tests is available through Apollo 24|7.
Dengue vs Other Fevers: Malaria, Chikungunya, Typhoid, and COVID-19
Key Differences in Symptoms and Timelines
- Chikungunya: Prominent joint pain and swelling, often more severe than dengue; rash possible.
- Malaria: Cyclic fever, chills, sweats, anemia. Malaria testing is essential in endemic areas.
- Typhoid: Prolonged fever, abdominal discomfort, slower onset, relative bradycardia.
- COVID-19: Respiratory symptoms, sore throat, loss of smell/taste; can overlap with dengue.
Why Testing Is Essential
Clinical features overlap; relying on symptoms alone can be misleading. Testing guides correct treatment.
When to See a Doctor—and What to Expect
Seek medical care if you have high fever lasting more than 48 hours, severe headache, persistent vomiting, bleeding, or
recent travel to dengue-prone areas. Clinicians will assess vital signs, hydration status, and may order blood tests.
What Your Clinician Will Check
- Hematocrit: Rising levels can indicate plasma leakage.
- Platelet count: Trending down may correlate with severity but is not the only predictor.
- Liver enzymes: Can be elevated in dengue.
When to Monitor at Home vs Hospital Care
- Home: Mild symptoms, stable vitals, able to drink adequately, no warning signs.
- Hospital: Any warning signs, comorbidities, pregnancy, infants/older adults, inability to maintain hydration, very high hematocrit, or rapidly dropping platelets with symptoms.
Keeping a 24-hour symptom diary helps clinicians track trends and determine care needs.
Caring for Mild Dengue at Home (Safely)
Supportive care is the mainstay for mild dengue.
Hydration, Fever Control, and Rest
- Frequent small sips of fluids (ORS, coconut water, soups); 2–3 liters/day for adults.
- Use paracetamol for fever and pain.
- Rest in a cool, well-ventilated room; avoid strenuous activity.
Medicines to Avoid and Why
- Avoid NSAIDs like ibuprofen, aspirin, and naproxen due to bleeding risk.
- Avoid intramuscular injections unless essential.
Monitor urine colour—aim for pale yellow—and maintain hourly hydration goals.
Complications and Hospital Management
Severe dengue involves plasma leakage, which can lead to shock, fluid accumulation, severe bleeding, and organ
dysfunction.
Capillary Leak, Shock, and Bleeding Risks
Leakage can occur when fever subsides; careful fluid management is critical. Clinicians monitor vitals and hematocrit
trends to guide IV fluids.
Platelet Counts: What They Do and Don’t Tell You
Low platelets are common but not the sole predictor of bleeding. Decisions are based on overall clinical assessment.
Prevention at Home: Mosquito Bite and Breeding Control
Here’s how you can prevent dengue at home:
Repellents, Clothing, and Nets
- Use EPA-approved repellents containing DEET, picaridin, IR3535, or oil of lemon eucalyptus.
- Wear long sleeves and pants; treat clothing with permethrin where approved.
- Use window screens and bed nets, especially for daytime sleepers and infants.
Eliminate Breeding Sites; Checklists That Work
- Weekly routine: Empty/brush containers, clear roof gutters, cover water tanks, discard trash capable of holding water.
- Check plant saucers, AC drip trays, and small hidden pools indoors and outdoors.
Assign a “breeding-spot champion” in the family to audit different areas weekly.
Community and Workplace Measures That Make a Difference
Community action is essential for dengue control.
Source Reduction Drives, Larval Control, and Audits
- Organize monthly clean-up drives; coordinate with local authorities for waste disposal and larviciding.
- Use ovitraps and larval surveys to track hotspots and maintain engagement.
Simple Monitoring Tools You Can Run Locally
- Mobile group chats for reporting standing water and scheduling cleanups.
- Map problem areas like construction sites and abandoned lots; escalate issues to municipal teams.
A 15-minute Friday “dry round” at offices before the weekend reduces breeding over 48–72 hours.
Travel Advice and Vaccines: What to Know Before You Go
Keep these travel advice in mind:
Travel Risk, Outbreak Alerts, and Bite Prevention
- Check outbreak updates; pack repellents and protective clothing.
- Choose accommodations with screens/AC and remain vigilant during daytime.
- Consider travel insurance covering mosquito-borne illnesses.
Vaccine Landscape
- Dengue vaccines are approved in some countries for specific age groups and exposure profiles. Consult a travel medicine specialist for guidance.
- Personal protection and community control remain the primary defenses.
Inform your clinician of any recent travel if fever develops within two weeks of returning.
Myths vs Facts: Getting the Basics Right
Here are some myths and facts:
Common Misconceptions Debunked
- Fever drop does not guarantee safety; the critical phase may start afterward.
- High platelets alone do not mean you are safe; clinical signs and trends matter more.
- Aedes mosquitoes breed in small, clean water containers, not just dirty water.
Evidence-Based Practices
- Apply repellents correctly; reapply as directed.
- Eliminate micro-breeding sites weekly.
- Time diagnostic tests appropriately.
For best effect, apply sunscreen first, then repellent 15–20 minutes later.
Seasonal Preparedness: Your 15-Minute Dengue Checklist
Here’s how to be prepared:
Pre-Monsoon Actions
- Inspect roofs, gutters, and overhead tanks; repair leaks and fit tight lids.
- Declutter balconies and yards; remove unused containers.
Weekly 10-Minute Home Routine
- Empty, scrub, and refill pet bowls and plant trays.
- Check refrigerator and AC drip trays.
- Walk your perimeter after rain to spot new standing water.
Use a shared family calendar for recurring “mosquito audits.”
What to Do After Recovery: Follow-Up and Prevention
Here’s what to do after recovery:
Preventing Repeat Infections
- Continue bite prevention; remember there are four serotypes.
- If you had severe dengue, discuss risk mitigation with your doctor.
Regaining Strength Safely
- Begin light activity once appetite and energy return.
- If fatigue persists beyond 2–3 weeks, consult a doctor online for personalised advice.
Conclusion
Dengue fever is preventable and manageable when you know what to look for and how to act. Recognising early signs—high fever, severe headache, body aches—and understanding the critical window when severe symptoms may develop are essential. Accurate, timely diagnosis depends on the day of illness: NS1 or PCR in the first 1–5 days, IgM/IgG after that. For most people with mild disease, supportive care at home—hydration, rest, and paracetamol—works well, but any red flags require urgent medical attention.
Prevention is powerful. Simple weekly actions to eliminate mosquito breeding sites, combined with daytime bite protection, can dramatically reduce risk at home and in your community. Travelers should use repellents, protective clothing, and choose accommodations that limit mosquito exposure.
If your condition does not improve or you are unsure of next steps, consult a doctor online for personalised guidance. Home sample collection for dengue testing can help you get answers faster. With the right knowledge and consistent habits, you can protect yourself and those around you from dengue.
Consult Top Specialists
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Sougata Kumar
General Practitioner
8 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Arthi S
Family Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Aakash Andgi
General Physician/ Internal Medicine Specialist
9 Years • MBBS MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from Dengue
Frequently Asked Questions
1) How do I know if my fever is dengue or something else?
Dengue often includes high fever with severe headache, eye pain, body aches, and sometimes rash. Because many illnesses overlap, testing is key. Consult a doctor online for a tailored diagnosis plan.
2) When should I take a dengue test for best accuracy?
NS1 or RT–PCR in the first 1–5 days; IgM/IgG after day 5. Repeat if initial results do not match symptoms.
3) Can I treat dengue fever at home?
Mild dengue can be managed with fluids, rest, and paracetamol. Avoid NSAIDs. Seek urgent care if warning signs appear. Consult a doctor online if symptoms persist beyond two weeks.
4) Do platelets always drop in dengue—and should I panic?
Platelets commonly fall, but trends and overall clinical condition matter more than a single reading. Rising hematocrit or severe symptoms are bigger concerns.
5) What’s the best way to prevent dengue at home?
Combine bite prevention (repellents, long sleeves, screens) with weekly source reduction: empty, scrub, cover, and discard containers holding water. A 10-minute weekly routine can significantly reduce Aedes breeding.