Diabetes Mellitus Symptoms & Risks
Learn what diabetes mellitus is, its symptoms, risks, complications, tests, and prevention tips. Clear guidance on when to see a doctor.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Diabetes mellitus affects millions of people around the world and often develops so gradually that many individuals do not realise anything is wrong until symptoms become harder to ignore. Because early signs are subtle, it is easy to dismiss them as tiredness, stress, or a busy schedule. Understanding what to watch for, when to get tested, and how to manage or prevent diabetes can make a meaningful difference to your long-term health. This guide offers clear explanations of the condition, the symptoms to look out for, who might be at higher risk, how diagnosis works, and the practical steps that help support everyday wellbeing.
Consult a Top General Practitioner for Personalised Advice
What is Diabetes Mellitus?
Diabetes is a long-term condition in which the body struggles to use glucose efficiently. Normally, the hormone insulin moves glucose from the bloodstream into the cells that need it for energy. When insulin is not produced as it should be, or when the body becomes less responsive to it, glucose builds up in the blood. Over time, persistently high blood sugar can damage blood vessels and nerves, affecting organs throughout the body.
Main Types of Diabetes Mellitus
• Type 1: An autoimmune condition in which the body destroys the cells that produce insulin. It is often diagnosed in childhood or adolescence but can appear later. People with type 1 need insulin from the time of diagnosis.
• Type 2: The most common type. The body becomes resistant to insulin and may also produce less of it. Lifestyle factors such as excess body weight and physical inactivity influence risk, although genetics also play a role.
• Gestational: A type that develops during pregnancy. It usually resolves after birth but increases the risk of future type 2 diabetes for both mother and baby.
• Prediabetes: A stage where blood sugar is higher than normal but not high enough for diabetes. Without lifestyle action, the progression to type 2 is common.
Symptoms of Diabetes Mellitus
Symptoms vary widely, and type 2 diabetes may cause few problems at first. Many people live with elevated blood sugar for years before diagnosis, making awareness essential.
Common Signs & Symptoms
• Increased thirst and frequent urination
• Heightened hunger that persists even after meals
• Unexplained weight loss, especially in type 1
• Tiredness, lethargy, or low energy
• Blurred or fluctuating vision
• Slow-healing cuts or sores
• Repeated infections such as UTIs, gum infections, or skin infections
• Tingling, numbness, or burning in hands or feet
• Areas of darkened skin, often around the neck or armpits
• Irritability, mood changes, or difficulty concentrating
Some people experience very mild symptoms that come and go. Others may notice only one or two changes that do not seem directly linked to blood sugar. Because of this, routine screening is vital for anyone with risk factors.
Who is At Risk For Diabetes Mellitus?
Many different influences can increase the likelihood of developing diabetes, particularly type 2. Risk increases when several factors are combined.
Key Risk Factors
• Excess weight or obesity, particularly around the waistline
• Low levels of physical activity
• A parent or sibling with diabetes
• Age over 35, although younger adults can develop it too
• History of gestational diabetes or delivering a large baby
• High blood pressure
• Cholesterol concerns, such as low HDL or high triglycerides
• Polycystic ovary syndrome (PCOS)
• Prediabetes
• Conditions linked to insulin resistance, such as sleep apnoea
• Certain ethnic or racial backgrounds
The causes of type 1 are less clearly understood, though genetic tendency combined with environmental triggers is suspected. Autoimmune conditions in the family also raise the risk slightly.
Serious Complications To Look Out For
Diabetes is manageable, especially when caught early, but uncontrolled blood sugar can gradually affect almost every part of the body. Complications may develop silently before symptoms appear, underscoring the value of regular monitoring and consistent treatment.
Possible Complications
• Heart and blood vessel disease, such as heart attack, stroke, and poor circulation
• Kidney disease, ranging from mild decline to kidney failure, over time
• Nerve damage causing pain, tingling, digestive problems, or loss of feeling
• Eye diseases such as diabetic retinopathy, cataracts, and glaucoma
• Foot problems, including ulcers, infections, and (in severe cases) amputations
• Gum disease and other oral health issues
• Problems with sexual function or bladder control
• Skin infections and slow wound healing
• Pregnancy complications for both parent and baby
• Diabetic ketoacidosis, a dangerous emergency more common in type 1
Early action, steady blood sugar control, and planned checkups can significantly reduce the risk of long-term harm.
How is Diabetes Diagnosed?
Diagnosing diabetes involves specific blood tests that measure how much glucose is circulating in the bloodstream. These tests help clinicians distinguish between normal blood sugar, prediabetes, and diabetes. In many cases, a result is confirmed by repeating the test on a separate day unless symptoms are clearly present alongside a very high reading. Understanding these tests can help you feel more prepared when speaking with your healthcare professional.
Common Tests and Thresholds
It includes:
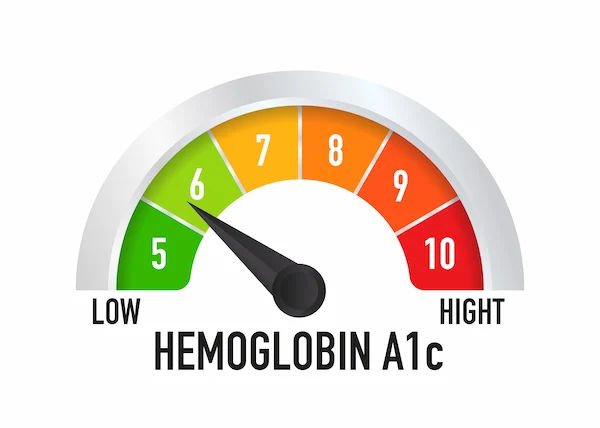
• A1C test (reflects average blood sugar over the previous two to three months)
• Prediabetes: 5.7% to 6.4%
• Diabetes: 6.5% or higher
• Fasting plasma glucose (after at least eight hours without calories)
• Prediabetes: 100 to 125 mg/dL (5.6 to 6.9 mmol/L)
• Diabetes: 126 mg/dL (7.0 mmol/L) or higher
• Oral glucose tolerance test, checking blood sugar two hours after a glucose drink
• Prediabetes: 140 to 199 mg/dL (7.8 to 11.0 mmol/L)
• Diabetes: 200 mg/dL (11.1 mmol/L) or higher
• Random plasma glucose
• Diabetes: 200 mg/dL (11.1 mmol/L) or higher with symptoms
Get Your Symptoms Assessed
When To Get Screened?
Screening is crucial because type 2 diabetes can develop quietly. Early detection allows you to take steps that protect your organs and reduce the risk of complications.
Recommended screening
• Age 35 or older
• At any age, if you are overweight or obese, plus at least one risk factor
• History of gestational diabetes
• Symptoms that suggest high blood sugar
Pregnant individuals are generally screened for gestational diabetes between 24 and 28 weeks, with earlier testing for those at higher risk.
When to Seek Medical Help?
Some symptoms require prompt attention so complications can be prevented or treated early. Knowing when to seek care can be lifesaving, especially for people with suspected type 1 or untreated high blood sugar.
Seek Prompt Medical Care If You Notice
It includes:
• Frequent urination with extreme thirst
• Significant, unexplained weight loss
• Blurry or fluctuating vision
• Slow-healing sores
Urgent Care Signs
Diabetic ketoacidosis develops below signs, which means urgent care is required:
• Nausea, vomiting, or abdominal pain
• Rapid or deep breathing
• Breath with a fruity odour
• Severe fatigue or confusion
• Very high blood glucose plus moderate or high ketones
DKA develops quickly and can be dangerous, especially in type 1 diabetes, so immediate treatment is essential.
Daily Steps To Handle Diabetes Effectively
Living with diabetes involves building habits that support steady blood sugar and overall health. Small actions add up, and the most effective plan is one that suits your lifestyle, preferences, and health needs. Consistency, rather than perfection, makes the biggest difference over time.
Healthy Eating Patterns
• Base meals around vegetables, fruits, whole grains, beans, lentils, nuts, seeds, lean meats, poultry, fish, and dairy if tolerated.
• Choose high-fibre carbohydrates; they digest more slowly and help maintain steadier blood sugar.
• Limit refined grains and added sugars.
• Include healthy fats such as olive oil, avocado, nuts, and seeds.
• Spread carbohydrate intake throughout the day to avoid large spikes.
• If you drink alcohol, enjoy it with food and check with your clinician to ensure it is safe for you.
Physical Activity
• Aim for at least 150 minutes of moderate-intensity aerobic exercise each week, such as brisk walking, cycling, dancing, or swimming.
• Include muscle-strengthening exercises at least two days a week.
• Break up long periods of sitting by standing or taking short movement breaks.
Weight Management
• Losing 5 to 10 per cent of your body weight can improve blood sugar, cholesterol, and blood pressure.
• Structured lifestyle programmes have been shown to significantly reduce the progression from prediabetes to type 2 diabetes.
Medications and Monitoring
• Your plan may include metformin, insulin, or other diabetes medications such as SGLT2 inhibitors or GLP-1 receptor agonists.
• Check your blood glucose as advised, using either finger-prick testing or a continuous glucose monitor if recommended.
• Manage blood pressure and cholesterol carefully because these factors play a major role in long-term complications.
Preventive Care
• Regular A1C tests and kidney checks help track your progress.
• Annual dilated eye exams look for early signs of retinopathy.
• Foot checks, both at home and in the clinic, reduce the risk of ulcers.
• Stay up to date with recommended vaccines to support immune health.
• If you smoke, seek help to quit because smoking significantly increases complications.
Stress, Sleep and Support
• Aim for seven to nine hours of good-quality sleep each night.
• Use relaxation strategies, social support, or counselling to manage stress.
• Diabetes education programmes offer practical skills that build confidence.
Prevention Tips for Prediabetes
Prediabetes is a crucial window of opportunity. Making lifestyle changes at this stage can often reverse or greatly improve blood sugar levels, reducing the chance of developing type 2 diabetes.
Effective Prevention Steps
Effective prevention tips include:
• Move more each week, working towards the 150-minute activity target.
• Choose a diet rich in whole foods, fibre, and minimal added sugar.
• If you carry excess weight, aim for a 5 to 7 per cent weight reduction.
• Consider joining a structured lifestyle or diabetes prevention programme.
• Keep up with regular checkups to monitor progress and adjust your plan.
Conclusion
Understanding diabetes empowers you to take meaningful steps towards protecting your long-term health. Recognising early symptoms, knowing your personal risk factors, and seeking timely screening all contribute to early diagnosis and effective management. Whether you are living with diabetes or aiming to prevent it, consistent lifestyle habits such as nutritious eating, regular movement, weight management, and routine medical care play a central role. With steady attention and the right support, many people find they can live well with diabetes while reducing the risk of serious complications. For personalised guidance, always work closely with your healthcare professional.
Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Md Yusuf Shareef
General Practitioner
8 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr Aswathy D C
General Practitioner
6 Years • MBBS
Bangalore
Apollo Clinic Bellandur, Bangalore
Consult a Top General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Md Yusuf Shareef
General Practitioner
8 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr Aswathy D C
General Practitioner
6 Years • MBBS
Bangalore
Apollo Clinic Bellandur, Bangalore
More articles from Diabetes
Frequently Asked Questions
1) What’s the difference between type 1 and type 2 diabetes?
Type 1 is an autoimmune condition where the body stops making insulin, which means insulin therapy becomes essential from the outset. Type 2 develops when the body struggles to use insulin effectively and may not produce enough. It is often connected with excess weight and low physical activity, although other factors contribute too. Many people with type 2 manage their condition with a combination of lifestyle changes and medication, though some eventually need insulin as well.
2) Can diabetes be cured?
Type 1 cannot be cured because the body no longer produces insulin. Type 2 does not have a cure either, but it can sometimes go into remission, particularly when significant weight loss or sustained lifestyle changes improve insulin sensitivity. Even in remission, regular monitoring is still necessary because blood sugar levels can rise again over time.
3) What are normal blood sugar levels?
Targets differ depending on your health, age, and recommendations from your clinician. Generally, a fasting level below 100 mg/dL (5.6 mmol/L) and a two-hour after-meal level below 140 mg/dL (7.8 mmol/L) are considered typical for people without diabetes. If you have diabetes or prediabetes, your clinician will set personalised targets that align with your goals and overall health.
4) Is prediabetes reversible?
Prediabetes can often be reversed or improved with consistent lifestyle changes. Weight loss of 5 to 7 percent and at least 150 minutes of moderate activity per week have been shown to significantly reduce the likelihood of progressing to type 2 diabetes. Early action is particularly effective because the body may still be responsive to insulin.
5) Which diet is best for diabetes?
There is no single diet that suits everyone, but eating patterns such as the Mediterranean-style and DASH approaches are well supported. These emphasise vegetables, whole grains, lean proteins, legumes, nuts, and healthy fats. Working with a registered dietitian or diabetes educator can help tailor your meals to your preferences, medication plan, and glucose goals.