Average Age Of Menopause After Hysterectomy
Learn how a hysterectomy affects the timing and symptoms of menopause, depending on whether the ovaries are removed, and how to manage the transition effectively.

Written by Dr.Sonia Bhatt
Last updated on 8th Jul, 2025

Introduction
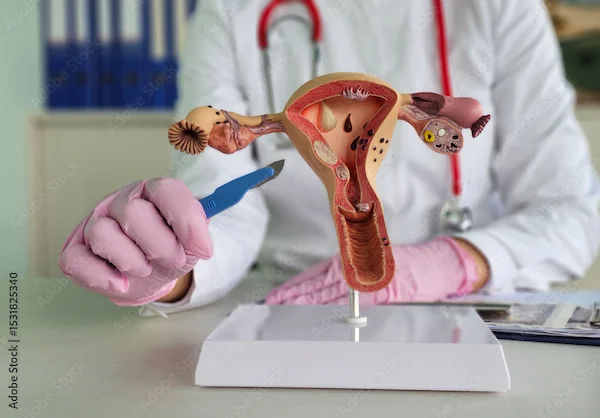
Menopause is a natural phase in a woman’s life when her menstrual cycles stop permanently, marking the end of her reproductive years. However, for women who undergo a hysterectomy (surgical removal of the uterus), menopause can occur differently. If you’ve had a hysterectomy or are considering one, it’s important to understand how this procedure affects menopause and what you can expect.
What Happens to Menopause After a Hysterectomy?
A hysterectomy involves the removal of the uterus, and sometimes the ovaries as well. The impact on menopause depends on whether the ovaries are removed during the procedure:
Hysterectomy with Ovaries Removed (Oophorectomy)
If both ovaries are removed (bilateral oophorectomy), menopause begins immediately, regardless of age. This is called surgical menopause.
Symptoms like hot flashes, mood swings, and vaginal dryness may appear suddenly and can be more intense than natural menopause.
Hysterectomy Without Ovaries Removed
If the ovaries remain, they continue producing hormones, and natural menopause will occur at the usual age (average around 51 years).
However, some women may experience menopause 1–2 years earlier than expected because the blood supply to the ovaries may be affected during surgery.
Consult Top Gynaecologists For More Information
Why Does Menopause Timing Change After Hysterectomy?
Ovarian Function Decline: Even if ovaries are preserved, their function may decline slightly faster due to reduced blood flow after surgery.
Hormonal Shifts: The uterus plays a role in hormone regulation, and its removal can subtly affect ovarian function.
Symptoms of Menopause After Hysterectomy
If you experience surgical menopause (ovaries removed), symptoms may be more severe and sudden. Common signs include:
Hot flashes and night sweats
Mood swings, anxiety, or depression
Vaginal dryness and discomfort
Sleep disturbances
Decreased libido
Bone density loss (higher risk of osteoporosis)
If your ovaries remain, symptoms may develop gradually, similar to natural menopause.
Managing Menopause After Hysterectomy
Here’s how you can manage menopause after a hysterectomy:
1. Hormone Replacement Therapy (HRT)
If you’ve had both ovaries removed, your doctor may recommend HRT to replace estrogen and progesterone, reducing symptoms and protecting bone health.
Discuss risks and benefits with your doctor, especially if you have a history of breast cancer or blood clots.
2. Lifestyle Adjustments
Diet: Include calcium-rich foods such as dairy, leafy greens, and vitamin D sources like fortified foods and sunlight exposure.
Exercise: Weight-bearing exercises such as walking and yoga help maintain bone density and support mood stability.
Stress Management: Meditation, deep breathing, and relaxation techniques can help ease emotional symptoms.
3. Vaginal Health
Use water-based lubricants or vaginal moisturizers if dryness causes discomfort.
Low-dose vaginal estrogen creams may help if recommended by your doctor.
4. Regular Health Check-ups
Monitor bone density using DEXA scans, especially if you are at risk for osteoporosis.
Keep up with heart health screenings, as menopause increases cardiovascular risks.
When to See a Doctor
Consult a healthcare provider if:
Symptoms are severe and interfere with daily life
You experience unexpected bleeding (if your cervix was retained)
You have concerns about bone or heart health after hysterectomy
Conclusion
A hysterectomy can influence when and how menopause occurs, but with the right care, symptoms can be managed effectively. Whether you’ve had your ovaries removed or not, staying informed and working closely with your doctor will help you navigate this transition smoothly.
If you have concerns about menopause after a hysterectomy, consider booking a consultation with a specialist through Apollo 24|7 for personalised guidance.
Consult Top Gynaecologists
Consult Top Gynaecologists For More Information

Dr. Abhishek Daga
Obstetrician and Gynaecologist
20 Years • MBBS, MS (Obstetrics & Gynaecology)
Kolkata
Gynae Care Fertility Centre, Kolkata
(150+ Patients)

Dr. Ramya G S
Obstetrician and Gynaecologist
11 Years • MBBS, DGO - Obstetrics & Gynaecology, DNB - Obstetrics & Gynaecology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Mehnaz Rashid
Obstetrician and Gynaecologist
7 Years • MBBS, DNB (Obstetrics & Gynaecology), D.MAS, F.MAS, WALS
Bengaluru
Wellstar Polyclinic and Diagnostic Center, Bengaluru
(225+ Patients)

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata
Consult Top Gynaecologists

Dr. Abhishek Daga
Obstetrician and Gynaecologist
20 Years • MBBS, MS (Obstetrics & Gynaecology)
Kolkata
Gynae Care Fertility Centre, Kolkata
(150+ Patients)

Dr. Ramya G S
Obstetrician and Gynaecologist
11 Years • MBBS, DGO - Obstetrics & Gynaecology, DNB - Obstetrics & Gynaecology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Mehnaz Rashid
Obstetrician and Gynaecologist
7 Years • MBBS, DNB (Obstetrics & Gynaecology), D.MAS, F.MAS, WALS
Bengaluru
Wellstar Polyclinic and Diagnostic Center, Bengaluru
(225+ Patients)

Dr. Sreeparna Roy
Obstetrician and Gynaecologist
8 Years • MBBS , MS (OBSTETRICS & GYNAECOLOGY), Fellowship in Infertility, Endoscopy & Ultrasonography), Fellowship in Laparoscopy & Hysteroscopy,DRM
Kolkata
Dr Utsa Basu Clinic, Kolkata