Endometriosis After Menopause A Guide for Older Women
Know about endometriosis, a common presence in elderly women, its symptoms, diagnosis and treatment management. Learn about how to live with endometriosis and more.

Written by Dr. Siri Nallapu
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
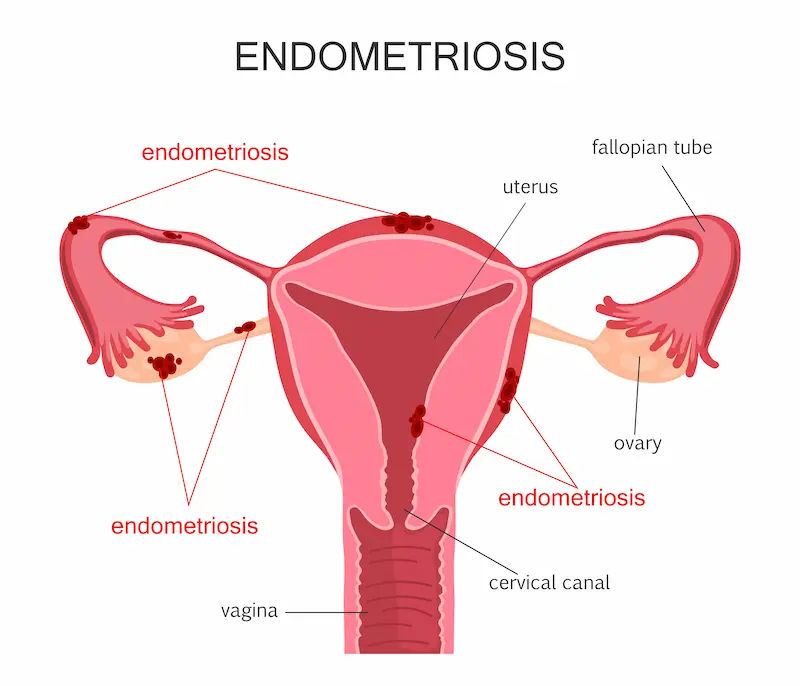
Endometriosis is often perceived as a condition that exclusively affects women during their reproductive years, typically subsiding after menopause. However, for a significant number of women, the reality is different. Endometriosis in elderly women is a challenging and frequently overlooked health issue. This guide aims to shed light on this under-discussed topic, providing clarity and support for those who may be experiencing symptoms later in life. While it's true that the natural decline of estrogen during menopause can cause endometrial lesions to shrink, some women continue to suffer from pain and other symptoms. Understanding the unique presentation, causes, and management strategies is crucial for maintaining quality of life. This article will explore the signs to watch for, the diagnostic hurdles, and the tailored treatment options available for older women navigating this complex condition.
Is Endometriosis Common in Elderly Women?
The short answer is no, it is not common, but it is certainly possible and more prevalent than previously thought. The prevailing medical belief was that endometriosis was dependent on cyclical estrogen and would therefore regress after menopause. While this is true for many, studies indicate that between 2% and 5% of postmenopausal women continue to experience symptoms or are diagnosed anew. This persistence or late onset occurs due to several factors, primarily related to ongoing estrogen exposure.
For women who have battled endometriosis throughout their lives, reaching menopause can bring welcome relief. However, a subset of this group may find their symptoms persist, especially if they are using hormone replacement therapy (HRT) to manage menopausal symptoms. Furthermore, the diagnosis of endometriosis in women over 60 can be complicated because symptoms are often mistaken for other age-related conditions like irritable bowel syndrome (IBS), diverticulitis, or even cancer. This highlights the importance of considering endometriosis as a potential cause of chronic pelvic pain, regardless of age.
Consult a Top Gynaecologist for Personalised Advice
Recognising the Signs: Symptoms of Endometriosis in Older Women
The signs, symptoms of endometriosis include:
Classic Endometriosis Symptoms That May Persist
Many of the symptoms of endometriosis after menopause mirror those experienced by younger women, though their intensity may vary. These include:
1. Chronic Pelvic Pain: A persistent, often dull ache that may not be cyclical.
2. Painful Intercourse (Dyspareunia): This can occur due to scarring and inflammation in the pelvis.
3. Painful Bowel Movements or Urination: Especially during periods of flare-ups.
4. Fatigue and General Malaise: The body's chronic inflammatory response can lead to significant tiredness.
Symptoms Often Mistaken for Other Age-Related Conditions
This is where diagnosis becomes tricky. Elderly women may present with symptoms that lead doctors down the wrong path.
1. Gastrointestinal Distress: Bloating, constipation, diarrhoea, and abdominal cramping are easily attributed to IBS or diverticular disease.
2. Urinary Issues: Frequency, urgency, or pain can be misdiagnosed as recurrent urinary tract infections or interstitial cystitis.
3. Pelvic Pressure or Fullness: This is a common symptom that can be confused with pelvic organ prolapse, a more typical condition in older age.
4. Postmenopausal Bleeding: While any postmenopausal bleeding requires immediate medical attention to rule out cancer, it can sometimes be linked to endometrial tissue in the cervix or vagina.
A unique insight here is that the pain may be less "cyclic" and more constant, reflecting the chronic, inflammatory nature of the disease in the absence of a regular menstrual cycle.
Why Does Endometriosis Occur or Recur After Menopause?
The endometriosis occurs after menopause for below scenarios:
The Role of Hormone Replacement Therapy (HRT)
One of the primary drivers of persistent postmenopausal endometriosis is HRT. Many women use estrogen-based therapy to alleviate severe menopausal symptoms like hot flashes and bone loss. However, this supplemental estrogen can "feed" any remaining endometrial implants, causing them to remain active and symptomatic. The type of HRT matters significantly; regimens that include a progestogen (synthetic progesterone) along with estrogen are generally considered safer for women with a history of endometriosis, as progestogen can counteract estrogen's growth-stimulating effects.
Natural Estrogen Production in Postmenopausal Women
Even without HRT, the body does not completely stop producing estrogen. After menopause, the ovaries cease production, but adipose (fat) tissue continues to produce small amounts of estrogen through the conversion of androgens. In women with higher body fat percentages, this endogenous production can be sufficient to sustain endometriosis lesions. Additionally, certain lesions can produce their own estrogen, creating a local inflammatory environment that is self-perpetuating.
The Diagnostic Challenge: Identifying Endometriosis in the Elderly
Why Diagnosis is Often Delayed or Missed
The diagnosis of endometriosis in an older woman is frequently delayed due to a phenomenon called "diagnostic overshadowing." This occurs when symptoms are automatically attributed to more common conditions in that age group. A complaint of abdominal pain in a 70-year-old is more likely to be investigated for gastrointestinal or oncological causes first. Furthermore, many women themselves may not suspect endometriosis, believing it to be a problem of their past.
Essential Diagnostic Tools and Procedures
The diagnostic process is similar to that for younger women but requires a careful approach.
1. Detailed Patient History: A doctor should take a thorough history, including any past symptoms or diagnosis of endometriosis.
2. Pelvic Exam: This can reveal nodules, tenderness, or scarring.
3. Imaging: Transvaginal ultrasound is the first-line imaging tool. MRI can provide more detailed information about the extent of deep-infiltrating endometriosis.
4. Laparoscopy: This minimally invasive surgery remains the gold standard for a definitive diagnosis. It allows a surgeon to visually confirm the presence of endometrial lesions and, if possible, take a biopsy.
If you are experiencing persistent pelvic pain or other concerning symptoms, it's crucial to consult a specialist. You can book a consultation with an experienced gynaecologist online with Apollo24|7 to discuss your symptoms and review your history in detail.
Treatment and Management Strategies for Elderly Women
Treatment must be highly individualised, considering overall health, comorbidities, and personal preferences. The goal is to manage symptoms and improve quality of life with the least invasive approach possible.
Conservative Management and Pain Relief
For mild symptoms, a conservative approach is often preferred.
1. Pain Management: Over-the-counter NSAIDs (e.g., ibuprofen) can help with pain and inflammation, but their long-term use must be monitored in older adults due to risks to the kidneys and the gastrointestinal tract.
2. Physical Therapy: Pelvic floor physical therapy can be incredibly beneficial in relieving pelvic pain and discomfort caused by muscle tension and scarring.
Surgical Options: Reconsidering Hysterectomy and Excision
Surgery may be recommended if symptoms are severe or if there's a suspicion of malignancy.
1. Laparoscopic Excision: This is the preferred surgical method, involving the careful cutting out of endometriosis lesions while preserving healthy tissue.
2. Hysterectomy with Bilateral Salpingo-oophorectomy (BSO): Removal of the uterus, ovaries, and fallopian tubes. This is a definitive treatment as it removes the primary source of estrogen. However, it is a major surgery, and the decision must be weighed against surgical risks in an older patient.
The Critical Role of Hormone Management
This is a delicate balancing act. If a woman is on HRT and experiencing a recurrence of symptoms, the first step is often to re-evaluate the HRT regimen. Switching to a lower dose or a continuous combined (estrogen + progestogen) therapy may help. In some cases, discontinuing HRT may be necessary, but this decision should be made collaboratively with a doctor, considering the benefits of HRT for bone and heart health. Apollo24|7 offers convenient home collection for tests like bone density markers (Vitamin D, Calcium) or HbA1c to help monitor overall health while managing hormone therapy.
Living Well with Endometriosis Later in Life
It includes:
Lifestyle Modifications for Pain and Wellness
While not a cure, lifestyle changes can significantly impact symptom severity.
1. Anti-inflammatory Diet: Focusing on whole foods, omega-3 fatty acids (found in fish), and reducing processed foods and sugar can help manage inflammation.
2. Gentle Exercise: Activities like walking, swimming, or yoga can improve circulation, reduce stress, and help manage pain.
3. Stress Management: Techniques such as meditation, deep breathing, or mindfulness can help modulate the body's pain response.
The Importance of Mental and Emotional Health
Chronic pain can be isolating at any age. For elderly women, who may also be dealing with other health issues or life changes, the emotional toll can be significant. Seeking support from friends, family, or a therapist who understands chronic illness is vital. Connecting with support groups, even online, can provide validation and reduce feelings of loneliness.
Conclusion
Navigating endometriosis in elderly women requires a shift in perspective—both for patients and healthcare providers. Dismissing pelvic pain as an inevitable part of ageing or immediately attributing it to more common conditions can leave women suffering needlessly. This guide underscores that endometriosis is a possible diagnosis after menopause, and recognising its unique presentation is the first step toward effective management. By understanding the causes, advocating for a thorough diagnostic process, and exploring tailored treatment options, women can reclaim their comfort and well-being. If you suspect your symptoms may be related to endometriosis, do not hesitate to seek a second opinion from a gynaecologist familiar with the condition. Your health and quality of life are paramount at every stage of life.
Consult a Top Gynaecologist for Personalised Advice
Consult a Top Gynaecologist for Personalised Advice
Dr. K Anusha
Obstetrician and Gynaecologist
4 Years • MBBS, DGO
Yemmiganur
SRINIVASAA HOSPITAL, Yemmiganur

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)

Dr. Asha Rani Singh
Obstetrician and Gynaecologist
24 Years • MBBS DGO
Delhi
Dr Asha Rani Singh Clinic, Delhi
Consult a Top Gynaecologist for Personalised Advice
Dr. K Anusha
Obstetrician and Gynaecologist
4 Years • MBBS, DGO
Yemmiganur
SRINIVASAA HOSPITAL, Yemmiganur

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Parul Sharma
Obstetrician and Gynaecologist
8 Years • MBBS, MS (Obstetrics & Gynaecology)
New Delhi
THE DOCTORS NESST, New Delhi

Dr. Debajyoti Goswami
Obstetrician and Gynaecologist
10 Years • MBBS,D.G.O(DNB),Adv. Infertility Tech.(AIIMS),Fellowship in Diabetes(U.K),Comprehensive Abortion Care(Govt. Of W.B), Certificate in Clinical Embryology(AIIMS, BHUBANESWAR)
Bankura
D.G Clinic, Bankura
(25+ Patients)

Dr. Asha Rani Singh
Obstetrician and Gynaecologist
24 Years • MBBS DGO
Delhi
Dr Asha Rani Singh Clinic, Delhi
More articles from Endometriosis
Frequently Asked Questions
1. Can endometriosis turn into cancer in older women?
A.While endometriosis itself is benign, it is associated with a slightly increased risk of certain types of ovarian cancer, specifically endometrioid and clear cell carcinomas. However, the absolute risk remains low. Any new or worsening symptoms, such as a rapidly growing pelvic mass or postmenopausal bleeding, should be promptly evaluated by a doctor to rule out malignancy.
2. I've never had endometriosis. Can it develop for the first time after menopause?
A.Yes, although it is rare. Most cases of postmenopausal endometriosis are recurrences, but a first-time diagnosis can happen. This is often linked to hormone replacement therapy or the body's own estrogen production from fat tissue.
3. What are the risks of surgery for endometriosis in an elderly patient?
A.Risks are higher than for younger patients and include reactions to anaesthesia, infection, bleeding, blood clots, and damage to surrounding organs. Recovery may also be slower. A surgeon will conduct a thorough pre-operative assessment of your heart, lungs, and overall health to determine if the benefits of surgery outweigh the risks.
4. If I stop my HRT, will my endometriosis pain go away?
A.It is very likely to improve or resolve completely, as endometriosis tissue typically thrives on estrogen. However, discontinuing HRT should be a decision made with your doctor, as it may lead to a return of menopausal symptoms like hot flashes and can impact bone density.
5. Are there any non-hormonal medications for managing postmenopausal endometriosis?
There are no specific non-hormonal drugs that target endometriosis. Management focuses on pain relief with NSAIDs (with caution) and addressing inflammation through lifestyle changes. Aromatase inhibitors are a powerful class of drugs that block estrogen production throughout the body and are sometimes used in severe, refractory cases, but they have significant side effects and are not a first-line treatment.