Epilepsy: Types, Symptoms, and Risk Factor
Learn about epilepsy, including its different types, common symptoms, and key risk factors to better understand and manage the condition.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Epilepsy is more than just seizures; it's a complex neurological disorder characterised by a tendency to have recurrent, unprovoked seizures. Affecting millions worldwide, it manifests in countless ways, making understanding its types and risk factors crucial for patients, caregivers, and the general public. This guide demystifies epilepsy, breaking down the different seizure classifications from focal onset to generalised events and exploring the various syndromes that doctors diagnose. More importantly, we delve into the key factors that can increase an individual's likelihood of developing epilepsy, including age, genetics, and past brain injuries. Whether you're seeking information for yourself or a loved one, this article provides a comprehensive overview to empower you with knowledge and guide your next steps.
The Many Faces of Seizures: A Guide to Epilepsy Types
The International League Against Epilepsy (ILAE) classifies seizures based on where they begin in the brain. This is the primary way doctors categorise and diagnose types of epileptic events. Understanding this classification is the first step toward proper management
1. Focal Onset Seizures: Starting in One Brain Area
Formerly known as partial seizures, these start in just one hemisphere of the brain. The experience depends entirely on the specific part of the brain affected.
Focal Aware Seizures (Simple Partial): The person remains fully conscious and aware during the event. Symptoms of a focal seizure can include sudden jerky movements of one body part, experiencing unusual smells or tastes, a rising feeling in the stomach, or intense feelings of déjà vu or fear.
Focal Impaired Awareness Seizures (Complex Partial): These affect a larger area of the brain, leading to a loss of consciousness or awareness. The person may stare blankly, perform repetitive movements like lip-smacking or fumbling with clothes (automatisms), and will not respond normally to their environment.
Focal to Bilateral Tonic-Clonic Seizures: This occurs when a focal seizure spreads to both sides of the brain, evolving into a convulsive seizure. This is what many people traditionally recognise as a grand mal episode.
2. Generalised Onset Seizures: Widespread Brain Involvement
These seizures engage both sides of the brain from the very beginning. There is no "warning" or focal start, and consciousness is almost always impaired.
Absence Seizures (Petit Mal): Common in children, these involve brief lapses in awareness that look like a person is staring blankly into space for a few seconds. They can occur many times a day and may be mistaken for daydreaming.
Tonic-Clonic Seizures (Grand Mal): These are the most dramatic and well-known types of seizures. The "tonic" phase involves muscle stiffening and a fall, while the "clonic" phase features rhythmic jerking. Breathing may be impaired, and the person is often confused and fatigued afterward.
Myoclonic, Atonic, and Tonic Seizures: Myoclonic seizures appear as quick, sudden jerks like a twitch. Atonic seizures ("drop attacks") cause a sudden loss of muscle tone, leading to collapses. Tonic seizures involve sudden stiffening of the body without the jerking phase
3. Unknown Onset Seizures
Sometimes, there isn't enough information for doctors to determine where the seizure began. These are classified as unknown onset but may be reclassified later.
Consult a Neurologist for the best advice
Beyond Seizures: Recognising Common Epilepsy Syndromes
An epilepsy syndrome is a disorder defined by a cluster of features, including seizure type, age of onset, EEG findings, and more.
Childhood Absence Epilepsy
This syndrome appears in otherwise healthy school-aged children and is characterised by frequent absence seizures. It has a strong genetic component.
Juvenile Myoclonic Epilepsy
This common syndrome begins in adolescence. Individuals experience myoclonic jerks (especially in the morning), absence seizures, and tonic-clonic seizures. It is often lifelong but usually manageable with medication.
Lennox-Gastaut Syndrome
A severe childhood-onset syndrome involving multiple types of seizures (including tonic, atonic, and atypical absence), cognitive impairment, and specific EEG patterns. It is often resistant to medication.
Unique Insight: Many people don't realise that a "seizure" is just a symptom, while "epilepsy" is the underlying disease (a tendency to have recurrent seizures). Furthermore, the classification system is dynamic. A diagnosis can change as more information becomes available, emphasising the need for continuous monitoring by a specialist.
What Increases the Risk? Key Epilepsy Risk Factors
Understanding the risk factors for epilepsy helps in identifying potential causes and, in some cases, implementing preventive measures. These factors are generally divided into two categories
Non-Modifiable Risk Factors: Age, Genetics, and Family History
Certain factors are beyond our control. The incidence of epilepsy is highest in young children and older adults. Genetics play a significant role; having a close relative with epilepsy increases one's risk. Specific genes are linked to certain syndromes, like Juvenile Myoclonic Epilepsy. Developmental disorders such as autism and neurofibromatosis are also associated with a higher risk of seizures.
Acquired and Modifiable Risk Factors: Brain Injuries and Lifestyle
These are factors that occur throughout a person's life.
Head Trauma: Severe head injuries are a leading cause of acquired epilepsy. Using seatbelts and helmets can mitigate this risk.
Brain Conditions: Strokes, brain tumors, and infections like meningitis or encephalitis can cause scarring that leads to seizures.
Prenatal Injuries: Brain damage before birth due to oxygen deficiency, infection, or poor nutrition is a common cause of epilepsy in adults that actually originated in childhood.
Lifestyle Triggers (for those with epilepsy): While not direct causes, sleep deprivation, extreme stress, flashing lights (photosensitivity), and alcohol or drug use can lower the seizure threshold and trigger events in diagnosed individuals.
If you or a loved one has experienced a significant head injury or a suspected seizure, it is crucial to consult a neurologist for evaluation.
Conclusion: Empowerment Through Knowledge
Understanding the diverse types of seizures and the underlying risk factors for epilepsy is the cornerstone of effective management and empathy. This neurological disorder is not a monolith; it presents uniquely in every individual. Recognising the difference between a focal aware seizure and an absence seizure, or understanding the genetic factors at play, can demystify the condition and reduce stigma.
Knowledge empowers patients to have informed discussions with their doctors and helps caregivers provide better support. While some risks are inherent, a focus on brain safety through helmets, safe driving practices, and managing cardiovascular health can contribute to prevention. If you suspect you or a loved one is experiencing seizures, the most critical step is to seek a professional evaluation. Modern medicine offers a range of effective treatments that allow most people with epilepsy to lead full, active lives. Your journey begins with understanding.
Consult a Neurologist for the best advice
Consult a Neurologist for the best advice

Dr Debnath Dwaipayan
Neurosurgeon
9 Years • MBBS, MS(Gen. Surgery), DrNB (Neurosurgery)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Shanmugasundaram K
Neurologist
25 Years • MBBS, MD (GENMED), DCH, DM (NEURO)
Chennai
Apollo Speciality Hospitals OMR, Chennai
(25+ Patients)

Dr. Uddalak Chakraborty
Neurologist
8 Years • MBBS, MD(GENL.MED.),DM(NEUROLOGY)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr. Ganeshgouda Majigoudra
Neurologist
10 Years • MBBS, MD ( GENERAL MEDICINE) DM (NEUROLOGY)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Avinash Gupta
Neurologist
12 Years • MBBS, DNB - Neurology
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)
More articles from Epilepsy
Frequently Asked Questions
1. Can you develop epilepsy later in life?
2. Is epilepsy hereditary?
Genetics play a significant role as a risk factor. Having a first-degree relative with epilepsy increases your risk. However, for most people with epilepsy, there is no strong family history, indicating other factors like injury or infection are the cause.
3. What is the difference between a seizure and epilepsy?
A seizure is a single event of abnormal electrical activity in the brain. Epilepsy is a chronic neurological disorder diagnosed after a person has had two or more unprovoked seizures separated by at least 24 hours.
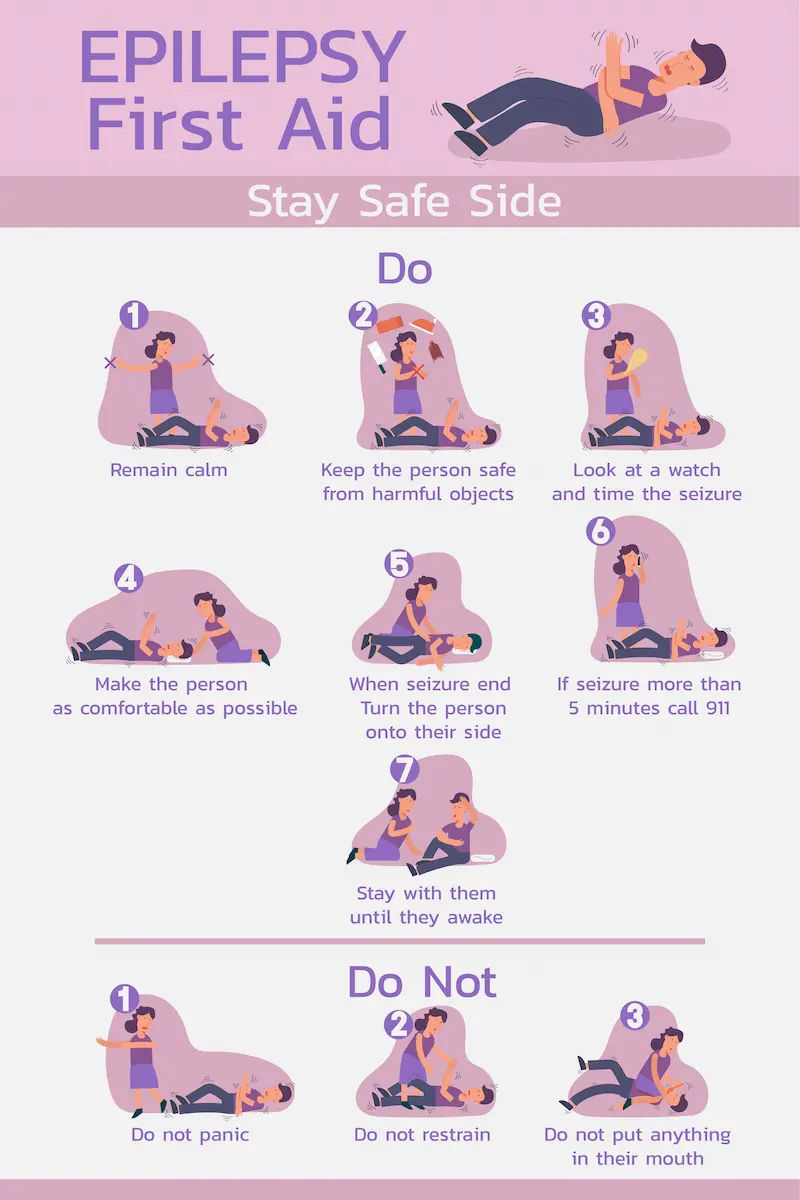
4. What should I do if someone has a tonic-clonic (convulsive) seizure?
Stay calm. Gently lower them to the floor, clear the area of hard objects, and place something soft under their head. Turn them onto their side to help keep their airway clear. Time the seizure. Do not hold them down or put anything in their mouth. Call for emergency medical help if the seizure lasts longer than 5 minutes.
5. Are all seizures dramatic and involve convulsions?
No, this is a common misconception. Many types of seizures, like focal aware or absence seizures, are subtle and may involve only a brief lapse in awareness, a strange feeling, or a small muscle jerk, and can easily go unnoticed.