Fatty Liver Disease: Your Essential Guide to Causes & Reversal
A concise guide to fatty liver disease. Understand what it is, its causes, symptoms, and treatment options. Learn how to prevent and manage this common condition.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Imagine your liver, your body's hardworking detox center, slowly becoming saturated with fat. This isn't a rare phenomenon; it's the reality for nearly 2530% of people globally, a condition known as fatty liver disease. Often silent until it reaches advanced stages, it has become one of the most common causes of chronic liver disease. But here's the crucial, hopeful part: fatty liver disease is largely preventable and, in its early stages, reversible. This guide will demystify this condition for you. We'll break down what it is, why it happens, how to spot the signs, and most importantly, the practical steps you can take to reclaim your liver health. Whether you're newly diagnosed, at risk, or simply health conscious, this is your roadmap to understanding and overcoming fatty liver disease.
What is Fatty Liver Disease, Really?
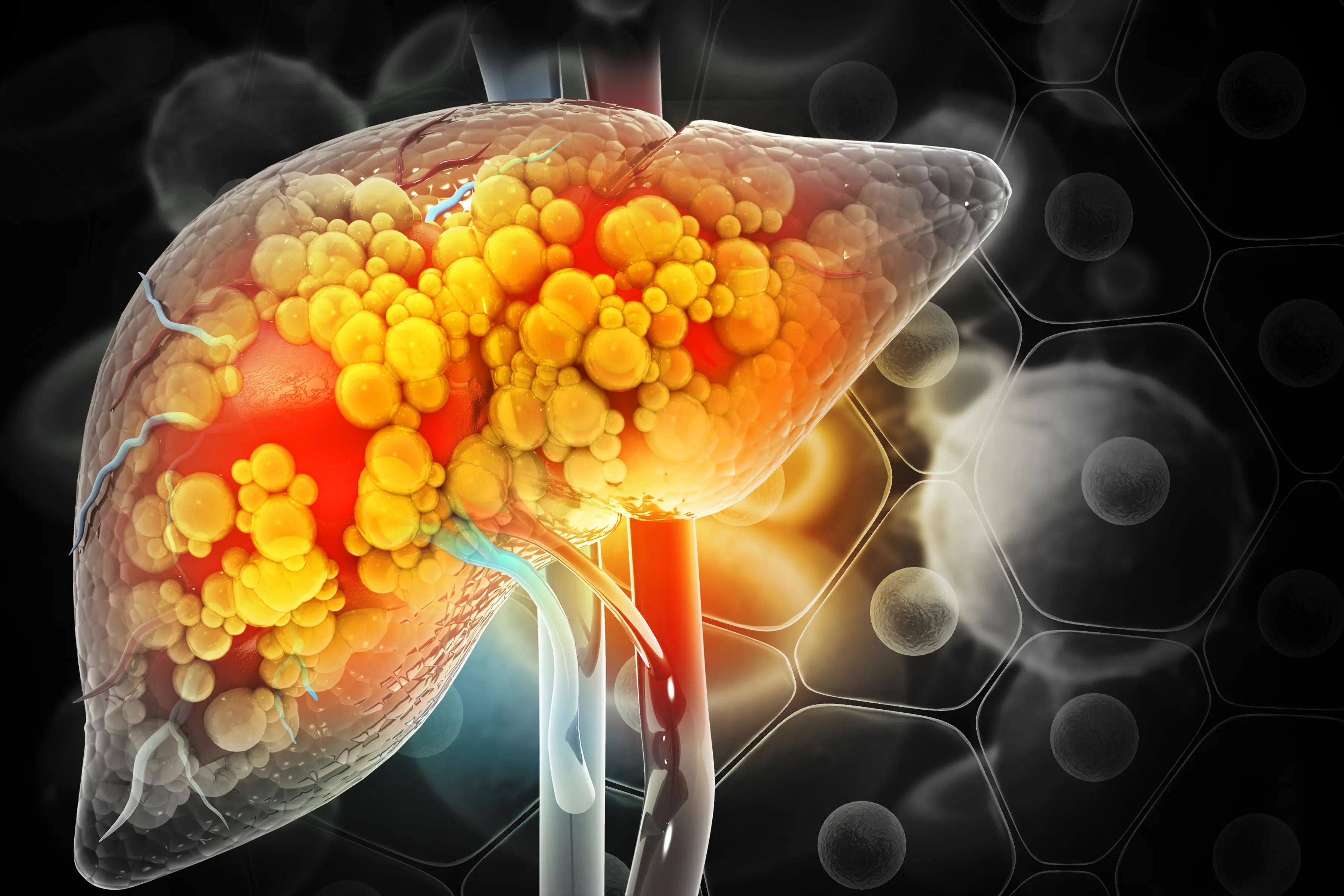
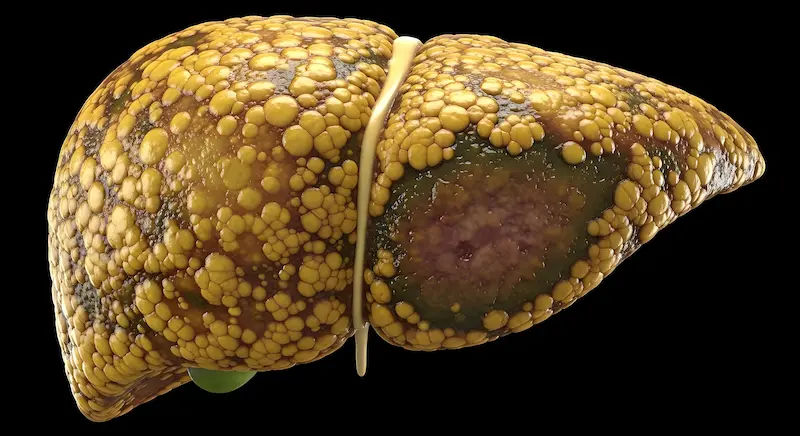
At its core, fatty liver disease, or hepatic steatosis, is exactly what it sounds like: an abnormal accumulation of fat inside liver cells. A healthy liver contains little to no fat. When fat makes up more than 5% of the liver's weight, it's diagnosed as fatty liver disease. This buildup can cause inflammation, damage liver cells, and create scar tissue—a process that can have serious consequences if left unchecked.
The Two Main Types: NAFLD vs. AFLD
Understanding the type is key to understanding the cause and treatment.
Nonalcoholic Fatty Liver Disease (NAFLD): This is the most common form, not linked to heavy alcohol use. It's closely tied to metabolic health—think insulin resistance, obesity, and type 2 diabetes. A more severe subset is called Nonalcoholic Steatohepatitis (NASH), which involves liver inflammation and damage.
Alcoholic Fatty Liver Disease (AFLD): This is caused by consuming large amounts of alcohol. The liver prioritizes breaking down alcohol over its other jobs, which leads to a buildup of fat. This can also progress to alcoholic hepatitis and cirrhosis.
How a Healthy Liver vs. a Fatty Liver Functions?
Your liver is a metabolic powerhouse. It filters toxins, processes nutrients from food, produces bile for digestion, and regulates blood sugar and cholesterol. A fatty liver becomes sluggish and inflamed. Imagine trying to filter water through a clogged sponge; it's inefficient. This impaired function disrupts your entire body's metabolism, often creating a vicious cycle that worsens the condition.
Are You at Risk? Recognizing the Causes and Risk Factors
While the exact cause isn't always clear, fatty liver disease doesn't appear out of nowhere. It's strongly linked to a cluster of metabolic risk factors.
Lifestyle and Metabolic Factors
The primary drivers of NAFLD are:
Overweight or Obesity: This is the single biggest risk factor. Excess weight, particularly around the abdomen, significantly increases strain on the liver.
Insulin Resistance and Type 2 Diabetes: When your body doesn't use insulin effectively, it leads to high blood sugar levels, which promote fat storage in the liver.
High Cholesterol or Triglycerides: Elevated levels of fats in your blood can contribute to fat buildup in the liver.
Poor Diet: A diet high in processed foods, sugary drinks (like soda and juice), refined carbohydrates (white bread, pasta), and saturated fats is a major contributor.
Genetic and Other Contributing Conditions
Genetics: Some people are genetically predisposed to storing fat in their liver.
Polycystic Ovary Syndrome (PCOS): This condition is often accompanied by insulin resistance and obesity.
Sleep Apnea: Research suggests a link between interrupted sleep and liver health.
Underactive Thyroid (Hypothyroidism): This can slow down metabolism and contribute to weight gain.
Listening to Your Body: Symptoms of Fatty Liver Disease
One of the most challenging aspects of this disease is its stealthy nature.
The Dangerous Silence of Early Stage Symptoms
In many cases, there are no noticeable early symptoms of fatty liver. The condition is frequently discovered incidentally during blood tests for other reasons that reveal elevated liver enzymes. This is why understanding your risk factors is so important.
Red Flags: Signs of Advancing Liver Damage
As the disease progresses to more serious inflammation (steatohepatitis) or fibrosis, symptoms may include:
Persistent fatigue or weakness
A dull or aching pain in the upper right abdomen (over the liver)
Unexplained weight loss
Yellowing of the skin and eyes (jaundice)
Swelling in the abdomen (ascites) or legs (edema)
If you experience any of these laterstage symptoms, it is essential to consult a doctor immediately. You can book a quick online consultation with a specialist on Apollo24|7 to discuss your concerns.
Getting a Diagnosis: How Doctors Identify Fatty Liver?
Since symptoms are often absent, diagnosis relies on specific tests.
Common Blood Tests and What They Mean
The first step is usually a liver function test (LFT). This measures enzymes like ALT (Alanine Transaminase) and AST (Aspartate Transaminase). When liver cells are damaged, they release these enzymes into the bloodstream, causing levels to rise. For convenience, Apollo24|7 offers home collection for these blood tests, making it easy to check your liver health.
Imaging Tests: Ultrasound, FibroScan, and More
Ultrasound: This is the most common initial imaging test. It can often detect excess fat in the liver.
Transient Elastography (FibroScan®): This is a specialized, noninvasive test that measures liver stiffness (fibrosis) and fat content, providing a clearer picture of the disease's severity than a standard ultrasound.
CT or MRI Scans: These can provide detailed images and are sometimes used.
The Role of Liver Biopsy
A liver biopsy, where a small sample of liver tissue is removed for analysis, is the gold standard for diagnosing NASH and determining the exact stage of fibrosis. It's typically reserved for cases where the diagnosis is unclear or advanced disease is suspected.
The Road to Reversal: Effective Treatment and Management
The good news? There is no medication specifically approved for fatty liver disease. The best treatment is lifestyle modification.
The 1 Treatment: Sustainable Weight Loss
This is the most effective strategy. Studies show that losing 510% of your body weight can significantly reduce liver fat. A 710% loss can improve inflammation and even reverse early fibrosis.
Designing a LiverFriendly Diet
Focus on a wholefoods, plantforward diet:
What to Embrace: Vegetables, fruits, whole grains, legumes, nuts, lean proteins (fish, poultry), and healthy fats (olive oil, avocados).
What to Avoid: Sugary beverages, processed foods, refined carbs (white bread, pasta, pastries), and excessive red meat.
Consider: Reducing fructose intake, commonly found in soda and processed foods, is particularly beneficial.
The Power of Movement: Exercise Recommendations
Regular exercise helps improve insulin sensitivity and promotes weight loss. Aim for:
Aerobic Exercise: At least 150 minutes of moderate intensity (brisk walking, cycling) or 75 minutes of vigorous intensity exercise per week.
Resistance Training: Include strength training (weight lifting, bodyweight exercises) at least 2 days a week.
Managing Underlying Conditions (Diabetes, Cholesterol)
Working with your doctor to tightly control blood sugar if you have diabetes and manage cholesterol levels is a critical part of treating the root causes of NAFLD.
Preventing Fatty Liver Disease: A Proactive Approach
Prevention mirrors treatment. The best way to prevent fatty liver disease is to maintain a healthy weight, eat a balanced diet, exercise regularly, and limit alcohol consumption. Think of it as investing in your metabolic health. Regular health checkups that include liver function tests are also wise, especially if you have known risk factors.
Key Takeaways: Quick Facts to Remember
Fatty liver disease is common, often silent, but largely reversible.
It's strongly linked to metabolic health: weight, diabetes, and diet.
Early stages typically have no symptoms, making awareness key.
Weight loss of 510% is the most effective treatment.
A wholefood diet and regular exercise are your best medicines.
Avoid alcohol and sugary drinks to protect your liver.
Regular checkups and blood tests are crucial for early detection.
Conclusion
Fatty liver disease is a widespread condition that serves as a clear warning sign from your body about your metabolic health. While its silent progression can be concerning, it also represents a significant opportunity. By understanding the risk factors and recognizing the power of lifestyle changes, you can take control. You have the ability to not only halt the progression of this disease but to reverse it entirely, safeguarding your liver and your overall health for years to come. This journey starts with a single step—perhaps a dietary change, a daily walk, or a conversation with your doctor.
If you have risk factors or are concerned about your liver health, don't wait for symptoms to appear. Consult a doctor online with Apollo24|7 for personalized advice and a proactive health plan.
Consult a General Physician
Consult a General Physician

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Abhishek Ranjan
General Practitioner
4 Years • MBBS
Kolkata
VDC Clinic, Kolkata
More articles from Fatty Liver
Frequently Asked Questions
1. Can a fatty liver ever truly go back to normal?
Yes, absolutely. The liver has a remarkable ability to regenerate. In the early stages of fatty liver disease (steatosis), consistent lifestyle changes like weight loss, a healthy diet, and exercise can completely reverse the condition and return the liver to normal health.
2. What are the best fruits for a fatty liver diet?
Focus on fruits lower in sugar and high in antioxidants and fiber. Berries (blueberries, strawberries), citrus fruits (grapefruit, oranges in moderation), apples, and avocados are excellent choices. It's best to limit very high sugar fruits like mangoes, grapes, and bananas in large quantities.
3. How quickly can you reverse fatty liver disease?
The timeline varies based on the individual and the severity of the disease. With significant commitment to lifestyle changes, improvements in liver fat can be seen on blood tests within a few weeks to months. Significant reversal may take 6 months to a year or more of sustained effort.
4. Is coffee bad for a fatty liver?
Surprisingly, no. Multiple studies have shown that coffee consumption (23 cups per day) is associated with a lower risk of liver fibrosis and progression of fatty liver disease. The antioxidants in coffee are believed to have a protective effect. Of course, avoid loading it with sugar and cream.
5. What is the life expectancy of someone with a fatty liver?
For someone with simple fatty liver (steatosis) who makes positive lifestyle changes, life expectancy is not significantly affected. The serious risk to longevity comes if the disease progresses to advanced cirrhosis or liver cancer. This highlights the critical importance of early intervention and management.

_1.webp)