Understanding Fatty Liver Disease
Gain a comprehensive understanding of Fatty Liver Disease (Hepatic Steatosis), covering causes, symptoms, diagnosis, and the crucial lifestyle interventions needed to reverse liver fat accumulation.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
Fatty liver disease happens when too much fat builds up in your liver. Most people never feel it—until problems appear. The good news: in many cases, fatty liver disease can be prevented, slowed, or even reversed with the right steps. In this guide, we’ll demystify fatty liver disease in plain language, explain the newer terms you may see (NAFLD now often called MASLD; NASH now MASH), and show you exactly how doctors diagnose it and what really works to treat it. You’ll learn the most common causes, what symptoms to watch, which tests to expect (like FibroScan and FIB-4), and how diet, exercise, sleep, and stress fit into recovery. We’ll also cover medicines on the horizon—including the first FDA approved drug for MASH—and when to consider specialty care. If you’ve been told you have a “fatty liver,” or you’re worried about your risk, this article gives you practical tools to protect your liver and your long term health.
Fatty liver disease at a glance
Fatty liver disease simply means there’s more fat inside liver cells than there should be. Two main categories exist: alcohol-related fatty liver (from excess alcohol) and metabolic-related fatty liver, historically called NAFLD (nonalcoholic fatty liver disease). In 2023, experts updated the terminology to MASLD—metabolic dysfunction-associated steatotic liver disease—to reflect the underlying metabolic drivers like insulin resistance and obesity. When fat in the liver becomes inflamed and starts injuring liver cells, NAFLD/MASLD can progress to NASH/MASH (steatohepatitis), which carries a higher risk of scarring (fibrosis) and cirrhosis.
Key point: many people with fatty liver disease don’t drink much alcohol. Their condition stems mostly from metabolic factors such as weight gain around the abdomen, type 2 diabetes, elevated triglycerides, or high blood pressure. Alcohol-related fatty liver is different in cause and management, though both can lead to similar complications if untreated.
Why do so many people have fatty liver disease without knowing? Early disease is often silent—no pain, no yellowing of the eyes, no obvious signs. Routine blood tests may be normal, and ultrasound isn’t always ordered unless risk is suspected. That’s why understanding your personal risk factors and discussing screening with your clinician matters. Unique insight: even small, sustained lifestyle changes—think 200–300 extra daily steps plus replacing one sugar-sweetened drink with water—can measurably reduce liver fat over weeks, building momentum toward bigger wins.
How common is fatty liver disease and why it matters?
About one in four adults worldwide has fatty liver disease, making it the most common chronic liver condition globally. Rates are even higher among people with type 2 diabetes and obesity. While many live for years with simple steatosis (fat only), a subset develops steatohepatitis (MASH/NASH), fibrotic scarring, and eventually cirrhosis. Importantly, the leading causes of death in people with fatty liver disease are heart disease and cancer—not just liver failure—because the same metabolic factors that drive liver fat also strain the heart, blood vessels, and kidneys.
Why this matters to you: early detection and focused lifestyle changes can change the trajectory. In clinical guidance, losing about 7–10% of body weight is associated with resolution of steatohepatitis and even regression of fibrosis in many patients, especially when combined with exercise and better metabolic control. That’s a powerful return on investment.
For families, this is also a pediatric issue. Children and teens—especially those with higher weight, sedentary habits, or insulin resistance—can develop fatty liver disease. Early habits around sleep, screen time, sugary drinks, and daily movement influence lifetime risk. A practical household approach (e.g., switching to family-wide water-first beverage rules and shared evening walks) can help everyone reduce risk while avoiding stigma.
Unique insight: think of fatty liver disease as a “metabolic traffic jam.” Clearing the jam doesn’t require perfection—just steady, prioritized flow in the right direction: fewer incoming sugars and refined starches, more fiber and protein, and regular energy “tolls” through movement.Consult a Top Hepatologist
Causes and risk factors you can and can’t control
Metabolic drivers top the list. Excess calories—especially from refined carbohydrates and sugar-sweetened beverages—promote de novo lipogenesis (your liver turns sugar into fat). Over time, insulin resistance develops, raising triglycerides and hepatic fat. Central obesity (larger waistline), type 2 diabetes, metabolic syndrome, high triglycerides, and hypertension cluster together, compounding risk. This is why fatty liver disease is often called the “liver’s expression” of metabolic dysfunction.
Genetics also play a role. Variants in genes like PNPLA3 and TM6SF2 can increase susceptibility—one reason some people with “normal” weight still develop fatty liver (often called “lean” fatty liver disease). Ethnic background matters as well; some groups have higher risk for the same BMI due to genetic and environmental factors.
Other contributors:
• Medications: some drugs can promote steatosis (e.g., certain steroids, amiodarone). Never stop a prescribed medication without consulting your doctor.
• Endocrine conditions: polycystic ovary syndrome (PCOS), hypothyroidism, and obstructive sleep apnea (OSA) are linked to fatty liver—treating OSA can improve metabolic health.
• Diet pattern and sleep: high late-night calorie intake, inadequate sleep, and high stress can worsen insulin resistance.
What you can’t control (genetics, age) informs your starting risk. What you can control—weight trajectory, food pattern, movement, sleep, alcohol limits—shapes your outcome. Unique insight: a “plate-first” approach (half vegetables, quarter protein, quarter whole grains or starchy veg) simplifies choices and reduces liver fat drivers without calorie counting—an approach used successfully in diabetes prevention and liver clinics.
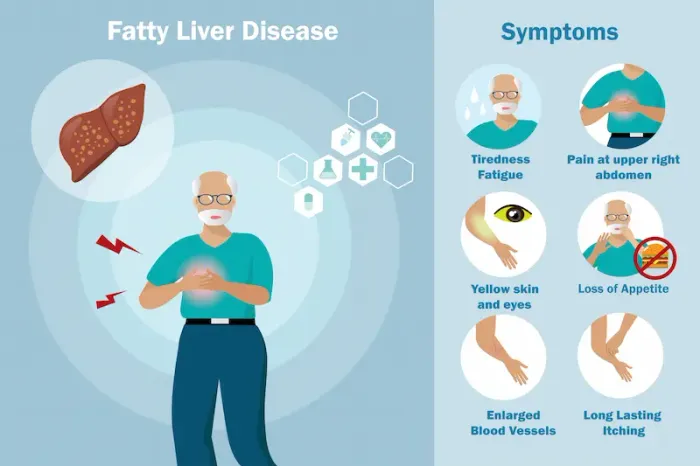
Symptoms, red flags, and when to seek medical care
Most people with fatty liver disease have no obvio
us symptoms. Some report fatigue, vague right upper abdominal discomfort, or a sense of fullness. These are nonspecific and can stem from many causes. That’s why risk-based screening is important.
Red flags to act on:
• Signs of advanced liver disease: yellowing of skin/eyes, easy bruising, swollen legs or abdomen (ascites), confusion or sleepiness (possible hepatic encephalopathy), vomiting blood or black stools (from varices). These require urgent care.
• Rapidly worsening fatigue, unintentional weight loss, or persistent right upper quadrant pain.
• If you have diabetes, obesity, or high triglycerides, ask your clinician whether you should be screened for fatty liver disease even if you feel well.
If you have concerning symptoms or your lab tests show abnormal liver enzymes for more than a couple of weeks, consider an online consult to triage next steps. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. Seek emergency care for jaundice with fever, severe abdominal swelling, confusion, or vomiting blood.
Unique insight: a “symptom diary” can help you and your clinician connect dots. Track fatigue levels, sleep quality, timing of meals, and alcohol intake for two weeks. Sometimes patterns (e.g., evening heavy meals and poor sleep) reveal actionable contributors.
How fatty liver disease is diagnosed?
Your clinician will start with history (including alcohol intake), exam, and blood tests: liver enzymes (ALT, AST), bilirubin, albumin, platelet count, lipid profile, and HbA1c if diabetes is suspected. Many with fatty liver have normal ALT/AST, so normal labs don’t rule it out.
Imaging:
• Ultrasound can detect moderate to severe steatosis but misses mild fat and doesn’t assess fibrosis well.
• Transient elastography (FibroScan) measures liver stiffness (a proxy for fibrosis) and controlled attenuation parameter (CAP) for fat. It’s noninvasive, quick, and widely used to stage risk.
• MRI-PDFF precisely quantifies liver fat, often used in research or complex cases.
Risk scores help decide who needs advanced testing or referral:
• FIB-4 score uses age, AST, ALT, and platelets to estimate fibrosis risk. Low scores suggest low risk; high scores suggest advanced fibrosis and need for specialist care. Do not self-diagnose—scores guide, not replace, clinical judgment.
• NAFLD Fibrosis Score is another validated tool that incorporates multiple labs and clinical factors.
Liver biopsy remains the gold standard to confirm steatohepatitis and stage fibrosis, but it’s reserved for selected cases, such as unclear diagnosis or when results will change management.
If your clinician orders labs such as HbA1c, lipid panel, hepatitis B/C screening, or vitamin D, Apollo 24|7 offers convenient home collection for tests, which can help you complete the workup without disrupting your schedule.
Unique insight: Ask for your FIB-4 and, if available, FibroScan results to be explained in plain language (e.g., “low, intermediate, high risk”) and to be tracked over time like you would blood pressure.
Stages and complications over time
Fatty liver disease progresses along a spectrum:
• Steatosis: fat in liver cells without significant inflammation.
• Steatohepatitis (MASH/NASH): fat plus inflammation and cellular injury.
• Fibrosis: scar tissue forms as the liver tries to heal; staged from F0 (none) to F4 (cirrhosis).
• Cirrhosis: advanced scarring that distorts liver architecture; can lead to portal hypertension (varices, ascites), liver failure, and hepatocellular carcinoma (primary liver cancer) .
Not everyone progresses. Many remain stable or improve with lifestyle changes. However, once cirrhosis develops, risks rise substantially and new monitoring becomes essential (e.g., ultrasound every 6 months for liver cancer surveillance). Remember: in MASLD, heart disease is a leading risk; controlling blood pressure, cholesterol, and blood sugar remains lifesaving.
Early action alters the story. Studies and guidelines note that losing 7–10% of body weight can resolve steatohepatitis in many and may regress fibrosis, particularly when weight loss is maintained and combined with regular exercise. Even a 3–5% loss reduces liver fat, which is a motivating early milestone.
Unique insight: Track “non-scale” wins that also predict better outcomes—resting heart rate dropping, waist circumference shrinking, improved sleep duration, and a lower fasting glucose. These often improve before large changes in the scale and keep motivation high.
Treatment you can start today: lifestyle that works
Lifestyle modification is the foundation of treating fatty liver disease.
Targets that move the needle:
• Weight loss: Aim for 7–10% of current body weight; even 3–5% reduces liver fat, while ≥10% offers the highest chance to improve fibrosis.
• Diet pattern: A Mediterranean-style pattern—vegetables, legumes, fruits, whole grains, nuts, olive oil, and fish—has the strongest evidence for improving metabolic health and liver fat. Reduce added sugars (especially sugary drinks), refined grains, and ultra-processed foods—long-tail keywords: Mediterranean diet for fatty liver; best foods for fatty liver.
• Protein and fiber: Adequate protein (especially with resistance training) preserves lean mass during weight loss. Aim for 25–30g fiber daily via vegetables, fruits, legumes, and whole grains.
• Exercise: Both aerobic and resistance training reduce liver fat—independent of weight loss. Target 150–300 minutes/week of moderate aerobic activity plus 2–3 resistance sessions. Start where you are: 10-minute walks after meals improve glucose handling and lower liver fat inputs. Long-tail keyword: exercise plan for fatty liver.
• Alcohol: If you have MASLD, limit or avoid alcohol; even moderate intake can worsen liver inflammation in some people. Discuss personalized limits with your clinician.
• Sleep and stress: Treat sleep apnea if present; prioritize 7–9 hours of quality sleep. Chronic stress drives cravings and metabolic dysregulation; try brief daily stress relief routines.
Food swaps that help:
• Replace sugar-sweetened beverages with water, sparkling water, or unsweetened tea/coffee.
• Choose whole fruit over fruit juice.
• Swap refined grains (white bread/rice) for whole grains or legumes.
• Use olive oil instead of butter/ghee for most cooking; keep portions mindful if using ghee.
• Build a default plate: half vegetables, quarter protein, quarter whole grain/starchy veg.
Unique insight: Micro-periodization. Plan “push” weeks (slightly tighter calorie budget, extra exercise session) alternating with “consolidation” weeks (maintenance of new habits). This rhythm helps avoid burnout and supports long-term adherence—crucial for fatty liver disease reversal.
Medical therapies, procedures, and what’s next
While lifestyle is first-line, medications can help selected patients:
• Vitamin E (800 IU/day) can improve steatohepatitis in non-diabetic adults but has potential risks (e.g., bleeding). Use only under medical guidance.
• Pioglitazone benefits steatohepatitis, especially in type 2 diabetes, but may cause weight gain; shared decision-making is essential.
• GLP-1 receptor agonists (e.g., semaglutide) drive weight loss and improve liver fat and inflammation; large trials are ongoing for fibrosis benefits. They’re commonly used for diabetes and obesity management and can be part of a comprehensive plan. Long-tail keyword: GLP-1 semaglutide fatty liver.
• Resmetirom (a thyroid hormone receptor-β agonist) became the first FDA-approved treatment for MASH with moderate-to-advanced fibrosis (F2–F3) in 2024. It reduces liver fat and improves fibrosis markers; candidacy depends on staging and specialist evaluation. Long-tail keyword: resmetirom for MASH.
Procedures:
• Bariatric/metabolic surgery can produce substantial weight loss, improve diabetes, and often resolve steatohepatitis and regress fibrosis in many patients; it’s considered for those with obesity not responding to medical therapy.
• Endoscopic weight-loss procedures may be options in selected cases.
Monitoring:
• Expect periodic labs, FIB-4, and possibly repeat FibroScan to track fibrosis risk. Avoid “detoxes” or unproven supplements that promise rapid liver cleansing—some can harm the liver.
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7 to discuss medications or referral for advanced therapies.
Unique insight: Think “stacked therapies.” Combining modest weight loss, resistance training, sleep optimization, and (when indicated) a GLP 1 RA often beats any single intervention—because liver, muscle, gut hormones, and brain appetite pathways improve together.
Consult a Top Hepatologist
Conclusion
Fatty liver disease is both a warning light and an opportunity. It signals that the body’s energy systems are out of balance—but with the right changes, the liver’s extraordinary capacity to heal can take over. Start with the fundamentals that matter most: reduce added sugars and refined carbs, build a Mediterranean-style plate, move your body most days, and aim for a steady 7–10% weight loss if you have overweight. Track your progress with practical metrics—waist size, step counts, sleep hours—and partner with your clinician to monitor labs, FIB 4, and potentially FibroScan. If you live with diabetes or high cholesterol, optimizing those conditions protects your liver and your heart.
Medical therapies are evolving. For selected people with MASH and fibrosis, options like resmetirom and GLP 1 RAs can complement lifestyle and accelerate improvement. If you’re unsure where to start, or if results have plateaued, an online consult can help you personalize your plan. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. And if your care plan includes lab work, Apollo 24|7 offers a home collection to keep you on track.
Your liver works tirelessly for you. With small daily steps and the right support, you can return the favor—and change your long-term health story.
Consult a Top Hepatologist

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)
Consult a Top Hepatologist

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Pukhraj Singh Jeji
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD ( Internal Medicine ), DM ( Gastroenterology ), Consultant - Gastroenterology
Bhubaneswar
Apollo Hospitals Old Sainik School Road, Bhubaneswar

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. Aswin S. Krishna
Hepatologist
10 Years • MBBS, MD (Internal Medicine,MMC), DM (Hepatology, MMC), PDF(Fellowship in Liver Transplanatation)
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)
More articles from Fatty Liver
Frequently Asked Questions
1) Can fatty liver disease be reversed?
Yes. Early fatty liver (steatosis) often improves with 7–10% weight loss, regular exercise, and a Mediterranean-style diet. Even 3–5% weight loss can reduce liver fat. Ask your doctor how to track improvements with FIB 4 or FibroScan.
2) What is the best diet for fatty liver disease?
A Mediterranean diet pattern—vegetables, legumes, fruits, whole grains, nuts, olive oil, and fish—has strong evidence. Limit sugary drinks and refined carbs. A personalized fatty liver diet plan from a dietitian can help you apply this to your culture and preferences.
3) Do I need a liver biopsy?
Not usually. Most people are staged with noninvasive tools (FIB 4, FibroScan, labs). Biopsy is reserved for unclear cases or when results will change treatment decisions.
4) Are there medications for fatty liver disease?
Lifestyle is first-line. Some patients benefit from vitamin E, pioglitazone, or GLP 1 RAs (e.g., semaglutide) depending on their profile. In 2024, resmetirom was approved for MASH with moderate-to-advanced fibrosis; a specialist can assess eligibility.
5) I don’t drink alcohol. Why do I have fatty liver?
Metabolic factors like insulin resistance, weight gain around the abdomen, and high triglycerides drive most fatty liver disease. This is called MASLD (formerly NAFLD), and it’s very common—even in people who rarely drink.
_2.webp)
.webp)
