What Leads To Symptoms And What Fever In Kids
Understand the common causes of symptoms and fever in children. Learn when to worry, when to treat, and essential tips for managing your child's illness.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
Watching your child develop a fever can be a heart-sinking moment for any parent. That warm forehead instantly triggers a wave of worry. But what if we told you that a fever is not an illness in itself, but rather a powerful sign that your child's body is fighting the good fight? Understanding what a fever truly is—and what it isn't—is the first step toward managing it effectively and calmly. This guide will demystify fever in kids, taking you from the basic "what and why" to the practical "what to do." We'll explore the common causes, from everyday viruses to more serious bacterial infections, and decode the accompanying symptoms like body aches and lethargy. You'll learn how to take an accurate temperature, implement safe and comforting home care strategies, and, crucially, recognize the red flags that mean it's time to call a doctor. Our goal is to replace anxiety with knowledge, empowering you to care for your sick child with confidence.
What exactly is a Fever?
A fever is defined as a temporary increase in body temperature, often due to an illness. It's a common sign of an activated immune system. For children, a rectal temperature of 100.4°F (38°C) or higher is generally considered a fever. It's crucial to remember that the number on the thermometer is just one piece of the puzzle; your child's overall behavior and comfort level are often more important indicators of how sick they are.
The Body's Thermostat: How the Hypothalamus Works
Think of your brain's hypothalamus as the body's sophisticated thermostat. Normally, it sets your body temperature to around 98.6°F (37°C). When viruses, bacteria, or other invaders enter your child's system, their immune cells release substances called pyrogens. These pyrogens act as messengers, traveling to the brain and telling the hypothalamus to raise the body's temperature set-point. It’s not that the body is overheating; it’s that the thermostat has been deliberately turned up.
Why a Higher Temperature is a Defense Mechanism?
This rise in temperature isn't a malfunction; it's a strategic defense. A fever creates a less hospitable environment for many germs, which reproduce best at normal body temperature. It also acts as an alarm bell, rallying the body's immune cells—like white blood cells—to work faster and more efficiently to neutralize the threat. So, while it makes your child feel unwell, the fever itself is a sign that their natural defenses are actively engaged in healing.
Consult Top Specialists
Common Causes of Fever in Children
The vast majority of fevers in kids are caused by infections. Identifying the likely cause helps you understand the expected course of the illness and when to seek further evaluation.
Viral Infections: The Most Frequent Culprits
Viruses are responsible for most childhood fevers. These illnesses are contagious and often come with a recognizable set of symptoms.
• Examples: The common cold, influenza (flu), RSV, croup, stomach flu (gastroenteritis), and common childhood illnesses like chickenpox or roseola.
• Characteristics: Viral fevers can range from low-grade to quite high (103-104°F). They typically follow a course of 3-5 days and are accompanied by symptoms like runny nose, cough, sore throat, vomiting, or diarrhea. Antibiotics are ineffective against viruses; treatment focuses on comfort and hydration.
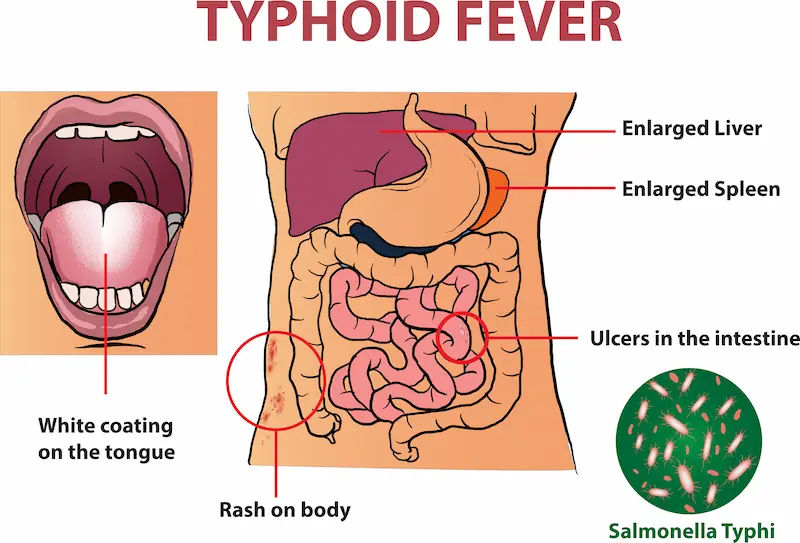
Bacterial Infections: Less Common but Often More Serious
Bacterial infections are less frequent but can be more severe and sometimes require treatment with antibiotics.
• Examples: Strep throat, ear infections, urinary tract infections (UTIs), pneumonia, and sinus infections.
• Characteristics: A high fever in a toddler with an earache, or a fever accompanied by pain during urination, can point toward a bacterial cause. Unlike viral illnesses that often improve on their own, bacterial infections may persist or worsen without treatment. If you suspect a bacterial infection like strep throat or a UTI, consulting a doctor online with Apollo24|7 can provide a quick initial assessment and guidance on whether a test or visit is needed.
Other Potential Causes: Teething, Immunizations, and Overheating
• Immunizations: A low-grade fever after vaccination is a normal immune response and usually resolves within 24-48 hours.
• Overheating: A child can develop a fever from being dressed too warmly or after playing vigorously in hot weather. This usually normalizes quickly once they cool down.
• Teething: While debated, teething may cause a very slight rise in temperature, but it is unlikely to cause a true fever (over 100.4°F). A significant fever during teething is likely due to a coincidental illness.
Decoding the Symptoms: What Your Child's Body is Telling You
A fever is rarely the only symptom. The other signs your child shows are clues to what’s really going on.
The Direct Symptoms of Fever Itself
As the body's thermostat resets, it initiates processes to reach the new, higher temperature. This can cause:
1. Chills and shivering (muscles contracting to generate heat).
2. Feeling cold despite having a warm forehead.
3. Flushed cheeks and glassy eyes.
4. As the fever breaks (the hypothalamus resets to normal), the body sweats to cool down.
Symptoms Caused by the Underlying Illness
These are the symptoms directly caused by the virus or bacteria.
• Respiratory: Cough, runny nose, congestion.
• Gastrointestinal: Vomiting and fever in a child, diarrhea, loss of appetite.
• Pain: Earache, headache, body aches, sore throat.
• General Malaise: Lethargy, irritability, poor sleep.
Red Flag Symptoms: When to Seek Immediate Medical Attention
While most fevers are harmless, certain symptoms warrant immediate medical care:
In an infant under 3 months: Any temperature of 100.4°F (38°C) or higher.
Difficulty breathing or unusual drowsiness.
A stiff neck, severe headache, or unexplained rash.
• Signs of dehydration: No tears when crying, sunken soft spot (in infants), very dry mouth, or no urination for 8+ hours.
• Febrile seizure: A convulsion caused by a rapid spike in fever.
How to Accurately Take Your Child's Temperature?
Accuracy is key to making informed decisions.
Choosing the Right Thermometer
Digital multi-use thermometers are the standard. For infants and young children, rectal temperatures are the most accurate. Forehead (temporal artery) thermometers are a good non-invasive option for quick checks. Ear (tympanic) thermometers can be accurate if placed correctly but are less reliable in young children.
Step-by-Step Guide for Different Age Groups
• Under 3 Months: Use a digital thermometer rectally for the most reliable reading.
• 3 Months to 4 Years: Rectal is still most accurate. Forehead thermometers are a good alternative. Ear thermometers can be used if the child is cooperative.
• 4 Years and Older: Oral (by mouth) is usually accurate if the child can keep their mouth closed around the thermometer. Forehead or ear are also acceptable.
Safe and Effective Home Care Strategies
Your primary goal is to keep your child comfortable and hydrated.
Comfort Measures: Hydration, Rest, and Light Clothing
• Hydration is Critical: Offer plenty of fluids—water, diluted juice, broth, or oral rehydration solutions. Dehydration signs are a key thing to watch for.
• Rest: Their body needs energy to fight the infection.
• Comfortable Clothing: Dress them in light clothing. Bundling them up can trap heat and raise their temperature further.
Using Fever-Reducing Medication Safely (Acetaminophen & Ibuprofen)
Medication should be used for comfort, not just to normalize the temperature.
• Acetaminophen (e.g., Tylenol): Can be used for all ages (consult a doctor for infants under 3 months).
• Ibuprofen (e.g., Advil, Motrin): For children 6 months and older.
• Crucial: Always do it based on your child's weight, not age. Never give aspirin to children due to the risk of Reye's syndrome.
Myths and Practices to Avoid
Avoid cold baths or alcohol rubs. These can cause shivering, which actually raises the core body temperature and can be dangerous.
Do not alternate ibuprofen and acetaminophen unless specifically instructed by your pediatrician, as it increases the risk of dosing errors.
When to Call the Doctor or Seek Emergency Care?
Use these guidelines, but always trust your instincts.
Age-Specific Guidelines for Infants and Older Children
• Under 3 Months: Call your doctor immediately for any fever of 100.4°F (38°C) or higher.
• 3-6 Months: For a fever over 102°F (38.9°C) or if they seem unusually irritable, lethargic, or uncomfortable.
• Any Age: If the fever lasts for more than 3 days, is consistently above 104°F (40°C), or if your child has a chronic medical condition.
Trusting Your Parental Instincts
You know your child best. If your child's condition does not improve after trying these methods, or if something just doesn't feel right, book a physical visit to a doctor with Apollo24|7. A persistent fever or worsening symptoms may require a physical exam or tests, which Apollo24|7 can facilitate, including convenient home collection for tests like a strep test or urine analysis if needed.
Conclusion
A fever in kids, while alarming, is most often a visible sign of a robust and healthy immune system at work. By understanding that it's a defense mechanism, not the enemy, you can shift your focus from fighting the number on the thermometer to providing comforting care for your child. Remember to prioritize hydration, rest, and comfort measures, and use fever-reducing medications wisely. Keep a watchful eye for the red flag symptoms that signal a need for medical intervention, but also trust your gut feeling as a parent. Armed with this knowledge, you can navigate your child's next illness with greater confidence, providing the calm and effective care they need to recover. Your role is not to eliminate the fever, but to support the little warrior inside them as they battle through it.
Consult Top Specialists
Consult Top Specialists

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
14 Years • MBBS, DNB
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Swaroopa Rani
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Internal Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Shiv Krishna Mitra
General Physician/ Internal Medicine Specialist
15 Years • MBBS GEN. MED. PGDRM, MCH
Kolkata
Samaritan Clinic, Kolkata

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)
Consult Top Specialists

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
14 Years • MBBS, DNB
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Swaroopa Rani
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Internal Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Shiv Krishna Mitra
General Physician/ Internal Medicine Specialist
15 Years • MBBS GEN. MED. PGDRM, MCH
Kolkata
Samaritan Clinic, Kolkata

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)
More articles from Fever
Frequently Asked Questions
1. What is considered a high fever in a toddler that I should worry about?
For a toddler, a fever above 102°F (38.9°C) warrants a call to the doctor, especially if it doesn't respond to medication or is accompanied by other concerning symptoms like listlessness or refusal to drink. However, any fever in a child under 3 months (100.4°F or higher) requires immediate medical attention.
2. My child has a fever but no other symptoms. What could it be?
A fever with no other symptoms is common in the early stages of a viral illness. Other symptoms like a runny nose or cough often appear within 24 hours. It can also sometimes indicate a hidden bacterial infection like a UTI. If the fever persists for more than 24-48 hours without any other signs, it's best to consult a doctor.
3. How can I tell if my child's fever is viral or bacterial?
It can be difficult without a medical evaluation. Generally, viral fevers are more common and often come with cold-like symptoms. Bacterial infections may cause more localized symptoms (like an earache or pain during urination) and the fever might be persistently high without the ups and downs seen with viruses. A doctor can make a definitive diagnosis.
4. What should I do if my child has a febrile seizure?
Stay calm. Gently place your child on their side on a soft, safe surface. Do not put anything in their mouth. Time the seizure. Most last less than a minute. After it stops, comfort your child and call your doctor. If the seizure lasts longer than 5 minutes or your child has trouble breathing, call for emergency services immediately.
5. Is it dangerous to have a fever for too long?
The duration of the fever is less critical than the underlying cause. A fever from a common virus may last 3-5 days. The concern is not the fever itself causing damage (which is rare until temperatures exceed 107°F), but rather the progression of the illness. A fever lasting more than 3 days should be evaluated by a doctor to rule out a bacterial infection that may need treatment.