Nipah Virus: Causes and Symptoms
Learn about Nipah virus, its causes, transmission, and key symptoms. Understand the risks, early warning signs, and why timely diagnosis is critical.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. Mohammed Kamran MBBS, FIDM
Last updated on 13th Jan, 2026

Introduction
The Nipah virus (NiV) often emerges in headlines during worrying outbreaks, associated with high fatality rates and significant public health responses. But what exactly leads to the terrifying signs of this disease? Understanding the causes and transmission pathways of the Nipah virus is not just for epidemiologists; it's crucial knowledge for anyone in affected regions to protect themselves and their communities. This article demystifies the journey of the Nipah virus, from its natural reservoir in fruit bats to the severe neurological symptoms it can cause in humans. We will explore the precise causes of Nipah virus infection, detail the progression of symptoms, and outline the critical risk factors. By comprehending what leads to this disease, we can better focus on prevention and know when to seek immediate medical help, such as consulting a specialist online with Apollo24|7 for initial guidance during concerns.
What is the Nipah Virus? Understanding the Pathogen
Discover what the Nipah virus is and gain insight into the pathogen behind it, including its origin, transmission, and health impact.
A Zoonotic Virus from the Henipavirus Genus
Nipah virus is a zoonotic virus, meaning it originates in animals and can jump to humans. It belongs to the Henipavirus genus within the Paramyxoviridae family. It's notorious for causing severe disease in both animals and humans, with a high case fatality rate (estimated between 40% to 75% in past outbreaks according to the WHO). This makes it a pathogen of significant public health concern.
Historical Context: Past Nipah Virus Outbreaks
The virus was first identified in 1999 during an outbreak among pig farmers in Malaysia and Singapore. It gets its name from the Malaysian village of Sungai Nipah. Since then, regular outbreaks have occurred in Bangladesh and India, particularly in the state of Kerala, highlighting specific geographic and environmental risk factors.
Consult Top Specialists for Personalised Tips
The Primary Cause: How Nipah Virus Jumps to Humans
The root cause of Nipah virus infection is human exposure to the virus carried by specific animal hosts. It doesn't spontaneously occur; it requires a "spillover event."
1. The Natural Host: Fruit Bats (Flying Foxes)
The natural reservoir for the Nipah virus is fruit bats of the Pteropus genus, also known as flying foxes. These bats carry the virus without showing any signs of illness themselves. They shed the virus in their saliva, urine, feces, and birthing fluids.
2. The Spillover Event: From Bats to Intermediate Hosts
Human infection occurs through direct or indirect contact with these bat excretions. This transmission of Nipah virus happens in several key ways:
Contaminated Date Palm Sap: A Major Route
A common route of transmission in Bangladesh and India is the consumption of raw date palm sap. Bats can contaminate the sap collection pots with their droppings or urine while feeding on the sap. Drinking this raw, contaminated sap is a significant risk factor.
Infection Through Infected Animals (Pigs, etc.)
The initial Malaysian outbreak involved pigs as intermediate hosts. Bats dropped partially eaten fruit into pigsties; the pigs ate the fruit, became infected, and then amplified the virus. Humans then contracted it through close contact with the infected pigs' respiratory droplets or tissues. Other animals like horses, goats, and cats can also be infected.
3. Human-to-Human Transmission: The Secondary Spread
Once a human is infected, the Nipah virus can spread from person to person, often in healthcare or family settings. This occurs through close contact with the respiratory droplets, saliva, or other bodily fluids of an infected person. This mode of transmission makes outbreak containment challenging and puts healthcare workers at high risk.
From Exposure to Illness: The Pathogenesis of Nipah
Explore the pathogenesis of the Nipah virus, tracing the journey from exposure to illness and understanding its effects on the human body.
Incubation Period: The Silent Phase
The incubation period (time from exposure to the onset of symptoms) typically ranges from 4 to 14 days, though it can be as long as 45 days. During this time, the virus is multiplying within the body, but the person remains asymptomatic.
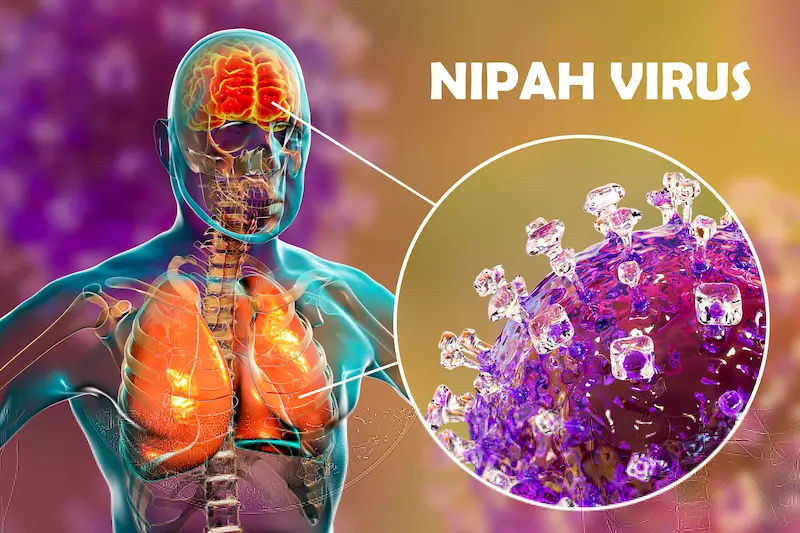
How the Virus Attacks the Body
The virus initially replicates in the respiratory tract. It then spreads through the bloodstream (viremia), invading various organs. Its key target is the endothelium (lining) of blood vessels, causing vasculitis (inflammation) and damaging small blood vessels. This leads to the leakage of fluid and blood, which is a hallmark of the disease. Its most devastating effect is on the central nervous system, where it causes severe inflammation of the brain, known as encephalitis.
Recognizing the Signs: Symptoms of Nipah Virus Infection
The symptoms of Nipah virus infection can range from asymptomatic (no symptoms) to fatal encephalitis. The progression is often rapid.
Initial and Common Symptoms
The illness often begins with non-specific, flu-like symptoms, which can make early diagnosis difficult. These include:
Fever
Headache
Muscle pain (myalgia)
Vomiting
Sore throat
Dizziness
Drowsiness
These initial signs usually last for 3-10 days.
Severe Symptoms and Neurological Complications
If the infection progresses, it leads to severe respiratory and neurological signs, indicating the virus has reached the brain.
Encephalitis: Brain Inflammation
This is the most dangerous complication. Signs of Nipah virus encephalitis include:
Drowsiness progressing to disorientation and confusion.
Altered consciousness.
Severe dizziness.
Atypical symptoms
Some patients may experience seizures or a syndrome where the brainstem shuts down, leading to coma within 24-48 hours.
Late-Onset and Dormant Infections
A unique and terrifying aspect of Nipah is the potential for late-onset or relapse encephalitis, which can occur months or even years after the initial infection. Furthermore, some survivors are left with long-term neurological conditions, such as persistent seizures and personality changes.
Who is at Risk? Key Risk Factors for Nipah Virus
Discover who is at risk for the Nipah virus and understand the key factors that increase susceptibility to enhance awareness and prevention.
Geographic and Occupational Risks
Location: People living in areas where Pteropus bats are common (parts of South and Southeast Asia) and where outbreaks have occurred.
Occupation: Pig farmers, fruit growers, and date palm sap harvesters have a higher occupational risk due to potential contact with bat excretions.
Consumption Habits: Individuals who consume raw date palm sap are at significantly higher risk.
Risks in Healthcare Settings
Healthcare workers and family members caring for infected patients without proper personal protective equipment (PPE) are at a heightened risk due to the virus's ability to spread through close contact with bodily fluids.
Diagnosis and Medical Response
Understand how Nipah virus is diagnosed and managed, including the tests, treatment options, and medical steps for timely and effective care.
How Doctors Test for Nipah Virus
Early diagnosis is critical for managing outbreaks. Diagnosis can be made during the acute phase of illness using real-time polymerase chain reaction (RT-PCR) from throat swabs, nasal swabs, cerebrospinal fluid (CSF), urine, or blood. Later in the course of illness and after recovery, testing for antibodies (IgG and IgM) can be performed.
Treatment Options and Supportive Care
There is no specific drug approved to treat Nipah virus infection. The primary approach is supportive care, which includes:
Managing fever and pain.
Ensuring hydration.
Treating nausea and vomiting.
Providing mechanical ventilation for respiratory support.
Managing seizures and other neurological complications.
Monoclonal antibody therapies (e.g., m102.4) are under investigation and have been used on a compassionate-use basis. Ribavirin has been used, but its efficacy is not fully proven.
Prevention is Key: How to Avoid Nipah Virus Infection
Since treatment is limited, prevention is paramount:
Avoid Raw Date Palm Sap: Do not consume raw date palm sap in endemic areas.
Wash Fruits Thoroughly: Wash all fruits before eating, especially those with bite marks.
Use Protective Covers: Cover sap collection pots to prevent bat access.
Avoid Contact with Bats: Do not handle bats or enter bat roosting areas.
Practice Hygiene: Wash hands regularly with soap and water.
Use PPE in Healthcare Settings: Strict infection control measures and PPE are essential when caring for patients.
Isolate infected individuals to prevent human-to-human transmission.
Conclusion
Understanding what leads to the signs of Nipah virus is the first and most crucial step in combating this deadly disease. The chain of transmission, beginning with fruit bats and moving through contaminated food or direct contact, highlights the complex interplay between human activity, animal habitats, and public health. Recognizing the early, non-specific symptoms is vital, but being aware of the risk factors, like consuming raw date palm sap or caring for an infected person without protection, is what truly empowers prevention. While the medical community continues to research effective treatments and vaccines, our best defense remains vigilance and proactive measures. If you live in or are traveling to an endemic area and develop a high fever with neurological symptoms like confusion or severe drowsiness, it is critical to seek immediate medical attention. You can consult a doctor online with Apollo24|7 for an initial assessment and guidance on the next steps.
Consult Top Specialists
Consult Top Specialists for Personalised Tips

Dr. Swaroopa Rani
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Internal Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Utsa Basu
Diabetologist
14 Years • MBBS , MD
Barasat
Diab-Eat-Ease, Barasat
(75+ Patients)

Dr. Anindita Mondal
General Physician/ Internal Medicine Specialist
8 Years • MBBS
Kolkata
VDC Clinic, Kolkata

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)

Dr. Ishita Mandal
General Surgeon
7 Years • MBBS(hons.), MS(general surgery), General and laparoscopic surgeon
Kolkata
VDC Clinic, Kolkata
Consult Top Specialists

Dr. Swaroopa Rani
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Internal Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Utsa Basu
Diabetologist
14 Years • MBBS , MD
Barasat
Diab-Eat-Ease, Barasat
(75+ Patients)

Dr. Anindita Mondal
General Physician/ Internal Medicine Specialist
8 Years • MBBS
Kolkata
VDC Clinic, Kolkata

Dr. Santanu Mandal
General Physician/ Internal Medicine Specialist
18 Years • MD (Physician), DNB (General Medicine)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(25+ Patients)

Dr. Ishita Mandal
General Surgeon
7 Years • MBBS(hons.), MS(general surgery), General and laparoscopic surgeon
Kolkata
VDC Clinic, Kolkata
More articles from Fever
Frequently Asked Questions
Can you get Nipah virus from eating fruit?
Yes, but only if the fruit has been contaminated by an infected bat. This typically happens if a bat drops saliva or excretions on the fruit or takes a bite. Thoroughly washing and peeling all fruits, especially those with bite marks, significantly reduces this risk.
What is the first sign of Nipah virus?
The first signs are usually non-specific and flu-like, most commonly a sudden onset of fever and headache. These are often followed by muscle pain, vomiting, and a sore throat.
How long does it take for Nipah virus symptoms to appear?
The incubation period for Nipah virus is typically between 4 to 14 days after exposure. In rare cases, it can extend up to 45 days.
Is there a vaccine for the Nipah virus?
No, there is currently no commercially available vaccine for humans against the Nipah virus. Several vaccines are in various stages of development and clinical trials.
Can Nipah virus be cured?
There is no specific antiviral cure for Nipah virus. Treatment is supportive, focusing on managing complications like respiratory distress and encephalitis. The mortality rate remains high, making prevention critically important.