Difference Between Angioplasty And Angiography
Understand the difference between angiography and angioplasty, their uses, procedures, risks, recovery, and costs. Learn how these heart procedures help diagnose and treat blocked arteries effectively.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
If you or a loved one has been told you might need a heart test or procedure, the terms “angiography” and “angioplasty” can sound confusingly similar. Here’s a simple way to think about it: angiography is the camera; angioplasty is the toolkit. Angiography is an imaging test that shows doctors where your arteries are narrowed or blocked. Angioplasty is a treatment that opens those narrowed or blocked arteries—often during the same hospital visit.
In this guide, we’ll demystify the difference between angioplasty and angiography, explain why and when each is used, walk you through what to expect before, during, and after, and help you ask the right questions. We’ll also compare risks, recovery, costs, and alternatives like bypass surgery or medications. By the end, you’ll have a clear, practical understanding to make informed decisions with your care team.
Note: If you’re experiencing new or worsening chest pain, shortness of breath, or symptoms suggestive of a heart attack, seek emergency care immediately. For non-urgent questions or follow-up, you can consult a cardiologist online with Apollo 24|7.
What Are Angiography and Angioplasty?
Here’s an understanding of angiography and angioplasty:
Angiography = the diagnostic camera
Coronary angiography is a specialised X-ray test that uses a thin tube (catheter) and contrast dye to map blood flow in the heart’s arteries. Think of it as a live video of your heart’s plumbing that shows where arteries are narrowed or blocked. It’s diagnostic—meaning it tells doctors what’s wrong—but it doesn’t fix the problem by itself. Angiography is often recommended if you have concerning symptoms (like chest pain), abnormal stress-test results, or during/after a heart attack to find the culprit artery.
Angioplasty = the treatment toolkit
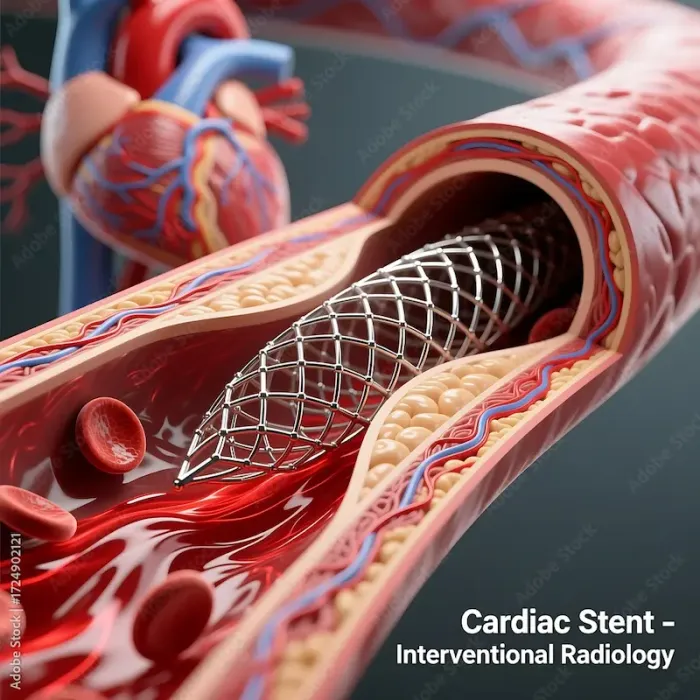
Angioplasty (also called PCI—percutaneous coronary intervention) is a minimally invasive treatment used to open narrowed or blocked arteries. A tiny balloon is inflated at the blockage site to widen the artery, and a stent (a small metal mesh tube) is usually placed to help keep it open. Angioplasty can be planned in advance (elective) or done urgently during a heart attack to quickly restore blood flow and limit heart damage.
Consult Top Heart Specialists
When and Why Each Is Used?
Your doctor may suggest coronary angiography if:
• You have persistent chest pain (angina), shortness of breath, or reduced exercise tolerance.
• A stress test or CT scan suggests significant blockage.
• You had a heart attack (to identify and treat the culprit artery).
• You have unusual symptoms with high cardiac risk.
Angiography helps answer “How severe and where are the blockages?” and “What treatment is best—medicines, angioplasty, or bypass surgery?”
Common reasons for angioplasty
Angioplasty is considered when:
• Angiography shows a significant narrowing (often ≥70%, or less if blood flow is clearly impaired) that correlates with symptoms.
• You have unstable symptoms or a heart attack, where quick re-opening lowers the risk of death and complications.
• You have ongoing angina despite optimal medication.
• The anatomy is suitable for stenting rather than bypass.
Is angiography always done before angioplasty?
Usually, yes. Angiography provides the roadmap to decide whether angioplasty is necessary and safe. In emergencies (like heart attacks), doctors may go from “diagnose to treat” immediately in the same procedure. Non-invasive tests sometimes guide plans, but a definitive angiography is typically performed before stenting.
If you’re unsure about the next steps after an abnormal test or new symptoms, consult a doctor online with Apollo 24|7 for timely guidance and to plan further evaluation.
Step-by-Step: What Happens During Each Procedure
Here’s what happens during each procedure:
Access sites: wrist (radial) vs groin (femoral)
• Radial (wrist) access is increasingly preferred. It’s associated with fewer bleeding complications, faster mobility, and high patient comfort.
• Femoral (groin) access may be chosen for complex cases or when radial arteries are too small or previously used.
Contrast dye and X-ray imaging
For angiography, a catheter is gently threaded to the heart arteries. Contrast dye is injected, and X-ray images capture blood flow in real time. You might feel a brief “warm flush” during dye injection. Tell your team about any past dye reactions or kidney disease; they’ll take precautions like hydration and using the lowest necessary dye dose.
Ballooning and stenting during angioplasty
If angioplasty is needed, a tiny balloon is positioned where the artery narrows and inflated to compress plaque against the vessel wall. A stent (often a drug-eluting stent that slowly releases medicine) is then deployed to keep the artery open. The balloon is deflated and removed, leaving the stent in place. Total time ranges from 30 minutes to two hours, depending on complexity. Most patients go home the same day or next day, especially after radial access.
Consult Top Heart Specialists
Safety, Risks, and Complications—What the Data Say
Here’s the risks of angiography and how they’re minimised:
Coronary angiography is considered low risk, with serious complications uncommon (generally less than 1%). Potential issues include bleeding or bruising at the access site, allergic reactions to contrast dye, arrhythmias, and rarely stroke or heart attack. Kidney function can be affected by contrast, especially in people with chronic kidney disease or diabetes; your care team may check creatinine and ensure good hydration before and after. If lab tests like kidney function are advised, Apollo 24|7 offers convenient home collection to make pre-procedure testing easier.
Angioplasty risks, restenosis, and stent types
Angioplasty carries procedure-related risks—bleeding, vessel injury, heart attack, stroke, or emergency bypass surgery—but these are uncommon in experienced centers. The main long-term concern used to be restenosis (re-narrowing). Drug-eluting stents have significantly lowered restenosis rates (often to single-digit percentages), compared with higher rates seen historically with bare-metal stents. You’ll be prescribed antiplatelet medicines (e.g., aspirin plus a P2Y12 inhibitor like clopidogrel) to prevent stent thrombosis.
Special considerations: kidney disease, diabetes, bleeding risk
• Kidney disease: Extra precautions to limit contrast dye and support hydration reduce risk of contrast-induced kidney injury.
• Diabetes: Higher risk of restenosis; modern drug-eluting stents help. Good glucose control improves outcomes.
• Bleeding risk: Radial access and careful antiplatelet management reduce bleeding. Your team balances clotting vs bleeding risk, especially if you need surgery soon.
Recovery and Aftercare: What to Expect at Home
Here’s the recovery and aftercare after angioplasty:
Activity timelines: hours to days
• After angiography via the wrist, many people sit up and walk within hours, and can resume most activities within 24–48 hours. Bruising at the wrist is common.
• After angioplasty, expect to rest the access arm/leg for a day, avoid heavy lifting for a few days, and gradually return to normal activities over a week. Your doctor will provide specific instructions based on your case.
Medicines after angioplasty (antiplatelets) and follow-up
You’ll likely take dual antiplatelet therapy for several months (the exact duration depends on stent type and clinical scenario), plus statins, blood pressure medicines, and possibly others. Don’t stop antiplatelets without talking to your cardiologist, as doing so can increase the risk of stent thrombosis. A follow-up visit typically happens within a few weeks to monitor recovery and optimise medication.
When to call a doctor—and who to contact
Call your care team urgently if you notice severe or worsening chest pain, fainting, unusual shortness of breath, significant bleeding, or signs of infection at the access site. For non-emergency concerns, you can book a quick online follow-up with Apollo 24|7. If symptoms persist beyond two weeks despite treatment, consult a doctor online with Apollo 24|7 for further evaluation.
Outcomes, Success Rates, and Long-Term Heart Health
Here’s how success is measured for each:
• Angiography “success” means high-quality images that accurately show whether and where blockages exist, guiding next steps.
• Angioplasty “success” means restoring adequate blood flow (TIMI flow grade 3) with a well-expanded stent and no major complications. For heart attacks, timely angioplasty lowers death and improves heart function.
Lifestyle, cardiac rehab, and preventing future blockages
Regardless of the procedure, long-term heart health depends on:
• Cardiac rehab and exercise (as advised by your doctor).
• Stopping smoking and limiting alcohol.
• Heart-healthy diet (Mediterranean-style), weight management, and stress control.
• Adhering to medicines for cholesterol, blood pressure, and diabetes.
Alternatives and How Decisions Are Made
Here are some alternatives:
Medications, coronary bypass (CABG), and shared decision-making
Not every blockage needs a stent. Options include:
• Optimal medical therapy: anti-anginal medicines, statins, BP and diabetes control, lifestyle changes. Many patients improve without intervention.
• CABG (bypass surgery): Often preferred for complex multi-vessel disease, left main disease, or in some diabetics, offering durable relief and survival benefits in selected groups.
Emergency heart attack care vs elective planning
During a heart attack (STEMI), angioplasty is the standard emergency treatment to rapidly restore blood flow. In non-emergency settings, there’s time to consider all options—including doing nothing immediately and focusing on medicines—depending on your risk and goals.
Conclusion
The key difference between angiography and angioplasty is purpose: angiography is a diagnostic test that shows where and how severely your arteries are narrowed; angioplasty is a treatment that opens those narrowed arteries, often with a stent. In many cases, both happen in a seamless sequence—diagnose, then treat—especially during a heart attack. While the procedures are generally safe and recovery is quick (particularly with wrist access), the best long-term outcomes come from a comprehensive plan: medications, cardiac rehab, and sustainable lifestyle changes.
If you’ve been advised to undergo angiography or angioplasty, don’t hesitate to ask your cardiologist about access site options, alternatives like medications or bypass, stent type, antiplatelet duration, and recovery expectations. For non-urgent questions or to arrange follow-up, you can consult a cardiologist online with Apollo 24|7. If your doctor recommends pre-procedure blood tests, Apollo 24|7 also offers convenient home sample collection.
Your heart health is a journey—these tools help along the way, but your daily habits drive the destination.
Consult Top Heart Specialists
Consult Top Heart Specialists

Dr. Syed Akram Ali
Cardiologist
14 Years • MBBS DCH DNB(PED) DNB(CARD) CONSULTANT INTERVENTOINAL CARDIOLOGIST, EUROPEAN SOCIETY OF CARDIOLOGY CERTIFIED HEART FAILURE SPECIALIST
Hyderabad
AYMAN POLYCLINIC, Hyderabad

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr. Sibashankar Kar
Cardiologist
10 Years • MBBS, DNB
Bhubaneswar
Hi-Tech Medical College & Hospital, Bhubaneswar
Consult Top Heart Specialists

Dr. Syed Akram Ali
Cardiologist
14 Years • MBBS DCH DNB(PED) DNB(CARD) CONSULTANT INTERVENTOINAL CARDIOLOGIST, EUROPEAN SOCIETY OF CARDIOLOGY CERTIFIED HEART FAILURE SPECIALIST
Hyderabad
AYMAN POLYCLINIC, Hyderabad

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr. Sibashankar Kar
Cardiologist
10 Years • MBBS, DNB
Bhubaneswar
Hi-Tech Medical College & Hospital, Bhubaneswar
Consult Top Heart Specialists

Dr. Syed Akram Ali
Cardiologist
14 Years • MBBS DCH DNB(PED) DNB(CARD) CONSULTANT INTERVENTOINAL CARDIOLOGIST, EUROPEAN SOCIETY OF CARDIOLOGY CERTIFIED HEART FAILURE SPECIALIST
Hyderabad
AYMAN POLYCLINIC, Hyderabad

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Zulkarnain
General Physician
2 Years • MBBS, PGDM, FFM
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Dr. Sibashankar Kar
Cardiologist
10 Years • MBBS, DNB
Bhubaneswar
Hi-Tech Medical College & Hospital, Bhubaneswar
More articles from General Medical Consultation
Frequently Asked Questions
Q1: Is angiography always required before angioplasty?
Generally yes. Angiography maps your arteries to confirm if angioplasty is needed and safe. In emergencies, doctors may go directly from angiography to angioplasty in one session.
Q2: How long does coronary angiography take and what is recovery like?
The angiography procedure time is typically 30–60 minutes. With wrist access, many patients go home the same day and resume light activities within 24–48 hours.
Q3: What are the risks of angiography contrast dye?
Allergic reactions and kidney effects can occur but are uncommon. Your team may test kidney function and use hydration strategies to lower risk. If needed, Apollo 24|7 offers home collection for tests like creatinine.
Q4: How long is angioplasty recovery time and what restrictions apply?
Many people return to normal light activities within a few days, avoiding heavy lifting for about a week. You’ll take antiplatelet medicines as advised; don’t stop them without medical advice.
Q5: What’s the difference between drug-eluting and bare-metal stents?
Drug-eluting stents slowly release medication to reduce re-narrowing and are now standard in most cases. Bare-metal stents are used less commonly and have higher restenosis rates.