Bone Marrow Failure Syndrome; A Comprehensive Guide to Symptoms & Treatment
Discover everything about Bone Marrow Failure Syndrome, including its symptoms, causes, diagnosis, and treatment options such as bone marrow transplants and immunosuppressive therapy.

Written by Dr. Siri Nallapu
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
Have you been feeling unusually tired, bruising more easily, or catching every bug that goes around? While these can be signs of many common issues, they are also the classic, silent whispers of a more serious condition: bone marrow failure syndrome. This is not a single disease but a group of disorders where the bone marrow—the vital factory inside your bones—slows or stops producing enough healthy blood cells. This disruption can affect your energy, your body's ability to fight infection, and its power to clot blood. Understanding this complex condition is the first step toward managing it. This guide will walk you through what bone marrow failure is, its signs, causes, and the modern treatments that offer hope and health.
What is Bone Marrow and Why is it So Important?
The Factory of Your Blood: Red Cells, White Cells, and Platelets
Imagine your bone marrow as a bustling, highly productive factory nestled within the cavities of your larger bones, like the hip and thigh bones. This factory is responsible for haematopoiesis—the continuous production of life-sustaining blood cells from special cells called haematopoietic stem cells.
- Red Blood Cells (RBCs): These are the oxygen carriers. They contain haemoglobin, which picks up oxygen from your lungs and delivers it to every tissue and organ in your body. Without enough RBCs, you develop anaemia, leading to fatigue and shortness of breath.
- White Blood Cells (WBCs): These are your body's defence army. They identify and fight off bacteria, viruses, and other foreign invaders. A low WBC count leaves you highly vulnerable to infections.
- Platelets: These are tiny cell fragments that act as your body's emergency repair crew for bleeding. They rush to the site of a cut or injury to form clots and stop bleeding. A low platelet count causes easy bruising and excessive bleeding.
The seamless operation of this factory is non-negotiable for health. In bone marrow failure, this production line breaks down.
What is Bone Marrow Failure Syndrome (BMF)?
When the Production Line Breaks Down
Bone marrow failure syndrome occurs when the marrow fails to produce sufficient numbers of one or more of these vital blood cells. This can happen in two primary ways:
- The Stem Cells are Damaged or Destroyed: This is common in acquired conditions like Aplastic Anaemia, where the body's own immune system mistakenly attacks the stem cells.
- The Stem Cells are Defective from Birth: This is the case in inherited syndromes, where a genetic mutation means the stem cells are unable to produce healthy blood cells effectively or are prone to dying early.
The result is a deficiency known as pancytopenia (low counts of all three blood cell types) or deficiencies in specific cell lines, leading to a cascade of health problems.
Common Types of Bone Marrow Failure Syndromes
BMF syndromes are broadly categorised into acquired and inherited types.
Acquired Bone Marrow Failure Syndromes
These are not present at birth but develop later in life due to environmental factors, immune responses, or unknown causes.
Health topic carousel:
Doctor's speciality: Haematology
Text: Consult an Haematologist doctor for the best advice
Aplastic Anaemia: The Most Common Acquired Form
In Aplastic Anaemia, the bone marrow becomes empty or "aplastic," and stops producing new cells. It is often considered an autoimmune disorder. A unique insight often missed is that it can sometimes evolve into another condition, like PNH or even MDS, making ongoing monitoring crucial.
Myelodysplastic Syndromes (MDS)
In MDS, the marrow produces cells, but they are dysfunctional ("dysplastic") and do not mature properly. These abnormal cells often die in the marrow or shortly after entering the bloodstream. MDS carries a risk of progressing to acute myeloid leukaemia (AML).
Paroxysmal Nocturnal Haemoglobinuria (PNH)
PNH is a rare, acquired genetic disorder where red blood cells are missing certain proteins, making them susceptible to destruction by the body's complement system (part of the immune system). This leads to red blood cell breakdown (haemolysis), blood clots, and can be associated with bone marrow failure.
Inherited Bone Marrow Failure Syndromes
These are caused by specific genetic mutations passed from parents to children.
Fanconi Anaemia
This is characterised by bone marrow failure, physical abnormalities, and a high risk of developing certain cancers. The genes involved are critical for DNA repair.
Dyskeratosis Congenita
Often identified by a classic triad of nail dystrophy, skin rashes, and white patches in the mouth, this syndrome is caused by defects in telomere maintenance, leading to premature ageing of cells and bone marrow failure.
Shwachman-Diamond Syndrome
This primarily affects the bone marrow and pancreas, leading to neutropenia (low neutrophils, a type of WBC) and problems with nutrient absorption.
Recognising the Signs: Symptoms of Bone Marrow Failure
The symptoms are directly tied to which blood cell lines are deficient.
Symptoms Caused by Low Red Blood Cells (Anaemia)
- Persistent fatigue and weakness
- Pale skin or pallor
- Shortness of breath, especially with exertion
- Dizziness or lightheadedness
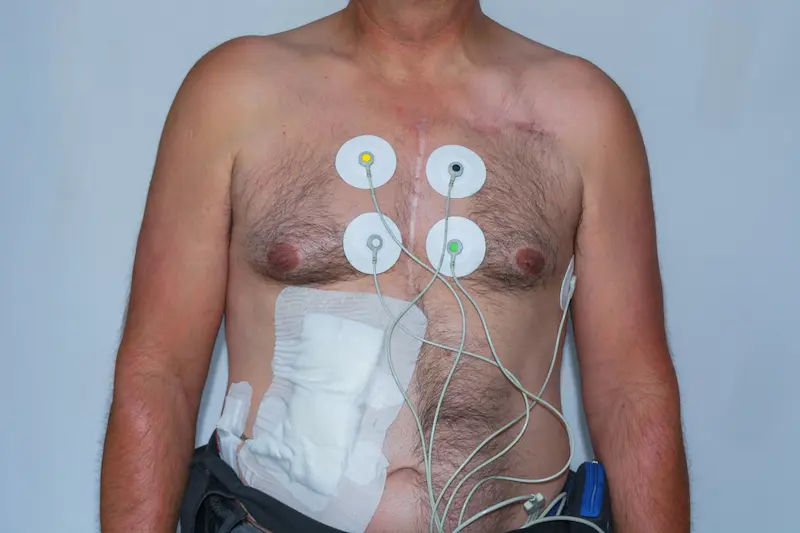
- Rapid or irregular heartbeat
Symptoms Caused by Low White Blood Cells (Neutropenia)
- Frequent infections (bacterial, viral, fungal)
- Fevers and chills
- Sores in the mouth or throat
Symptoms Caused by Low Platelets (Thrombocytopenia)
- Easy or unexplained bruising
- Prolonged bleeding from minor cuts
- Frequent or severe nosebleeds
- Pinpoint red spots on the skin (petechiae)
- Blood in urine or stool
If you are experiencing a combination of these persistent symptoms, it is crucial to consult a doctor for a proper evaluation. You can connect with a haematologist online through Apollo24|7 to discuss your concerns.
How is Bone Marrow Failure Syndrome Diagnosed?
Diagnosis is a multi-step process that begins simply and can become more complex.
The First Step: Complete Blood Count (CBC) and Peripheral Smear
This is the most fundamental test. A CBC measures the number of RBCs, WBCs, and platelets. A peripheral smear allows a pathologist to look at the cells under a microscope for abnormalities in size and shape. Apollo24|7 offers convenient home collection for CBC tests, making this first step easily accessible.
The Gold Standard: The Bone Marrow Biopsy and Aspiration
If the CBC is abnormal, this procedure is essential. A doctor uses a needle to withdraw a small liquid sample (aspirate) and a tiny core of solid bone marrow tissue (biopsy) from the hip bone. This sample is analysed to determine the marrow's cellularity, structure, and the presence of any abnormal cells.
Further Investigations: Genetic and Flow Cytometry Testing
- Genetic Tests: Look for chromosomal abnormalities (like in MDS) or specific genetic mutations (for inherited syndromes).
- Flow Cytometry: A highly sensitive test used to diagnose PNH by detecting the absence of specific proteins on blood cells.
Treatment Options for Managing Bone Marrow Failure
Treatment is highly personalised, depending on the type of BMF, its severity, and the patient's age and health.
Supportive Care: Transfusions and Medications
- This is not a cure but a way to manage symptoms and improve quality of life.
- Blood Transfusions: To boost red blood cell and platelet counts.
- Antibiotics/Antivirals: To prevent and treat infections.
- Growth Factors: Medications like erythropoietin or G-CSF can stimulate the bone marrow to produce more cells.
Immunosuppressive Therapy (IST)
For autoimmune-based Aplastic Anaemia, drugs like antithymocyte globulin (ATG) and ciclosporin are used to suppress the immune system and stop it from attacking the bone marrow.
The Curative Option: Bone Marrow Transplant (Stem Cell Transplant)
This is the only potential cure for many severe BMF syndromes. It involves replacing the diseased bone marrow with healthy stem cells from a donor (allogeneic transplant). The high-dose chemotherapy or radiation given first destroys the faulty marrow, making room for the new, healthy cells to grow.
Living with a Bone Marrow Failure Syndrome
A diagnosis can be overwhelming, but many people live full lives with proper management. This involves:
- Strict Hygiene: Meticulous handwashing to prevent infections.
- Dietary Precautions: Avoiding raw or undercooked foods that might harbour bacteria.
- Avoiding Injury: Being cautious to prevent cuts and bruises.
- Strong Support System: Leaning on family, friends, and support groups.
- Regular Monitoring: Consistent follow-up with a haematologist is non-negotiable.
Conclusion
A diagnosis of a bone marrow failure syndrome is a life-altering event, but it is far from a hopeless one. Medical science has made astounding progress in understanding and treating these complex disorders. From precise diagnostics to innovative treatments like targeted immunosuppression and stem cell transplantation, there are more options for management and cure than ever before. The journey requires a partnership between you and a dedicated medical team, a commitment to self-care, and the support of loved ones. If you suspect you or a family member may be showing signs, the most powerful step you can take is to seek expert medical advice. Your health is your priority. If you have concerns about persistent symptoms like unexplained fatigue or bruising, consult a haematologist online with Apollo24|7 for a professional evaluation and guidance on the next steps.
Consult an Haematologist doctor for the best advice
Consult an Haematologist doctor for the best advice

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)
Dr. Velu Nair
Haematologist
36 Years • MBBS, MD (Med.), FRCP, FACP, FAMS, FICP, FIACM, FUICC, FISHTM
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult an Haematologist doctor for the best advice

Dr Abilash Jain
General Physician/ Internal Medicine Specialist
12 Years • MBBS,DNB(FM),MNAMS,FIAMS,CCGMG(GERIATRICS),DGM (GERIATRICS),PGCD(DIABETES,BOSTON UNIVERSITY),FID(DIABETICS UK)CCEPC(PALLIATIVE CARE),CCCC(CRITICAL CARE)
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(175+ Patients)
Dr. Velu Nair
Haematologist
36 Years • MBBS, MD (Med.), FRCP, FACP, FAMS, FICP, FIACM, FUICC, FISHTM
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad
(25+ Patients)

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
Is bone marrow failure syndrome a type of cancer?
Not always. While some syndromes like MDS are considered pre-leukaemic and can transform into cancer, others, like Aplastic Anaemia, are autoimmune disorders. However, they are all serious conditions treated by haematologists, who are also blood cancer specialists.
What is the life expectancy for someone with Aplastic Anaemia?
With modern treatments like immunosuppressive therapy and bone marrow transplants, the prognosis has improved dramatically. Many patients can achieve long-term survival and a good quality of life. Outcomes depend on age, severity, and response to treatment.
Can bone marrow failure be reversed?
In some cases, yes. A successful bone marrow transplant can effectively cure the condition by replacing the faulty marrow. Immunosuppressive therapy can also induce long-term remission in Aplastic Anaemia by halting the autoimmune attack.
What is the difference between Aplastic Anaemia and leukaemia?
In Aplastic Anaemia, the marrow is empty and fails to produce cells. In leukaemia, the marrow is overrun with cancerous, immature white blood cells that crowd out healthy cell production. They are opposite problems in terms of marrow cellularity.
Are there any known prevention methods for acquired bone marrow failure?
For idiopathic cases (unknown cause), prevention is not possible. However, you can reduce risk by avoiding known environmental toxins like benzene, certain pesticides, and unnecessary exposure to radiation. Always follow safety guidelines when handling chemicals.