Bone Marrow Transplant: Procedure, Donation Process, and Recovery
Understand bone marrow transplant: procedure, donor guide, risks, and recovery. Clear steps, safety tips, and FAQs from trusted medical sources.

Introduction
Facing a serious blood disorder or cancer can be overwhelming. A bone marrow transplant—also called a stem cell transplant—can be a life-saving option for many conditions, from leukaemia and lymphoma to aplastic anaemia and certain inherited disorders. This donor guide explains the bone marrow transplant procedure, how donation works, what to expect during recovery, and how to stay safe afterwards. You’ll find straightforward steps, practical tips, and answers to common questions, grounded in guidance from reputable medical sources.
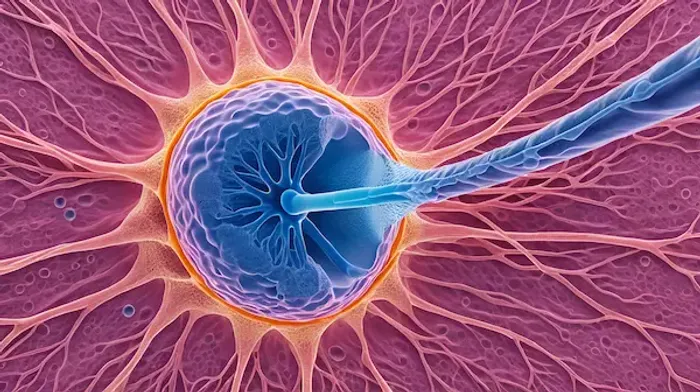
What Is a Bone Marrow Transplant?
A bone marrow transplant (BMT), also known as a haematopoietic stem cell transplant (HSCT), replaces diseased or damaged blood-forming stem cells with healthy ones. These stem cells live in the bone marrow and make red blood cells (carry oxygen), white blood cells (fight infection), and platelets (help clotting).
Healthy stem cells can come from:
- Your own body (autologous transplant), collected and stored before intensive treatment
- A donor (allogeneic transplant), often a relative or a well-matched unrelated volunteer
- An identical twin (syngeneic transplant, uncommon)
The goal is to restore healthy blood and immune cell production after high-dose therapy, and—when using donor cells—to allow the donor immune system to help fight remaining disease.
When Is a Bone Marrow Transplant Recommended?
Doctors may recommend a transplant to:
- Treat blood cancers: leukaemia, lymphoma, multiple myeloma
- Replace failing bone marrow: severe aplastic anaemia, myelodysplastic syndromes
- Correct inherited disorders: sickle cell disease, thalassaemia, certain immune deficiencies
- Manage some autoimmune diseases that do not respond to other treatments (in select cases)
Whether a transplant is appropriate depends on your diagnosis, age, overall health, previous treatments, availability of a suitable donor, and your goals of care. Your transplant team will review risks and benefits tailored to you.
Types of Bone Marrow Transplant and Stem Cell Sources
Here are the types of bone marrow transplant:
- Autologous transplant (your own cells): Your stem cells are collected, stored, and returned after high-dose chemotherapy. This approach reduces immune complications like graft-versus-host disease (GVHD) because the cells are your own. It’s commonly used in multiple myeloma and some lymphomas.
- Allogeneic transplant (donor cells): Cells come from a matched sibling, another relative, or an unrelated volunteer found through registries. Donor cells can attack residual cancer (graft-versus-tumour effect), but there is a risk of GVHD. This approach is used for many leukaemias, bone marrow failure syndromes, and some inherited conditions.
Stem cell sources:
- Peripheral blood stem cells (PBSC): Collected from the bloodstream after a few days of medication to move stem cells out of the marrow. PBSCs are commonly used and often engraft faster.
- Bone marrow: Collected from pelvic bones in an operating room under anaesthesia.
Umbilical cord blood: Stored units collected at birth; helpful when a closely matched donor is not available, though engraftment may take longer.
The Bone Marrow Transplant Procedure: Step by Step
Here’s a step-by-step guide on bone marrow transplant procedure:
Initial Evaluation
Before a transplant, you’ll have a thorough work-up to confirm the plan is safe and appropriate:
- Medical history, physical exam, and review of prior treatments
- Blood tests, heart and lung function tests
- Infection screening (for example, for viruses)
- Imaging as needed (e.g., chest X-ray, scans)
- Placement of a central venous catheter (a special IV line used for treatments)
- For allogeneic transplants: Human leukocyte antigen (HLA) typing to match donors
Conditioning (Pre-Transplant Treatment)
You’ll receive chemotherapy, and sometimes radiation, to:
- Destroy cancer or abnormal cells
- Make room in the marrow for new stem cells
- Suppress the immune system to help donor cells engraft
Conditioning regimens vary in intensity. Reduced-intensity (“mini”) regimens may be used for older adults or those with other health conditions.
Transplant Day (Infusion)
Despite the name, the “transplant” is an infusion of stem cells through your IV line—similar to a blood transfusion. The cells travel to the bone marrow and begin making new blood cells. If your cells were frozen, you may notice a brief taste or smell related to the preservative during infusion.
Engraftment and Early Recovery
“Engraftment” means the new cells are growing and your blood counts are rising. This usually happens over the next few weeks. During this time:
- You’ll be closely monitored for infections, bleeding, and side effects
- You may receive antibiotics, antivirals, antifungals, and transfusions
- If you had an allogeneic transplant, you’ll take medicines to prevent GVHD
Some centres perform parts of autologous transplants as outpatient care; others require a hospital stay. Plan for frequent visits and blood tests for weeks to months.
Consult Top Specialists
Bone Marrow Transplant Donor Guide: How Donation Works
Becoming a donor can save a life. Here’s what to know if you’re interested or you’ve been asked to donate.
Matching and Registries
- Matching is based on HLA typing—proteins on white blood cells that help the immune system recognise “self”. A close HLA match lowers the risk of serious immune reactions.
- Many donors are relatives, but most patients rely on volunteer registries. If you’d like to register, a simple cheek swab is typically used to add your HLA type to a database so you can be found if you match someone in need.
Donor Eligibility
- Donors are generally adults in good health. Medical history and screening blood tests ensure donation is safe for you and the recipient.
- Certain conditions, recent infections, or medications may affect eligibility. The transplant team will provide individualised guidance.
Two Ways to Donate
Peripheral blood stem cells (PBSC): The most common method for allogeneic donation.
- Before donation: You receive daily injections for several days to move stem cells from your marrow into your bloodstream.
- Collection: Blood is drawn from one arm, stem cells are separated in a machine, and the rest of your blood is returned to your other arm. This process (apheresis) usually takes several hours and may occur over one or two days.
- Side effects: Temporary bone or muscle aches, fatigue, and headache are possible; these typically resolve shortly after donation.
Bone marrow harvest:
- Procedure: In an operating room under anaesthesia, doctors draw marrow from the back of the pelvic bones using needles.
- Recovery: Most donors go home the same day. You may have soreness in the lower back and feel tired for a few days.
Both methods have been used safely for decades. Serious complications are uncommon, and the body replenishes donated cells.
Donor Safety and Follow-Up
- Donor safety is the top priority. You’ll have a medical check-up before donation and follow-up afterwards.
- Costs related to donation for an identified patient are typically covered by the recipient’s insurance or the transplant programme; if you register as a volunteer donor, the registry coordinates logistics and coverage.
- You can ask questions, and you are free to withdraw at any time before the recipient begins their pre-transplant conditioning.
Risks and Possible Side Effects
Your transplant team will explain risks specific to your situation. Possible short-term effects include:
- Nausea, vomiting, mouth sores, diarrhoea
- Hair loss, skin rashes
- Fatigue and weakness
- Low blood counts with increased risk of infection and bleeding
- Organ side effects from chemotherapy or radiation (for example, liver or lung irritation)
Possible longer-term effects can include:
- Infections while the immune system recovers
- Graft-versus-host disease (GVHD) after an allogeneic transplant, where donor immune cells attack the recipient’s tissues (skin, gut, liver, eyes, and others). Medicines are used to help prevent and treat GVHD.
- Fertility changes; discuss sperm, egg, or embryo preservation before treatment if future fertility is important to you
- Hormone changes (thyroid, adrenal), bone loss, cataracts, heart or lung effects
- Rarely, secondary cancers years later
Your care team will monitor you closely and provide treatments and preventive strategies to reduce risks whenever possible.
Recovery and Life After Transplant
Recovery is a journey. While experiences vary, here’s what many people can expect.
The First Weeks to Months
- Blood counts usually improve over weeks, but full immune recovery can take many months. Follow your team’s guidance on masks, visitors, and activities.
- Infection prevention:
- Wash hands often and ask visitors to do the same
- Avoid sick contacts and crowded indoor spaces early on
- Follow food safety rules: avoid undercooked meats, unpasteurised dairy, and unwashed produce; pay attention to kitchen hygiene
- Medicines: You may take antibiotics and antivirals for a period of time, plus drugs to prevent GVHD if you had an allogeneic transplant.
- Vaccinations: The immune system often needs to be re-vaccinated after transplant. Your team will provide a schedule, typically starting several months after transplant when your counts are stable.
- Nutrition and activity: Eat small, protein-rich meals if your appetite is low. Gentle activity—such as short walks—can improve strength and mood. Ask for a referral to nutrition and physical therapy as needed.
Returning to Daily Life
- Work or school: Timing varies. Some people resume light duties within a few months; others need longer. Discuss a gradual return plan with your clinicians.
- Mental health: It’s common to feel anxious, low, or overwhelmed. Ask about counselling, peer support, or patient navigator programmes.
- Sun protection: Use sunscreen and protective clothing; certain medicines and GVHD can make skin more sensitive.
- Ongoing monitoring: Expect frequent follow-ups, especially in the first year, to check blood counts, organ health, and any signs of GVHD or infection.
Practical Tips to Prepare
- Get your home ready: Clean and declutter high-touch areas; stock easy-to-prepare foods.
- Line up support: Arrange help with rides, childcare, pets, and errands. Identify a caregiving partner if your centre requires one.
- Dental check-up: Address any dental issues before conditioning to reduce infection risk.
- Fertility and family planning: Discuss options before treatment if relevant.
- Vaccination review: Household members should be up to date on vaccines based on public health guidance; your team will advise about any specific precautions.
Consult Top Specialists
Consult Top Specialists

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr. B Shravanthi Reddy
Radiation Specialist Oncologist
8 Years • MBBS, DNB(Radiation Oncology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
Dr. Amit Kumar Jain
Medical Oncologist
7 Years • MBBS, MD, Dr. NB (Medical Oncology)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru
Consult Top Specialists

Dr.sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
Dr. Sanchayan Mandal Oncology Clinic, Kolkata

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Dr. B Shravanthi Reddy
Radiation Specialist Oncologist
8 Years • MBBS, DNB(Radiation Oncology)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
Dr. Amit Kumar Jain
Medical Oncologist
7 Years • MBBS, MD, Dr. NB (Medical Oncology)
Bengaluru
Apollo Clinic, Indiranagar, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
Is a bone marrow transplant the same as a stem cell transplant?
Yes. The medical term is hematopoietic stem cell transplant. Stem cells can be collected from bone marrow, the bloodstream (PBSC), or umbilical cord blood. Many people still say “bone marrow transplant” even when cells come from the bloodstream.
Who can be a donor, and how do I register?
Adults in good health can often register as volunteer donors with a cheek swab. If matched to a patient, you’ll have a health screening to make sure donation is safe for you. Family members may be tested when a relative needs a transplant. Your transplant center or a national registry can guide you through the process.
How long does recovery take after transplant?
Blood counts usually recover over weeks, but strength and immune recovery can take months. The timeline depends on your diagnosis, transplant type (autologous vs allogeneic), stem cell source, and overall health. Your team will give you specific milestones and safety guidelines.
What is graft-versus-host disease (GVHD), and can it be prevented?
GVHD can occur after an allogeneic transplant when donor immune cells react against the recipient’s tissues. It can affect the skin, gut, liver, eyes, and other organs. Doctors reduce risk by carefully matching donors and giving immune-suppressing medicines before and after transplant. Prompt reporting of symptoms—such as new rashes, severe diarrhea, or yellowing of the eyes—helps ensure early treatment.
Will a bone marrow transplant cure my disease?
For some conditions, transplant offers the best chance of long-term control or cure. Outcomes vary by disease type, stage, genetics of the disease, your health, the donor match, and the center’s experience. Your transplant team can discuss expected results for your specific situation.




