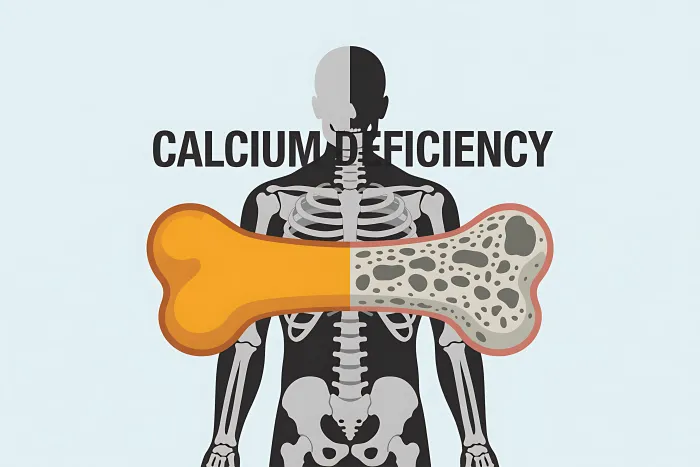
Calcium Deficiency: Signs, Symptoms, and Health Risks
Calcium deficiency explained: signs, risks, testing, foods, and safe supplements to protect bone health at every age.

Introduction: Why This Topic Matters
Calcium is essential for strong bones and for many everyday body functions, from muscle movement to nerve signalling. Yet a large number of people do not meet their daily needs, which can increase the long-term risk of weakened bones, fractures and reduced quality of life. Understanding calcium deficiency—what it is, how it develops, who is most vulnerable and how to prevent it—helps you take practical steps to safeguard bone health throughout your lifespan. Calcium deficiency often progresses silently, so learning the early indicators and ways to optimise your intake can make a genuine difference to your health and wellbeing.Consult a Top General Practitioner for Personalised Advice
What Is Calcium Deficiency?
Calcium deficiency occurs when the body does not get, absorb or use enough calcium. It can appear in two main forms:
- Low calcium in the blood (hypocalcaemia): This is often linked to certain medical conditions or medications and may trigger noticeable symptoms.
- Low calcium intake over time: Blood calcium may still appear normal because the body pulls calcium from the bones to keep blood levels stable, which gradually weakens bone structure.
Calcium’s Role in Bone Health and Beyond
The role of calcium in bone health and more is:
- Bones and teeth: Around 99% of the body’s calcium is stored in bones and teeth, providing firmness and structure.
- Muscle and nerve function: Calcium is essential for muscle contraction and the effective transmission of nerve signals.
- Blood clotting and heart rhythm: It plays a vital role in blood clotting processes and helps maintain a steady heart rhythm.
Signs and Symptoms of Calcium Deficiency
Signs and symptoms of calcium deficiency include:
Early or Mild Symptoms
These are often related to low blood calcium and can be subtle at first; they include:
- Numbness or tingling in the lips, tongue, fingers or feet
- Muscle cramps, spasms or twitching
- Fatigue, low energy or generalised weakness
Severe or Prolonged Deficiency Symptoms
If calcium remains low for a long time, symptoms may become more pronounced:
- Seizures or heart rhythm abnormalities in cases of severe hypocalcaemia
- Brittle bones and an increased risk of fractures from minor falls
- Rickets in children, where bones become soft and poorly mineralised
Symptoms can vary significantly depending on the cause and how long the deficiency has been present. Medical care is essential if you develop persistent tingling, muscle spasms or signs of a fracture.
Health Risks Linked to Calcium Deficiency
Health risks linked to calcium deficiency include:
- Osteopenia and osteoporosis: Reduced bone mineral density leads to weaker bones and a greater risk of fractures.
- Fragility fractures: Breaks caused by low-impact incidents can greatly affect mobility and long-term independence.
- Rickets (children) and osteomalacia (adults): Long-term low calcium or vitamin D can lead to soft, weak bones.
- Dental issues: Inadequate calcium over time can weaken tooth enamel and increase susceptibility to decay.
- Severe hypocalcaemia: May lead to life-threatening complications, including seizures or abnormal heart rhythms.
Who Is at Higher Risk?
High-risk people or situations include:
- Postmenopausal women and adults over 70 due to accelerated bone loss
Adolescents undergoing rapid growth - People with low dietary intake or those who avoid dairy or fortified foods
- Individuals with lactose intolerance or milk allergies
- Vegans and those on restrictive diets without suitable alternatives
- People with malabsorption conditions such as coeliac disease or inflammatory bowel disease
- Those with low vitamin D levels, which reduces calcium absorption
- People taking certain medications, including long-term steroids, anti-seizure drugs or loop diuretics
- Those with kidney or parathyroid disorders that directly influence calcium balance
How Is Calcium Deficiency Diagnosed?
Healthcare professionals may use several approaches. The diagnosis includes:
- Medical history and diet review to assess calcium and vitamin D intake
- Blood tests to measure serum or ionised calcium, albumin, parathyroid hormone, vitamin D, magnesium and kidney function
- Bone density testing (DXA scan) to evaluate bone strength and fracture risk
Get Your Symptoms Assessed
It is important to note that blood calcium may remain normal even when dietary intake is consistently low, because the body compensates by pulling calcium from the bones.
Daily Calcium Needs and Safe Upper Limits
The daily calcium needs and safety limits include:
General Recommendations for Adults
- Ages 19–50: 1,000 mg/day
- Men 51–70: 1,000 mg/day
- Women 51–70: 1,200 mg/day
- Adults 71+: 1,200 mg/day
Safe Upper Limits
- Ages 19–50: 2,500 mg/day
- Ages 51+: 2,000 mg/day
Regularly exceeding these limits, especially through supplements, should be avoided without medical guidance.
Food-First Approach: Top Calcium Sources
Meeting your calcium needs through food offers additional nutrients that support bone strength and overall well-being. It includes:
Dairy and Fortified Foods
- Milk, yoghurt and cheese
- Fortified plant-based milks such as soy, almond and oat
- Fortified juices and cereals (check labels for calcium content)
Plant-Based and Other Options
- Leafy greens, including kale, bok choy and collards
- Tofu made with calcium sulphate
- Canned sardines or salmon with edible bones
- Almonds, chia seeds and sesame/tahini
- Beans and lentils, which add additional bone-supportive nutrients
Tips to Boost Absorption
Tips to boost absorption are:
- Pair calcium foods with vitamin D, as it enhances absorption.
- Moderate foods high in oxalates, like spinach or beet greens, since they reduce calcium absorption.
- Spread your calcium intake across the day, as the body absorbs moderate doses more efficiently.
When Calcium Supplements Make Sense?
Supplements may be helpful if:
- Your diet does not supply enough calcium due to intolerance, allergy or preference
- You have increased needs or reduced absorption
- A clinician recommends supplementation based on tests or bone density results
Choosing a Supplement
- Calcium carbonate: Cost-effective and best absorbed with meals.
- Calcium citrate: Suitable with or without food and is gentler on the stomach.
- Take no more than 500 mg at once for optimum absorption.
- Select products with reliable third-party testing where possible.
Safety and Interactions
Safety and interaction tips include:
- Do not exceed recommended limits, especially with supplements, as excess may increase kidney stone risk.
- Take calcium separately from iron supplements, thyroid medication, some antibiotics and certain osteoporosis medicines.
- Speak with a clinician if you have kidney stones, heart issues, kidney disease or parathyroid disorders.
Lifestyle Habits That Support Bone Health
Lifestyle habits that help in bone health are:
- Engage in weight-bearing and resistance exercises such as walking, stair climbing and strength training.
- Ensure adequate vitamin D through food, supplements or safe sun exposure.
- Maintain a balanced diet with protein, fruits, vegetables and magnesium-rich foods.
- Avoid smoking and reduce alcohol intake, as both weaken bones.
- Monitor sodium and high caffeine intake, as excessive amounts may increase calcium loss.
When to See a Healthcare Professional
Seek professional help:
- If you experience symptoms such as persistent tingling, muscle cramps or spasms
- If you are at higher risk due to age, medical conditions or medication use
- If you have experienced a low-impact fracture or noticeable height loss
- If you are considering supplements and want personalised recommendations
- If you have concerns about a child’s growth or signs of rickets
Conclusion
Calcium is vital for maintaining strong bones, stable nerve function and healthy muscles, yet many people do not achieve the recommended daily intake. Understanding calcium deficiency and taking early steps—such as improving diet, ensuring adequate vitamin D and engaging in bone-strengthening activities—can significantly reduce long-term risks like osteoporosis and fractures. A balanced, food-first approach is ideal, with supplements used when necessary under guidance. Paying attention to symptoms and risk factors allows you to safeguard your bone health and support overall well-being throughout life.Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Dhankecha Mayank
General Practitioner
6 Years • MBBS
Hyderabad
Apollo 24|7 Clinic - Telangana, Hyderabad

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Md Yusuf Shareef
General Practitioner
8 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
Consult a Top General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Dhankecha Mayank
General Practitioner
6 Years • MBBS
Hyderabad
Apollo 24|7 Clinic - Telangana, Hyderabad

Dr Suseela
General Physician
5 Years • MBBS
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Md Yusuf Shareef
General Practitioner
8 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
More articles from General Medical Consultation
Frequently Asked Questions
1) What Is the Difference Between Calcium Deficiency and Hypocalcaemia?
Calcium deficiency generally means long-term inadequate intake that can weaken bones, while hypocalcaemia is a low level of calcium in the blood at the current moment, which may require urgent treatment. A person can have normal blood calcium yet still have a low dietary intake that harms bone health.
2) Do I Need a Calcium Supplement If I Eat a Balanced Diet?
Many people can meet their needs through food alone, especially those who consume dairy or fortified products. If your diet is limited or you have increased needs, a supplement may be useful. A clinician or dietitian can assess your diet and guide you.
3) What Are the Best Foods to Prevent Calcium Deficiency?
Dairy products, fortified plant milks and juices, tofu made with calcium sulphate, canned fish with bones and certain leafy greens such as kale or bok choy.
4) Can Too Much Calcium Be Harmful?
Yes. Exceeding the upper limit, especially through supplements, can increase the risk of kidney stones and may cause constipation. Aim to meet your needs without over-supplementing.
5) How Does Vitamin D Affect Calcium and Bone Health?
Vitamin D is essential for calcium absorption. Even adequate calcium may not be enough for bone strength if vitamin D is low. Your clinician can check your vitamin D status and recommend safe ways to correct it.


.webp)

 Ayurvedic Benefits, Nutrition, and Side Effects.webp)
