Common Causes of Recurring Stomach Pain and When to See a Doctor
Understand common stomach pain causes, what recurring pain means, and when to see a doctor. Trusted digestive health tips, warning signs, and FAQs.

Written by Dr. Siri Nallapu
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
Most people have a tummy ache now and then. But when abdominal discomfort keeps coming back, it can interrupt work, sleep, and daily life—and leave you worrying about what’s going on. Understanding common stomach pain causes can help you know what to try at home, what to track, and when it’s time to see a clinician. This guide offers clear, trustworthy information to support your digestive health, with practical tips and warning signs you shouldn’t ignore.
What do doctors mean by “stomach pain”?
Many of us say “stomach pain” to describe any discomfort in the area between the chest and groin (the abdomen). The true stomach is in the upper middle-left area under the ribs, but pain can come from many organs: stomach, intestines, esophagus, gallbladder, pancreas, liver, kidneys, bladder, uterus/ovaries, and abdominal muscles.
Pain can feel sharp, crampy, burning, dull, or like pressure. It may be steady or come and go. Noticing where the pain is, what triggers it (such as meals or stress), and what helps it settle can offer helpful clues to your clinician.
Common stomach pain causes that come back
Recurring or on-and-off abdominal pain often has more than one contributing factor. Below are frequent causes seen in primary care and gastroenterology. Keep in mind that symptoms can overlap, and similar pains can have different causes in different people.
Functional gastrointestinal disorders (including IBS)
- What it is: Conditions where the GI tract looks normal on tests but doesn’t function normally. Irritable bowel syndrome (IBS) is the most common, causing belly pain along with changes in bowel habits (diarrhea, constipation, or both).
- Typical clues: Pain improves after having a bowel movement; bloating; symptom flare-ups with certain foods or stress.
- What helps: Food and symptom tracking; gradual fiber changes as tolerated; stress management; clinician-guided diets (such as a time-limited, supervised low-FODMAP plan); medications if needed.
Acid reflux and GERD
- What it is: Stomach acid flowing back into the esophagus. When it’s frequent and bothersome, it’s called gastroesophageal reflux disease (GERD).
- Typical clues: Burning pain behind the breastbone or upper abdomen, sour taste in the mouth, symptoms after large or late meals, lying down soon after eating, or certain trigger foods.
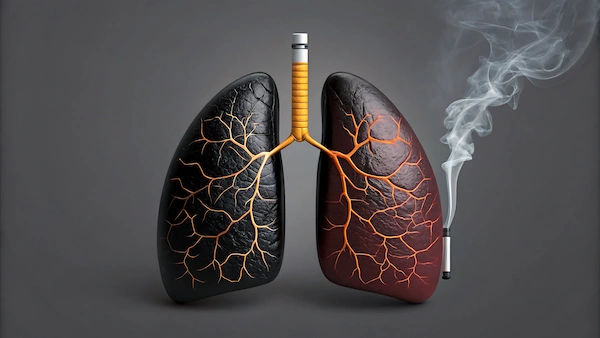
- What helps: Smaller meals, not lying down for 2–3 hours after eating, weight management if advised by your clinician, avoiding individual trigger foods and tobacco. Antacids or acid-reducing medicines may help; ask your clinician about safe use.
Peptic ulcers and gastritis
- What it is: Sores in the stomach or upper small intestine (peptic ulcers), or irritation of the stomach lining (gastritis). Common causes include Helicobacter pylori infection and frequent use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen.
- Typical clues: Burning or gnawing upper abdominal pain, often between meals or at night; nausea; feeling full quickly. Red flags include vomiting blood or black, tarry stools.
- What helps: Testing and treatment for H. pylori if present; reviewing pain reliever use; acid-suppressing medicines as directed; avoiding tobacco and limiting alcohol. Seek prompt care for bleeding symptoms or severe pain.
Gallbladder problems (gallstones)
- What it is: Hardened deposits in the gallbladder that can block bile flow.
- Typical clues: Pain in the right upper abdomen, often after a fatty meal; pain that may spread to the right shoulder or back; nausea. Fever and severe, lasting pain suggest possible gallbladder inflammation and need urgent care.
- What helps: Evaluation and imaging (often an ultrasound). Some cases are managed with surgery; your clinician will advise.
Pancreatitis
- What it is: Inflammation of the pancreas, sometimes linked to gallstones or alcohol.
- Typical clues: Severe pain in the upper abdomen that may radiate to the back; worsens after eating; nausea and vomiting.
- What helps: This is a medical urgency or emergency—seek care right away.
Food intolerances and celiac disease
- Lactose intolerance: Bloating, gas, cramps, and diarrhea after dairy. Solutions include adjusting lactose intake, using lactose-free products, or enzyme tablets.
- Celiac disease: An immune reaction to gluten that damages the small intestine. Symptoms can include abdominal pain, diarrhea, weight loss, fatigue, and anemia—or be subtle. Diagnosis requires specific blood tests and often an intestinal biopsy. Do not start a gluten-free diet before testing, as it can affect results.
Inflammatory bowel disease (IBD)
- What it is: Chronic inflammation of the GI tract—Crohn’s disease and ulcerative colitis.
- Typical clues: Ongoing or recurrent abdominal pain, diarrhea, blood in the stool, fatigue, weight loss.
- What helps: Medical evaluation and long-term treatment plan with a specialist.
Constipation
- What it is: Difficult or infrequent bowel movements that can cause cramping and pressure.
- Typical clues: Straining, hard or lumpy stools, a sense of incomplete emptying, less frequent bowel movements than usual.
- What helps: Fluids, dietary fiber as tolerated, physical activity, routine bathroom habits. Discuss safe laxative use with your clinician if needed.
Urinary and gynecologic conditions
- Urinary tract infections: Pelvic or lower abdominal pain, burning with urination, frequent urination, sometimes blood in urine.
- Kidney stones: Sudden, severe pain in the back or side that can move to the lower abdomen/groin; nausea; blood in urine.
- Menstrual cramps, endometriosis, or ovarian cysts: Can cause recurring lower abdominal or pelvic pain. Sudden severe pain or pain with fever, vomiting, or fainting needs urgent evaluation.
- If you could be pregnant: Severe abdominal pain or pain with vaginal bleeding should be treated as urgent.
Infections and foodborne illness
Acute episodes of cramping, diarrhea, and vomiting are often due to viruses or bacteria in food or water. If episodes repeat, consider potential recurring exposures or other underlying causes with your clinician.
Medicines and supplements
- NSAIDs and some other medicines can irritate the stomach and intestines.
- Antibiotics can sometimes trigger infections like Clostridioides difficile, which causes significant diarrhea and abdominal pain. Seek care if you develop severe or persistent diarrhea after antibiotics.
Stress and the gut-brain connection
Stress, anxiety, and poor sleep can amplify gut symptoms—even when there is no structural disease—by affecting how the gut and brain communicate. Stress management, counseling, and mind–body approaches can be helpful parts of a treatment plan.
Consult Top Specialists
When to see a doctor—and when to go now?
Call your primary care clinician soon if you have:
- Abdominal pain that keeps coming back, interferes with daily life, or lasts more than a few days
- New or worsening symptoms, especially if you’re over age 55
- Unexplained weight loss, changes in bowel habits, or persistent bloating
- Pain related to a new medicine
- Ongoing heartburn or indigestion more than twice a week
Seek urgent or emergency care if you have:
- Severe, sudden, or worsening pain, or pain with a rigid/tender belly
- Fever, repeated vomiting, or signs of dehydration (very dry mouth, dizziness, very dark urine, little or no urination)
- Vomit that looks like coffee grounds, blood in vomit, black/tarry or bloody stools
- Yellowing of the skin or eyes (jaundice)
- Chest pain, shortness of breath, or fainting with abdominal pain
- You might be pregnant and have abdominal pain or vaginal bleeding
- Pain after a significant injury to the abdomen
How do clinicians find the cause?
Your clinician will start with a careful history and exam. Depending on your symptoms, you may have:
- Blood tests (for infection, inflammation, anemia, liver or pancreatic enzymes)
- Urine tests; pregnancy test when appropriate
- Stool tests (for infection, inflammation, or blood)
- Tests for H. pylori if ulcer is suspected
- Imaging (ultrasound, X-ray, CT scan) when needed
- Endoscopy or colonoscopy in specific cases
It’s common to try treatment steps while testing proceeds. Keep track of symptoms, food, medications, and stressors—this can speed a correct diagnosis.
Everyday steps to support digestive health
Small, steady changes can make a big difference. Try:
- Eat regular, balanced meals. Notice your personal triggers (for example, very fatty, spicy, or highly processed foods) and adjust.
- Fiber, as tolerated. Slowly increase fiber from foods like fruits, vegetables, beans, nuts, and whole grains; drink enough fluids so fiber can work well.
- Space meals and sleep. Avoid lying down within 2–3 hours after eating; consider smaller portions if large meals trigger symptoms.
- Stay hydrated. Water supports digestion and stool regularity.
- Move your body. Regular physical activity helps bowel regularity and stress levels.
- Be careful with pain relievers. Use NSAIDs only as advised. Ask about alternatives if you need frequent pain relief.
- Limit alcohol and avoid tobacco. Both can irritate the digestive tract.
- Manage stress and sleep. Relaxation exercises, mindfulness, counseling, and good sleep habits can reduce symptom flare-ups in some conditions.
- Consider probiotics with guidance. Some people with IBS find benefit from certain probiotic strains; discuss options with your clinician.
Remember: There isn’t one diet or remedy that fits everyone. Work with your clinician or a registered dietitian to tailor a plan to your needs.
Putting it together
Recurring abdominal discomfort is common—and most causes are manageable once identified. Paying attention to patterns, addressing lifestyle factors, and seeking timely medical advice are the best ways to protect your digestive health. If you notice red flags, don’t wait; early care can prevent complications.
Consult Top Specialists
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ramya Hari
General Practitioner
18 Years • Medical Head & Family Physician, DG Shipping Approved Doctor, Panel Physician - UK Visa Medicals
Chennai
Apollo Medical Centre Kotturpuram, Chennai

Dr. S Ananth Kumar
General Physician/ Internal Medicine Specialist
41 Years • MBBS; MD
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(125+ Patients)

Dr. Mohammed Sharouk Khader
General Physician/ Internal Medicine Specialist
11 Years • MBBS, Bach. of Med. & Surg., Dip. of American Board of Family Med.
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)
Dr. Indrajit Das
General Physician/ Internal Medicine Specialist
4 Years • "MD (Internal medicine) : Gauhati Medical College and Hospital, Guwahati (2018-2021) MD (Pathology) : Gauhati Medical College and Hospital, Guwahati (2012-2015) MBBS (Bachelor of Medicine, Bachelor of Surgery) : Silchar Medical College, Assam (2003-2008) "
Guwahati
Apollo Excelcare Hospital, Guwahati
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ramya Hari
General Practitioner
18 Years • Medical Head & Family Physician, DG Shipping Approved Doctor, Panel Physician - UK Visa Medicals
Chennai
Apollo Medical Centre Kotturpuram, Chennai

Dr. S Ananth Kumar
General Physician/ Internal Medicine Specialist
41 Years • MBBS; MD
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(125+ Patients)

Dr. Mohammed Sharouk Khader
General Physician/ Internal Medicine Specialist
11 Years • MBBS, Bach. of Med. & Surg., Dip. of American Board of Family Med.
Chennai
Apollo Hospitals Greams Road, Chennai
(125+ Patients)
Dr. Indrajit Das
General Physician/ Internal Medicine Specialist
4 Years • "MD (Internal medicine) : Gauhati Medical College and Hospital, Guwahati (2018-2021) MD (Pathology) : Gauhati Medical College and Hospital, Guwahati (2012-2015) MBBS (Bachelor of Medicine, Bachelor of Surgery) : Silchar Medical College, Assam (2003-2008) "
Guwahati
Apollo Excelcare Hospital, Guwahati
More articles from General Medical Consultation
Frequently Asked Questions
What’s the difference between stomach pain and abdominal pain?
People often use the terms interchangeably. Abdominal pain refers to discomfort anywhere between your chest and groin, which includes many organs. True stomach pain is located in the upper middle-left area under the ribs. Because many organs can cause similar symptoms, it’s best to describe where the pain is, what it feels like, and what affects it.
Can stress or anxiety really cause stomach pain?
Yes. The gut and brain communicate closely, so stress and anxiety can trigger or worsen symptoms like cramping, bloating, and bowel changes, especially in conditions like IBS. That said, ongoing or severe pain still deserves a medical evaluation to rule out other causes.
Are there safe home remedies for mild recurring pain?
For mild, familiar symptoms without red flags, people often find relief with:
- Heat (a warm pack) on the abdomen
- Hydration and smaller, lighter meals
- Limiting known trigger foods and alcohol
- Gentle activity and stress-reduction techniques
- If pain persists, returns frequently, or worsens, check in with your clinician.
Is pain after eating normal?
Occasional fullness after a big meal is common, but repeated pain after eating may point to reflux/GERD, ulcers, gallbladder issues, food intolerances, or other conditions. Track which foods or meal sizes trigger symptoms and share this with your clinician.
Should I take antacids or acid reducers for recurring pain?
Short-term use of over-the-counter antacids or acid-reducing medicines can help reflux or ulcer-like symptoms. However, frequent or long-term use should be guided by a clinician to avoid masking a condition that needs evaluation and to ensure medicines are used safely.