Foods to Avoid While Taking Pantoprazole
Learn which foods to avoid on a pantoprazole diet for better acid reflux management. Evidence-based tips, safe swaps, and FAQs to feel better fast.

Written by Dr. Vasanthasree Nair
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Pantoprazole is a proton pump inhibitor (PPI) commonly prescribed for acid reflux, GERD, and stomach ulcers. While it reduces stomach acid and helps healing, what you eat still matters. The right pantoprazole diet can reduce breakthrough symptoms, prevent triggers, and support long-term acid reflux management. This guide explains which foods to avoid or limit, what to eat instead, and simple daily habits that make your treatment work better.
How pantoprazole works and why food still matters?
Pantoprazole lowers the amount of acid your stomach makes, which helps calm heartburn and allows irritated tissue to heal. But certain foods can still relax the lower esophageal sphincter (LES), slow stomach emptying, or irritate the lining—leading to reflux despite medication. Pairing pantoprazole with smart eating habits gives you the best chance at steady relief.
Tips to get the most from your medicine:
- Take pantoprazole 30–60 minutes before a meal (often before breakfast) as directed by your clinician.
- Swallow tablets whole; do not crush or chew. If swallowing is hard, ask about other formulations.
- Use antacids for occasional “breakthrough” heartburn if your clinician says they’re safe for you.Keep a symptom diary to spot your personal triggers.
Foods to avoid or limit on a pantoprazole diet
Food triggers vary from person to person. The items below are commonly linked with reflux symptoms. Try limiting them for 2–3 weeks while on pantoprazole, then reintroduce one at a time to identify your unique triggers.
High-fat and fried foods
- Examples: fried chicken, french fries, fatty cuts of meat, bacon, sausage, creamy sauces, rich pastries.
- Why: High-fat meals can relax the LES and slow stomach emptying, increasing the chance of reflux.
Spicy foods
- Examples: hot peppers, chili, curry, dishes heavy in cayenne or chili flakes.
- Why: Spicy ingredients can irritate the esophagus and worsen heartburn for many people.
Chocolate, coffee, and caffeinated drinks
- Examples: chocolate bars, hot cocoa, coffee (regular and decaf), black tea, energy drinks.
- Why: Chocolate and caffeine can relax the LES. Coffee (even decaf) and some teas may be acidic or irritating for some people.
Carbonated beverages
- Examples: soda, seltzer, sparkling water, kombucha.
- Why: Bubbles expand in the stomach, increasing pressure and the likelihood of reflux.
Citrus fruits and juices
- Examples: oranges, grapefruits, lemons, limes, orange juice, lemonade.
- Why: These are acidic and can irritate the esophagus.
Tomato products
- Examples: marinara, ketchup, salsa, tomato soup, pizza sauce.
- Why: Tomatoes are acidic and commonly trigger heartburn.
Peppermint and spearmint
- Examples: mint tea, candies, gums, mint-flavored desserts.
- Why: Mint can relax the LES, making reflux more likely.
Alcohol
- Examples: wine, beer, cocktails, spirits.
- Why: Alcohol can irritate the lining and relax the LES. Even small amounts can trigger symptoms in sensitive people.
Onions and garlic (for some)
- Why: These are common triggers for some individuals, especially when eaten raw.
Large or late-night meals
- Why: Big portions stretch the stomach. Eating within 2–3 hours of lying down raises the chance of nighttime reflux.
What to eat instead: gentle, reflux-friendly swaps?
You don’t need a restrictive diet. Most people feel better by choosing lower-fat, lower-acid options and watching portions. Try these swaps:
- Proteins: grilled chicken or turkey, fish, tofu, eggs, beans and lentils (as tolerated), lean ground meats.
- Grains: oatmeal, brown rice, quinoa, whole-grain bread or pasta (in moderate portions).
- Fruits: bananas, melons, apples, pears, berries (as tolerated).
- Vegetables: leafy greens, broccoli, green beans, zucchini, cucumbers, carrots, sweet potatoes.
- Dairy: low-fat or fat-free yogurt, milk, or lactose-free options; choose lower-fat cheeses.
- Fats: small amounts of olive oil, avocado, nuts and seeds (if tolerated).
- Drinks: water, non-mint herbal teas (e.g., ginger or chamomile), non-citrus smoothies.
- Snacks: plain crackers with hummus, rice cakes with nut butter, yogurt with berries, oatmeal cups.
Consult Top Specialists
Practical meal ideas
- Breakfast: oatmeal topped with banana and a sprinkle of chia seeds; chamomile tea.
- Lunch: grilled chicken salad with leafy greens, cucumber, carrots, olive oil–vinegar dressing; whole-grain roll.
- Dinner: baked salmon, steamed broccoli, quinoa.
- Snacks: apple slices with almond butter; low-fat yogurt; a handful of unsalted nuts (if tolerated).
Smart timing and portions for acid reflux management
- Take pantoprazole 30–60 minutes before a meal, as prescribed.
- Eat smaller, more frequent meals instead of large ones.
- Avoid eating 2–3 hours before bed.
- Maintain a healthy weight; even modest weight loss can reduce reflux.
- Wear looser clothing around your abdomen.
- Elevate the head of your bed 6–8 inches for nighttime symptoms.
- Don’t smoke or vape; nicotine relaxes the LES and worsens reflux.
Does pantoprazole interact with foods?
Pantoprazole does not have major food interactions. It’s typically taken before a meal for best effect. The main goal is to avoid foods that trigger your symptoms, not because they “inactivate” the medication, but because they can still cause reflux despite acid suppression.
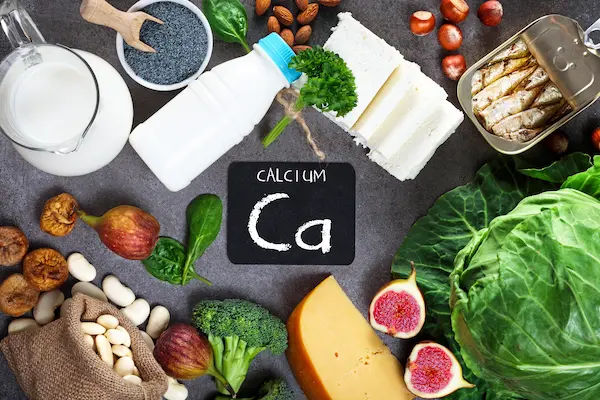
Special considerations if you use pantoprazole long-term
- Talk with your clinician if you’ve been on a PPI for many months. Long-term use has been associated with certain nutrient issues and risks in some people. Your care team may:
- Check magnesium and vitamin B12 levels if you have symptoms of deficiency or use PPIs long term.
- Review bone health and calcium/vitamin D intake, especially if you have osteoporosis risk.
- Reassess dose and duration to use the lowest effective dose for symptom control.
When to seek medical care?
Contact your healthcare provider promptly if you have any of the following:
- Trouble swallowing, food getting stuck, or painful swallowing
- Unexplained weight loss, persistent vomiting, or black/tarry stools
- Chest pain or pressure (seek emergency care to rule out heart causes)
- Severe or persistent symptoms despite medication
Putting it together: a practical pantoprazole diet plan
- Step 1: Take pantoprazole as directed, ideally 30–60 minutes before breakfast.
- Step 2: For 2–3 weeks, limit common triggers: high-fat/fried foods, spicy dishes, chocolate, coffee/caffeine, carbonated drinks, citrus and tomato products, mint, alcohol, and very large or late meals.
- Step 3: Build meals around lean proteins, whole grains, fruits and vegetables lower in acid, and lower-fat dairy.
- Step 4: Reintroduce one potential trigger per week to identify what you personally tolerate.
- Step 5: Keep up lifestyle steps—smaller portions, earlier dinners, head-of-bed elevation—so your acid reflux management plan works day and night.
Consult Top Specialists
Consult Top Specialists

Dr Haripriya S G
Family Physician
22 Years • MBBS, PGD (Family Medicine)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Ms. Sreeparna Dey Dhara Deb
Dietician
10 Years • DNHE
Bansdroni
Siddhita Healthcare., Bansdroni

Ms. Malabika Datta
Dietician
17 Years • Msc. in Dietetics & Food Service Management
Kolkata
Dr Utsa Basu Clinic, Kolkata
(25+ Patients)
Ms. Poushali Ghosh
Dietician
9 Years • Msc in Applied Nutrition
Barasat
Diab-Eat-Ease, Barasat
Dr Venkata Naga Sai Tribhushan Rambhatla
General Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult Top Specialists

Dr Haripriya S G
Family Physician
22 Years • MBBS, PGD (Family Medicine)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Ms. Sreeparna Dey Dhara Deb
Dietician
10 Years • DNHE
Bansdroni
Siddhita Healthcare., Bansdroni

Ms. Malabika Datta
Dietician
17 Years • Msc. in Dietetics & Food Service Management
Kolkata
Dr Utsa Basu Clinic, Kolkata
(25+ Patients)
Ms. Poushali Ghosh
Dietician
9 Years • Msc in Applied Nutrition
Barasat
Diab-Eat-Ease, Barasat
Dr Venkata Naga Sai Tribhushan Rambhatla
General Physician
3 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
Can I drink coffee while taking pantoprazole?
Some people can, but coffee (even decaf) may trigger reflux by increasing acidity or relaxing the LES. If you notice symptoms, try limiting coffee, switching to smaller servings, or choosing non-mint herbal tea or water instead.
Is alcohol safe on a pantoprazole diet?
Alcohol is a common trigger that can worsen reflux by irritating the lining and relaxing the LES. Avoiding or minimizing alcohol often helps symptoms. If you choose to drink, keep portions small and avoid drinking close to bedtime.
Do I need to avoid all dairy?
Not necessarily. High-fat dairy (like heavy cream or full-fat cheese) can trigger symptoms for some. Many people do well with low-fat milk or yogurt. Try smaller portions and see what works for you.
When should I take pantoprazole—before or after food?
Pantoprazole generally works best when taken 30–60 minutes before a meal, often before breakfast. Follow your prescriber’s instructions and take it consistently each day.
Does pantoprazole interact with any foods or supplements?
Pantoprazole has no major food interactions. However, some medications and supplements can affect how drugs work. Always check with your clinician or pharmacist before starting new over-the-counter medicines or supplements, especially if you take several prescriptions.