Guide to How Tumour Develop And Grow
Explore a comprehensive guide on tumour development and growth. Learn about the cellular changes, stages, and factors that contribute to how tumours form and progress in the body.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

Introduction
The word "tumour" can understandably cause concern, but understanding what it is and how it develops is the first step toward demystifying the process. At its core, a tumour is a mass of tissue that forms when cells divide and grow in an uncontrolled way. But not all tumours are cancerous. So, how does a single, misbehaving cell transform into a life-threatening condition? This article will guide you through the intricate journey of tumour development, from the first genetic misstep to the complex process of spread. We'll break down the science into easy-to-understand concepts, explain the critical difference between benign and malignant growths, and explore the factors that influence this process. By the end, you'll have a clear picture of the mechanisms behind cancer growth, empowering you with knowledge about prevention and the importance of early detection.
What is a Tumour? Benign vs. Malignant
A tumour, also known as a neoplasm, is essentially a lump or growth. It arises when the body's normal checks and balances on cell growth fail. Normally, cells divide, mature, perform their functions, and eventually die in a tightly regulated process. When this process goes awry, excess cells can accumulate, forming a tumour. The most critical distinction lies in whether this tumour is benign or malignant.
Characteristics of a Benign Tumour
Think of a benign tumour as a well-behaved guest who overstays their welcome. It grows slowly and, most importantly, remains localized. It does not invade nearby tissues or spread to distant parts of the body. Benign tumours are often encapsulated, meaning they are enclosed in a fibrous shell that separates them from surrounding tissue. Common examples include moles, uterine fibroids, and most lipomas (fatty tumours under the skin). While usually not life-threatening, a benign tumour can cause problems if it grows large enough to press on vital organs, nerves, or blood vessels.
Characteristics of a Malignant (Cancerous) Tumour
A malignant tumour is what we call cancer. Its behaviour is far more aggressive. These tumours are characterized by:
• Invasion: Malignant cells can invade and destroy adjacent healthy tissues.
• Metastasis: This is the hallmark of cancer. Cells break away from the primary tumour, travel through the bloodstream or lymphatic system, and form new tumours (metastases) in other organs.
Malignant tumours grow more unpredictably and rapidly than benign ones. Under a microscope, their cells appear abnormal in size, shape, and structure. Understanding this difference between benign and malignant tumour is crucial for diagnosis and treatment.Consult Top Specialists
The Fundamental Process: How a Tumour Starts
The journey of a tumour begins at the most fundamental level: our DNA. Cancer is, in essence, a genetic disease of the cell.
The Role of DNA Mutations
DNA provides the instruction manual for every cell in our body, telling it how to grow, function, and when to die. A mutation is a typo or error in this manual. Mutations happen every day, but our cells have sophisticated repair mechanisms to fix them. However, if a mutation occurs in a gene that controls cell division or DNA repair itself, it can set the stage for cancer. These DNA mutations linked to cancer can be inherited or, more commonly, acquired during a person's lifetime due to environmental factors like tobacco smoke, UV radiation, or simply random errors during cell division.
Oncogenes: The Accelerator Pedal
Certain genes, called proto-oncogenes, normally help cells grow. When a mutation occurs in a proto-oncogene, it can become an oncogene—a permanently "switched-on" gene that acts like a stuck accelerator pedal in a car. It drives the cell to divide relentlessly, ignoring signals to stop.
Tumour Suppressor Genes: The Brakes
Conversely, tumour suppressor genes are the brakes. They slow down cell division, repair DNA mistakes, and tell cells when it's time to die (a process called apoptosis). A mutation that inactivates a tumour suppressor gene is like cutting the brakes. The most famous example is the p53 gene, which is faulty in over half of all human cancers. The process of cancer metastasis often requires the failure of multiple tumour suppressor genes.
The Stages of Tumour Development
The development of a malignant tumour is not a single event but a multi-step process, often called carcinogenesis. This is the central answer to "how do cancer cells form" into a dangerous mass.
Stage 1: Initiation - The First Genetic Hit
This is the initial DNA damage that creates the potential for cancer. An external carcinogen or an internal error causes a mutation in a cell's DNA. This altered cell is now primed for cancer but is not yet cancerous. It may lie dormant for years.
Stage 2: Promotion - Encouraging Growth
During promotion, the initiated cell is stimulated to divide repeatedly. Promoters themselves don't cause cancer but encourage the growth of the already-initiated cells. Factors like chronic inflammation, certain hormones, or a poor diet can act as promoters. This clonal expansion creates a small, benign tumour.
Stage 3: Progression - Becoming Invasive
This is the final and most dangerous phase. The benign tumour acquires additional mutations that赋予 it malignant properties. Cells become invasive, breaking through the basement membrane that normally confines them. They also develop the ability to metastasize. This process of tumour progression involves genetic instability, where the rate of new mutations accelerates, allowing the cancer to evolve and become more aggressive.
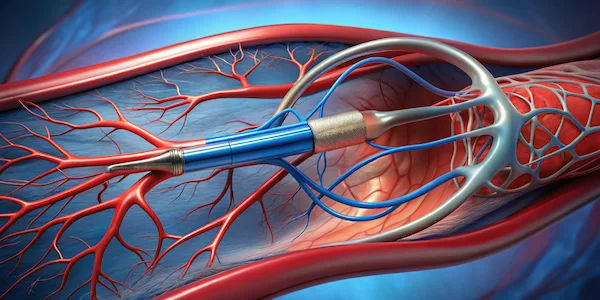
How Tumours Get Their Own Blood Supply: Angiogenesis?
A tiny tumour can only grow to about the size of a sugar cube (1-2 millimeters) without a dedicated blood supply. To grow larger, it needs oxygen and nutrients. This is where angiogenesis comes in. Angiogenesis is the formation of new blood vessels. Normally, this process is tightly controlled (e.g., during wound healing). Cancer cells, however, hijack this process by secreting signals that trick the body into building new blood vessels directly into the tumour. This network provides a lifeline, allowing the tumour to expand rapidly. Understanding how angiogenesis helps a tumour is a key area of cancer research, leading to drugs called angiogenesis inhibitors designed to starve tumours.
How Cancer Spreads?: The Process of Metastasis
Metastasis is what makes cancer so dangerous. It's a complex, inefficient process where cancer cells:
1. Invade: Cells break away from the primary tumour and invade surrounding tissue.
2. Intravasate: They enter the bloodstream or lymphatic system.
3. Survive: Most cells die during transit, but a few survive the immune system's attack.
4. Arrest: The surviving cells lodge in capillaries of a distant organ (like the lungs, liver, bones, or brain).
5. Extravasate: They exit the vessel and invade the new organ.
6. Colonize: The cells multiply to form a new, secondary tumour.
This ability to spread is the ultimate marker of malignancy and is the primary cause of cancer-related deaths.
Common Causes and Risk Factors for Tumour Growth
While the exact cause can be complex, several factors increase the risk of the genetic damage that leads to a tumour:
• Lifestyle Factors: Tobacco use, excessive alcohol consumption, poor diet (high in processed meats, low in fibre), obesity, and physical inactivity.
• Environmental Exposures: UV radiation from the sun, ionizing radiation (e.g., X-rays), certain chemicals (asbestos, benzene), and air pollution.
• Infections: Viruses like HPV (cervical cancer), Hepatitis B and C (liver cancer), and H. pylori bacteria (stomach cancer).
• Genetic Predisposition: Inherited mutations in genes like BRCA1 and BRCA2 significantly increase the risk of breast and ovarian cancers.
• Age: The risk of cancer increases with age because we accumulate more DNA damage over time and our repair mechanisms become less efficient.
Conclusion
Understanding how a tumour develops empowers us to see cancer not as a single monster, but as a complex biological process that unfolds over time. From the initial genetic typo to the aggressive spread of metastasis, each step represents a potential opportunity for intervention—through prevention, early detection, or targeted treatment. While the science is complex, the key message is one of hope and agency. By making informed lifestyle choices, being aware of our bodies, and seeking timely medical advice, we can significantly influence our risk and outcomes. Knowledge is power, and in the fight against cancer, it is one of our most vital assets. If you have concerns about your risk factors, speaking with a healthcare professional is always the best course of action.
Consult Top Specialists
Consult Top Specialists

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
14 Years • MBBS, DNB
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Jyotish R Nair
General Physician/ Internal Medicine Specialist
22 Years • MBBS, MD (General Medicine), PG Diploma(Diabetology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
(150+ Patients)

Dr. Nirmal Mathew Alex
General Physician/ Internal Medicine Specialist
17 Years • MBBS, MD(general medicine)
Angamaly
Apollo Hospitals Karukutty, Angamaly
(50+ Patients)

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
17 Years • MBBS, DNB (Internal Medicine)
Mumbai
Apollo Hospitals CBD Belapur, Mumbai
(250+ Patients)
Consult Top Specialists

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
14 Years • MBBS, DNB
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Jyotish R Nair
General Physician/ Internal Medicine Specialist
22 Years • MBBS, MD (General Medicine), PG Diploma(Diabetology)
Angamaly
Apollo Hospitals Karukutty, Angamaly
(150+ Patients)

Dr. Nirmal Mathew Alex
General Physician/ Internal Medicine Specialist
17 Years • MBBS, MD(general medicine)
Angamaly
Apollo Hospitals Karukutty, Angamaly
(50+ Patients)

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
17 Years • MBBS, DNB (Internal Medicine)
Mumbai
Apollo Hospitals CBD Belapur, Mumbai
(250+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
1. Can a benign tumour become malignant?
Yes, in some cases. While most benign tumours remain harmless, certain types have the potential to transform into cancer over time if they acquire additional mutations. For example, some colon polyps (benign growths) are considered precancerous. This is why doctors often recommend removing them during a colonoscopy.
2. How fast do tumours typically grow?
The growth rate of a tumour varies dramatically depending on the type of cancer and individual factors. Some cancers, like aggressive forms of pancreatic cancer, can grow and spread quickly. Others, like certain prostate cancers or low-grade lymphomas, may be so slow-growing that they may not even require immediate treatment, an approach known as 'active surveillance.'
3. What is the difference between a tumour and a cyst?
A tumour is a solid mass of cells. A cyst is a sac filled with fluid, air, or other material. Most cysts are benign, but a complex cyst may have solid areas and require further investigation to rule out cancer.
4. Are all cancers tumours?
Not all cancers form solid tumours. Cancers of the blood, such as leukaemias, generally do not form solid tumours. Instead, they involve the overproduction of abnormal blood cells that crowd out healthy cells in the bone marrow and blood.
5. Can stress cause a tumour to develop?
While stress does not directly cause cancer by creating DNA mutations, chronic stress can weaken the immune system and may lead to unhealthy behaviours (like smoking or poor diet) that increase cancer risk. The direct link between stress and cancer initiation is complex and not fully proven.