Guide to Category/Head Neck Oncology
Explore the diagnosis, surgical, and non-surgical treatment options for cancers affecting the head and neck region, including the throat, larynx, mouth, sinuses, and salivary glands.

Written by Dr. Siri Nallapu
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
Head and neck cancers can feel overwhelming to understand because they include many different conditions—from mouth and throat cancers to cancers of the larynx, nasal cavity, sinuses, and salivary glands. This guide to category/head neck oncology is designed for the general public looking for clear, trustworthy health advice. You’ll learn what head and neck oncology covers, the common warning signs, how diagnosis and staging work, the latest treatments (including surgery, radiation, chemotherapy, targeted therapies, and immunotherapy), and practical tips for managing side effects and life after treatment. We’ll also touch on prevention, HPV vaccination, tobacco cessation, and how to get help if you’re worried about symptoms. When relevant, we’ll point you to authoritative sources and how to consult a doctor online. Whether you’re concerned about a persistent sore throat or a neck lump, or you’re supporting a loved one, use this comprehensive category/head neck oncology guide to navigate the journey with more confidence.
What Head and Neck Oncology Covers?
- Head and neck oncology focuses on cancers that start in the mouth, tongue, gums, floor of mouth, hard/soft palate, tonsils, throat (oropharynx and hypopharynx), voice box (larynx), nasal cavity and sinuses, nasopharynx, and salivary glands. Most of these are squamous cell carcinomas arising from the mucosal lining, though salivary gland tumors can be adenocarcinomas or other rare histologies. In everyday terms, it’s the category/head neck oncology space dealing with diagnosis, treatment, and recovery across these sites.
- Why this category matters: Head and neck cancers affect core functions—speaking, swallowing, breathing, taste, and appearance—so care is uniquely multidisciplinary. Teams often include ENT/head and neck surgeons, radiation oncologists, medical oncologists, speech and swallowing therapists, dietitians, dentists, and psychosocial support professionals. Globally, head and neck cancers are common in regions with high tobacco, alcohol, or betel nut use. HPV-related oropharyngeal cancers have risen in many countries, while smoking-related laryngeal cancers remain a major burden..
- By the numbers: In the United States, head and neck cancers account for roughly 4% of all cancers; worldwide, lip/oral cavity and pharyngeal cancers rank among the top cancers in many regions. In South and Southeast Asia, oral cavity cancer rates are among the highest globally due to smokeless tobacco and areca nut (betel quid) use. Understanding these patterns helps people assess their own risk and act early.
Unique insight: One under-appreciated strength of category/head neck oncology is the emphasis on function-preserving care. Treatments are increasingly designed not only to control disease but also to maximize quality of life—maintaining speech, swallowing, and appearance whenever possible. Shared decision-making with a multidisciplinary team helps tailor care to your goals.
Consult a Top Head & Neck Surgical Oncologist
Sites and Types of Head and Neck Cancers
- Oral cavity: lips, front two-thirds of tongue, gums, buccal mucosa (inner cheeks), floor of mouth, hard palate.
- Oropharynx: tonsils, base of tongue, soft palate; HPV-related cancers are common here.
- Larynx: voice box; linked closely with tobacco and alcohol.
- Hypopharynx, nasopharynx, nasal cavity, paranasal sinuses, salivary glands.
- Less common: sarcomas, lymphomas of the head/neck region.
How Common Are These Cancers? Global and Local Context
- Rising HPV-associated oropharyngeal cancer incidence in many high-income countries.
- High burden of oral cancers in South Asia due to smokeless tobacco/areca nut.
- Occupational exposures (e.g., wood dust for sinonasal cancers) in specific industries.
Why “Category/Head Neck Oncology” matters for patients?
- Quick navigation to information by site and stage.
- Emphasis on multidisciplinary pathways and supportive care from the start.
- Increasing role of precision pathology (p16/HPV) and targeted/immunotherapies.
Risk Factors, Prevention, and Early Warning Signs
Knowing risk factors helps with prevention and early detection. The top risks are tobacco (smoked and smokeless), heavy alcohol use (especially combined with tobacco), and prior high-risk HPV infection for throat (oropharyngeal) cancers. Betel nut (areca nut) chewing, common in some regions, significantly increases oral cancer risk. Other exposures include prolonged sun exposure (lip cancer), poor oral hygiene, and certain occupational hazards like wood dust (sinonasal cancers).
Early symptoms you shouldn’t ignore:
- A mouth sore, patch (white/red), or ulcer that doesn’t heal in 2–3 weeks
- Persistent sore throat or hoarseness lasting >2 weeks
- Difficulty or pain with swallowing; feeling of a lump in the throat
- Unexplained ear pain (especially if on one side) or persistent nasal blockage/bleeding
- A neck lump persisting for more than two weeks
- Unexplained weight loss, bad breath, or loose teeth without gum disease
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. Early evaluation can be lifesaving.
Prevention strategies that work:
- Stop tobacco in all forms; minimize or stop alcohol.
- Get HPV vaccination as recommended; it prevents most HPV infections that can lead to oropharyngeal cancers.
- Maintain good oral hygiene and regular dental checks; dentists often spot suspicious lesions early.
- Use sun protection for lips and face; use PPE if exposed to dust/chemicals at work.
Unique insight: Prevention is often incremental. A “small wins” approach—switching from daily to weekend drinking, moving smokeless tobacco from mouth to trash, scheduling the HPV vaccine for eligible teens—compounds over time. Most importantly, discuss a personalized risk reduction plan with your clinician.
Tobacco, Alcohol, HPV, and Other Exposures
- Tobacco and alcohol have a synergistic effect, multiplying risk.
- HPV-positive oropharyngeal cancers often present in nonsmokers; they respond differently to treatment.
- Areca nut/betel quid is carcinogenic and commonly overlooked in risk assessments.
Early Symptoms You Shouldn’t Ignore
- The “2-week rule”: persistent symptoms in the mouth/throat/neck merit evaluation.
- Unilateral earache with a normal ear exam can be a referred pain sign of throat cancer.
Prevention Strategies: HPV Vaccination and Lifestyle
- HPV vaccination significantly reduces the risk of HPV-related cancers.
- Regular oral self-checks: look for persistent sores, color changes, or lumps.
How Diagnosis Works: Tests, Staging, and Timelines
Diagnosis in the category/head neck oncology follows a structured path. It typically starts with a thorough history and head-and-neck exam by an ENT specialist, often using a flexible scope to visualize the throat and larynx. Imaging may include contrast-enhanced CT, MRI (for soft tissue detail), PET-CT (to assess spread), and ultrasound for lymph nodes. Definitive diagnosis rests on a biopsy, with pathologists determining cancer type and critical biomarkers such as p16 (a surrogate for HPV in oropharyngeal cancers). Additional tests (e.g., EBV testing in nasopharyngeal cancers) may be ordered.
Staging is based on tumor size/extent (T), lymph node involvement (N), and distant spread (M). For oropharyngeal cancers, staging differs for HPV-positive vs HPV-negative cancers because prognosis and treatment paths diverge. Timely staging guides treatment selection—surgery up-front, radiation, chemoradiation, or systemic therapy first.
Timelines matter. Once a suspicious lesion is found, aim for:
- Specialist evaluation within 1–2 weeks
- Imaging within 2 weeks
- Biopsy and pathology within another 1–2 weeks
- Tumor board discussion before treatment starts, when possible
If logistics are challenging, online consultations can triage urgency. If your condition does not improve after initial measures or if red-flag symptoms persist, book a physical visit to a doctor with Apollo 24|7.
Unique insight: Bring a “diagnosis notebook” or phone note to each visit. Record dates, test names, and key findings. Ask for copies of imaging reports and slide/pathology summaries; these speed up second opinions and treatment planning. Apollo 24|7 also offers convenient home collection for common pre-treatment blood tests like CBC, kidney/liver function, and thyroid function tests that help clinicians plan therapy safely.
Clinical Exam, Imaging, and Biopsy
- Flexible naso-laryngoscopy, mirror exam; intraoral exam.
- Imaging: CT/MRI for extent; PET-CT for staging and radiotherapy planning; ultrasound-guided FNAC for neck nodes.
- Biopsy: incisional/excisional; core needle for nodes; p16/HPV testing for oropharyngeal sites.
Staging Basics and HPV/p16 Testing
TNM staging drives choices; HPV-positive disease is staged differently due to a better prognosis.
p16 positivity suggests HPV-related origin in oropharyngeal tumors.
Getting a Second Opinion and Multidisciplinary Reviews
- Tumor boards integrate surgery, radiation, medical oncology, radiology, and pathology inputs.
- Second opinions can refine plans, especially in borderline cases.
Treatment Pathways: From Surgery to Immunotherapy
Treatment in the category/head neck oncology is tailored to the tumor site, stage, HPV status, and your goals. Early-stage oral cavity cancers often start with surgery; early laryngeal cancers may be treated with radiation or partial laryngeal surgery. Locally advanced disease commonly calls for combined approaches—surgery with adjuvant radiation or chemoradiation; or primary chemoradiation for organ preservation in the larynx/oropharynx.
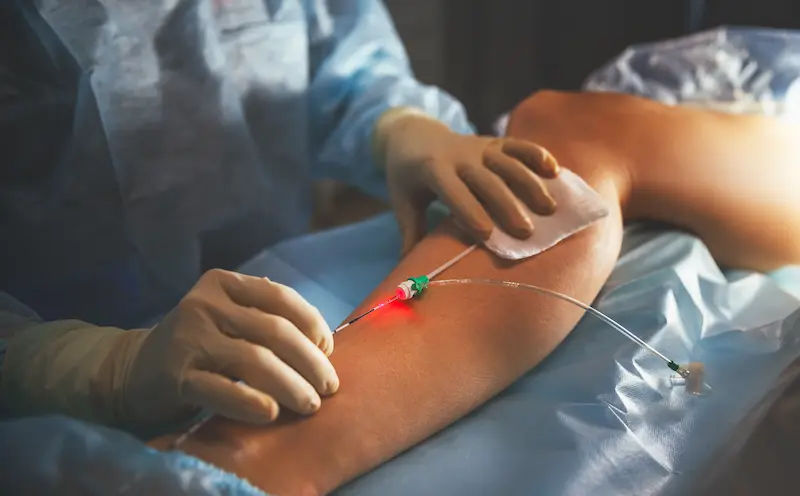
- Surgery and reconstruction: Head and neck surgeons may remove the tumor and reconstruct with local or free flaps to restore form and function. Advances in microvascular reconstruction have improved speech and swallowing outcomes. Transoral robotic surgery (TORS) can remove some oropharyngeal tumors with less morbidity.
- Radiation therapy: Intensity-modulated radiotherapy (IMRT) and image-guided radiotherapy (IGRT) spare normal tissues and reduce side effects like dry mouth. Concurrent chemotherapy (often cisplatin) enhances radiation’s effectiveness in locally advanced disease.
- Systemic therapy: Chemotherapy (cisplatin, carboplatin, 5-FU, taxanes) is used in definitive chemoradiation or for recurrent/metastatic disease. Targeted therapy with cetuximab may be used in select situations. Immunotherapies—pembrolizumab or nivolumab—have become standard options in recurrent/metastatic head and neck squamous cell carcinoma, improving survival in appropriate patients.
- Unique insight: Ask your team whether a “prehab” plan—nutrition optimization, dental care, swallowing exercises—can start before treatment. Starting early can meaningfully reduce complications and hospitalizations. Also discuss whether your case qualifies for any de-escalation strategies (e.g., in HPV-positive disease), ideally within a clinical trial.
Surgery and Reconstruction
- Margin-negative resection is the goal; selective/modified radical neck dissection as indicated.
- Reconstructive flaps (radial forearm, fibula, anterolateral thigh) help restore function.
Radiation Therapy and Chemoradiation
- IMRT reduces dose to salivary glands, swallowing muscles.
- Cisplatin-based chemoradiation remains a backbone for many locally advanced tumors.
Systemic Therapies: Chemotherapy, Targeted, Immunotherapy
- First-line metastatic options may include pembrolizumab alone or with chemotherapy, depending on PD-L1 status; nivolumab in platinum-refractory settings.
- Cetuximab is an EGFR-targeted monoclonal antibody used in select patients.
Personalized Care: Tumor Boards and Shared Decisions
- Outline pros/cons of each path (functional outcomes, time off work, side effect profiles).
- Choose based on values and goals—voice preservation, appearance, or shortest recovery.
Managing Side Effects and Supportive Care
Side effects vary with treatment and site. Common issues include mucositis (painful mouth sores), dry mouth (xerostomia), thick secretions, taste changes, skin irritation, fatigue, swallowing difficulty, weight loss, and dental complications. A proactive plan can make a major difference.
- Nutrition: Work with an oncology dietitian to maintain calories and protein. High-calorie smoothies, soft foods, and small, frequent meals help during radiation. Some patients benefit from a temporary feeding tube to keep treatment on track.
- Speech and swallowing: Early, guided exercises protect muscle function. Speech-language pathologists teach techniques to reduce aspiration and maintain safe swallowing.
- Dental health: See a dentist familiar with oncology before radiation. Address dental issues, receive fluoride trays, and learn jaw-stretching exercises to prevent trismus (jaw tightness).
- Skin and mouth care: Salt-and-baking-soda rinses, oral care protocols, topical analgesics, and saliva substitutes provide relief. Ask about preventive measures for mucositis and candidiasis during chemoradiation.
Unique insight: The “Teeth, Taste, Thyroid” triad. After head/neck radiation, monitor dental health aggressively, recognize that taste changes can alter nutrition, and check thyroid function periodically (radiation to the neck can cause hypothyroidism months or years later). Apollo 24|7 offers convenient home collection for tests like TSH and free T4, as well as CBC and metabolic panels during treatment.
Nutrition, Speech and Swallowing, Dental Health
- A dietitian, SLP, and dentist are essential team members.
- Fluoride trays, jaw physiotherapy, and hydration strategies reduce late effects.
Common Side Effects: Mucositis, Dry Mouth, Skin Changes, Fatigue
- IMRT reduces, but doesn’t eliminate, dry mouth risk.
- Plan rest, light activity, and hydration; ask about salivary-sparing techniques.
Real-world Coping Tips and “Prehab”
- Start swallowing exercises 2–4 weeks before therapy.
- Prep a “radiation pantry” with soft foods, broths, and oral care supplies in advance.
Life After Treatment: Follow-up, Recurrence, and Recovery
After treatment, a survivorship care plan maps follow-up visits, imaging when indicated, dental care, thyroid monitoring, and rehab referrals. Typical follow-up: every 1–3 months in year 1, then less frequently over time, with attention to the original site and neck nodes [3,4]. Lifestyle changes—tobacco cessation, moderate alcohol, nutrition, and exercise—lower the risk of second cancers and support recovery.
- Quality of life: It’s common to experience lingering dry mouth, taste or smell changes, neck stiffness, and voice alterations. Fatigue and “chemo brain” can improve with time, sleep hygiene, nutrition, and gradual exercise. Mental health support and peer groups are invaluable; consider counseling to process changes in body image and function.
- When to seek help: New or persistent pain, sores, swelling, voice changes, difficulty swallowing, unexplained weight loss, or a new neck lump need prompt evaluation. If you notice any concerning symptoms or if recovery stalls, consult a doctor online with Apollo 24|7 for guidance or book a physical visit to a doctor with Apollo 24|7. Early review helps catch recurrences or treatable late effects.
Unique insight: Create a wallet card listing your cancer type, stage, treatments received (including radiation dose and fields), and key late risks (e.g., hypothyroidism). Share it with any new clinician or dentist—it streamlines safe care.
Survivorship Plans and Surveillance Schedules
- Tailored to site/stage; frequent checks early, spacing out over time [3,4].
- Dental and thyroid check-ins are long-term priorities.
Mental Health, Work, and Quality of Life
- Gradual return-to-work plans with accommodations can ease transition.
- Voice/swallowing therapy continues to deliver benefits months to years later.
When to Seek Help and How to Access Care (including Apollo 24|7)?
- Two-week symptom rule remains a helpful guide.
- Use telehealth for triage; book an in-person evaluation for persistent or red-flag symptoms.
- Clinical Trials and What’s Next
- Clinical trials drive progress in category/head neck oncology, including:
- De-escalation trials for HPV-positive disease to maintain outcomes with fewer side effects.
- Novel combinations of immunotherapy, targeted agents, and radiation.
- Biomarker-driven strategies to personalize therapy [3,4].
- Ask your team: What trials are open for my stage and biomarker profile? What are the potential benefits and risks? Reassure yourself that enrollment often includes extra monitoring and support.
Unique insight: Keep a “questions list” for trial discussions—eligibility factors, extra visits, how side effects are handled, and what happens if you withdraw. Even if a trial isn’t right now, you may be eligible later.
How to Find Trials and Questions to Ask?
- Use reputable portals: NCI clinical trials search, Cancer.Net, or institutional trial finders.
- Key questions: goals of the trial, standard-of-care comparisons, out-of-pocket costs.
Emerging Research: De-escalation for HPV-positive disease
Selected, carefully staged HPV-positive cancers may be candidates for reduced-intensity regimens within trials to minimize late effects.
Conclusion
Head and neck cancers are complex, but the path through diagnosis, treatment, and recovery is clearer when you know what to expect. This guide to category/head neck oncology has covered the essentials: how to spot early warning signs, what diagnostic steps typically look like, how treatments are chosen, and the pivotal role of supportive care. Today’s care emphasizes both cure and quality of life—protecting speech, swallowing, and appearance whenever possible. Prevention matters, too: HPV vaccination, tobacco cessation, and regular dental/oral checks can meaningfully lower risk. If you’re dealing with persistent symptoms like a neck lump, a sore that doesn’t heal, hoarseness, or trouble swallowing, don’t wait. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation, and book a physical visit if advised. If you’re already in treatment or recovery, lean on your team—dietitians, speech therapists, and dentists are key allies. Finally, ask about clinical trials; they may offer access to cutting-edge, often gentler approaches. With the right information, a supportive team, and timely care, most people navigate category/head neck oncology with greater confidence and better outcomes.
Consult a Top Head & Neck Surgical Oncologist
Consult a Top Head & Neck Surgical Oncologist

Dr. V R N Vijay Kumar
Surgical Oncologist
9 Years • MBBS, MS (Gen. Surg.), DNB (Surg. Onco.)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad

Dr Monisha P
Head and Neck Surgical Oncologist
8 Years • MBBS, MS ENT, Fellowship in Head and Neck Oncosurgery
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru
(75+ Patients)

Dr. Tapaswini Pradhan
Head and Neck Surgical Oncologist
25 Years • MBBS (MAMC, New Delhi), MS (ENT/ Otorhinolaryngology) (LHMC, New Delhi), DNB (ENT), FELLOWSHIP (Head and Neck) – AIIMS, NEW DELHI,
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Arsheed Hussain Hakeem
Head and Neck Surgical Oncologist
18 Years • MBBS, MS (ENT), DNB (ENT), FHNS
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(50+ Patients)

Dr. Sandip Duarah
Head and Neck Surgical Oncologist
18 Years • MBBS, MS (ENT), MCH Head and Neck oncology
Chennai
Apollo Proton Cancer Center, Chennai
Consult a Top Head & Neck Surgical Oncologist

Dr. V R N Vijay Kumar
Surgical Oncologist
9 Years • MBBS, MS (Gen. Surg.), DNB (Surg. Onco.)
Ahmedabad
Apollo Hospitals Gandhinagar, Ahmedabad

Dr Monisha P
Head and Neck Surgical Oncologist
8 Years • MBBS, MS ENT, Fellowship in Head and Neck Oncosurgery
Bengaluru
Apollo Hospitals Bannerghatta Road, Bengaluru
(75+ Patients)

Dr. Tapaswini Pradhan
Head and Neck Surgical Oncologist
25 Years • MBBS (MAMC, New Delhi), MS (ENT/ Otorhinolaryngology) (LHMC, New Delhi), DNB (ENT), FELLOWSHIP (Head and Neck) – AIIMS, NEW DELHI,
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Arsheed Hussain Hakeem
Head and Neck Surgical Oncologist
18 Years • MBBS, MS (ENT), DNB (ENT), FHNS
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(50+ Patients)

Dr. Sandip Duarah
Head and Neck Surgical Oncologist
18 Years • MBBS, MS (ENT), MCH Head and Neck oncology
Chennai
Apollo Proton Cancer Center, Chennai
More articles from General Medical Consultation
Frequently Asked Questions
What are the early signs of head and neck cancer?
Nonhealing mouth sores, persistent hoarseness, difficulty swallowing, a neck lump, or one-sided ear pain are common signs. Follow the “two-week rule” for early detection of head and neck cancer—get evaluated if symptoms persist.
How is HPV related to throat cancers?
High-risk HPV can cause oropharyngeal (throat) cancers. p16 testing helps identify HPV-related throat cancer, which often has a better prognosis. HPV vaccination reduces future risk.
What side effects should I expect from radiation therapy?
Radiation therapy side effects in head and neck oncology can include mucositis, dry mouth, taste changes, fatigue, and skin irritation. IMRT reduces some risks; supportive care and swallow therapy help.
When is chemotherapy or immunotherapy used?
Chemotherapy helps with locally advanced disease alongside radiation and in metastatic settings. Immunotherapy (pembrolizumab, nivolumab) is used for recurrent/metastatic head and neck squamous cell carcinoma in eligible patients.
How often are follow-up visits after treatment?
Typically every 1–3 months in year 1, spaced out over time, with dental and thyroid checks included. If you notice new symptoms, book a visit right away. If you need quick advice, consult a doctor online with Apollo 24|7.