Guide to Hmpv Outbreak In India
Stay informed about the Human Metapneumovirus (HMPV) in India. Learn about symptoms, high-risk groups, prevention steps, and what to do if you or your child gets infected.

Written by Dr. Siri Nallapu
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
Human metapneumovirus (HMPV) is a common respiratory virus that often flies under the radar compared to flu, RSV, or COVID-19—yet it can cause significant illness, particularly in young children, older adults, and people with chronic conditions. With periodic spikes of respiratory infections reported across Indian cities, many families are asking: Is there an HMPV outbreak in India? What are the symptoms, and how do we protect ourselves? This guide brings together what you need to know—what HMPV is, how it spreads, who is most at risk, how it’s diagnosed and treated, and practical steps for home, school, workplace, and travel. You’ll also learn how HMPV compares to flu, RSV, and COVID-19, and how India’s public health systems track such surges. Throughout, we include trusted references and India-specific tips, along with when to seek care and how to access testing. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. Let’s walk through the facts, cut through myths, and focus on actionable steps you can take today.
Understanding HMPV: The virus and its spread
What is human metapneumovirus?
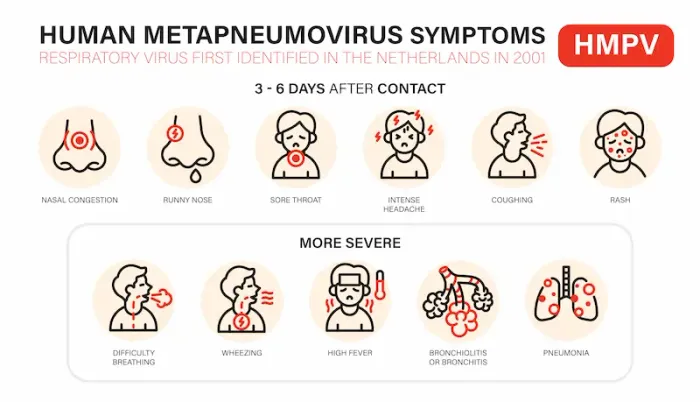
Human metapneumovirus (HMPV) is a respiratory virus identified in 2001. It infects the nose, throat, and lungs, ranging from a common cold like illness to bronchitis or pneumonia . Most children encounter HMPV by the age of five, and reinfections can occur throughout life. There is currently no licensed vaccine for HMPV, and no specific antiviral is routinely recommended; care is typically supportive.
Transmission: droplets, close contact, and surfaces
HMPV spreads primarily through respiratory droplets when an infected person coughs or sneezes, and through close contact (sharing utensils, hugging) or touching surfaces contaminated with secretions and then touching the nose, eyes, or mouth. The incubation period (time from exposure to symptoms) is generally 3–6 days. People are usually most contagious during the first few days of illness but can shed virus for a week or more, particularly young children and those with weakened immunity.Consult a Top General Physician
Seasonality and co-circulation with other viruses
Globally, HMPV tends to circulate in late winter to spring, often overlapping with influenza and RSV seasons. In India, respiratory viruses frequently show peaks in cooler months and sometimes around monsoon transition, with patterns varying by region due to climate, crowding, and school calendars. Co-circulation means a person could be exposed to multiple viruses in the same season—another reason testing is useful when symptoms are significant or persistent.
Unique insight: In India’s joint-family homes and multigenerational caregiving, droplet and contact spread can be amplified unless routine hand hygiene and ventilation are prioritized at home—simple, low-cost steps that are as impactful as public measures in reducing household transmission.
The HMPV situation in India: What we know now
How outbreaks are detected (ILI/SARI surveillance, IDSP, ICMR)
India tracks respiratory illnesses through networks that monitor influenza-like illness (ILI) and severe acute respiratory infection (SARI). The Integrated Disease Surveillance Programme (IDSP) and the Indian Council of Medical Research (ICMR), including National Institute of Virology (NIV) Pune, coordinate specimen testing using RT PCR panels that include influenza viruses, RSV, HMPV, and others . When labs detect a higher-than-expected share of HMPV among respiratory samples, or when clusters occur in schools or hospitals, it can signal a local surge.
Why apparent “spikes” happen after festival seasons and school reopenings?
Crowding during festivals, weddings, and travel—followed by school reopenings—creates a conducive environment for respiratory virus transmission. Seasonal changes (e.g., cooler, drier air in north India winters) also improve viral stability in aerosols and on surfaces. These factors can produce waves of respiratory infections, including HMPV, especially where masking and ventilation are limited.
Where to check reliable updates?
For timely information, check:
• IDSP weekly outbreaks and bulletins.
• ICMR/NIV or state health department advisories.
• Trusted national medical bodies such as the Indian Academy of Pediatrics for child-focused guidance.
• Media reports can be helpful but may mix multiple respiratory viruses; rely on official sources for confirmation.
Unique insight: Consider community-level signals—school absenteeism, a sudden rise in pediatric OPD visits, or clusters in elderly care facilities—as early “thermometers” of local spread even before formal advisories are issued.
Signs and symptoms: What to watch for
Mild illness vs. warning signs
HMPV commonly causes:
• Fever, cough, runny or stuffy nose
• Sore throat, headache, body aches
• Wheezing, especially in children or those with asthma
• Fatigue and poor feeding in infants
Most cases are mild to moderate and improve in 5–10 days. Warning signs include fast or labored breathing, persistent high fever, bluish lips or face, dehydration (very little urine), confusion, chest pain, or worsened wheezing. These require urgent medical evaluation.
How symptoms differ by age and risk group?
• Infants and toddlers: May present with bronchiolitis (wheezing, rapid breathing), feeding difficulty, or irritability. Reinfections occur but are often milder .
• Older adults (65+): Can develop lower respiratory tract infections, with fatigue and breathlessness more prominent; symptoms can mimic bacterial pneumonia.
• People with chronic lung disease (asthma, COPD), heart disease, diabetes, or immunocompromise: Higher risk of complications and hospitalization .
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. If you notice red-flag signs at any point, book a physical visit to a doctor with Apollo 24|7 or go to the nearest emergency facility.
Who is most at risk in India?
Young children, older adults, and those with chronic disease
Children under five (especially under two), older adults, and people with chronic lung or heart disease are more likely to experience severe HMPV disease, including bronchiolitis and pneumonia. Hospitalization risk increases in those with compromised immunity.
Pregnancy, air pollution, and household crowding
• Pregnancy: Viral respiratory infections in pregnancy may increase risks for the mother (e.g., hypoxia) and the fetus; prompt care for persistent symptoms is advised.
• Air pollution: High PM2.5/PM10 levels, common in many Indian cities, can worsen respiratory symptoms and inflame airways, increasing susceptibility and severity of viral infections.
• Household crowding and multigenerational living: Close contact with symptomatic family members makes targeted prevention (masking for the ill person, separate utensils/towels, frequent handwashing) especially valuable.
Testing and diagnosis: RT PCR and panels
When to test for HMPV?
Testing is not required for every mild cold. Consider testing when:
• Symptoms are moderate to severe (e.g., high fever, persistent cough, wheezing)
• The patient is very young, elderly, pregnant, immunocompromised, or has chronic disease
• There is a local respiratory outbreak or hospital cluster
• A diagnosis will change management (e.g., hospital admission, isolation decisions)
Types of samples and how RT PCR works
RT PCR detects HMPV genetic material from nasal or throat swabs and is the standard diagnostic method . Respiratory panels may test for multiple viruses (influenza A/B, RSV, SARS CoV 2, HMPV, adenovirus, parainfluenza). Turnaround is typically within 24–48 hours in most urban centers.
Access and home collection options
Many accredited labs in India offer multiplex RT PCR respiratory panels. For convenience and to reduce exposure, consider home collection services: Apollo 24|7 offers convenient home collection for tests like comprehensive respiratory RT PCR panels. Ask whether HMPV is included specifically when booking.
Treatment and home care: What actually helps
Supportive care and over-the-counter options
There is no specific antiviral routinely recommended for HMPV; treatment is supportive :
• Rest, fluids, and nutrition as tolerated
• Paracetamol or ibuprofen for fever and aches (avoid aspirin in children)
• Saline nasal drops/sprays and steam inhalation for congestion
• Inhaled bronchodilators if prescribed for wheezing/asthma
Antibiotics do not treat viruses; they are used only if a bacterial complication is suspected.
Red flags that need urgent care
Seek immediate care for:
• Fast or difficult breathing, chest indrawing, bluish lips/face
• Persistent high fever (>38.5°C) beyond 3–4 days
• Lethargy, confusion, seizures
• Signs of dehydration (very little urine, sunken eyes, no tears)
• Worsening symptoms in infants, older adults, or those with chronic disease
If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
Recovery timeline and preventing spread at home
Most people recover in 5–10 days; cough can linger 1–2 weeks. To reduce spread at home:
• Mask the symptomatic person for the first 5–7 days
• Keep windows open for cross-ventilation
• Isolate utensils, towels, and commonly touched items
• Wash hands before meals and after coughing/sneezing
Prevention during an outbreak: Masks, ventilation, hygiene
Masking: where and when it matters most
• Use a well-fitted mask (surgical or KN95/N95 if available) in crowded indoor spaces, especially during active surges or if you’re symptomatic.
• In India’s busy public settings—metros, buses, hospital OPDs, markets—masking significantly reduces droplet spread.
• Teach children the mask “fit and feel” with short practice at home; even 60–70% compliance in schools reduces overall transmission.
Indoor air: cross-ventilation, fans, and filters
• Cross-ventilation (two opposite windows open) dilutes indoor virus particles.
• Use ceiling and exhaust fans to keep air moving; avoid stagnant air in closed rooms.
• Portable HEPA purifiers help in bedrooms of high-risk persons; in resource-limited settings, keep doors/windows ajar and avoid indoor crowding.
Hand hygiene and surface cleaning
• Wash your hands for 20 seconds with soap and water or use alcohol-based sanitizer.
• Clean high-touch surfaces (doorknobs, phone screens, remotes) daily when someone is ill.
• Encourage cough etiquette: into a tissue or elbow, followed by hand hygiene.
HMPV vs flu, RSV, and COVID 19: Spot the differences
Symptoms overlap—and how testing clarifies
HMPV, influenza, RSV, and COVID 19 share fever, cough, and congestion. Distinguishing features are unreliable clinically; for example, loss of taste/smell suggests COVID 19, but it isn’t universal, and wheezing can occur with HMPV or RSV. Testing clarifies the cause, especially in high risk patients or during outbreaks.
Reinfection patterns and immunity
• HMPV: Reinfection is common; immunity is incomplete and wanes over time.
• RSV: Reinfections occur; severe disease often in infants and older adults.
• Influenza: Annual antigenic drift; updated vaccines reduce severity.
• COVID 19: Reinfections occur; vaccines reduce severe outcomes.
Currently, no licensed HMPV vaccine exists, though candidates are in development.
Schools, workplaces, and public transport: Practical guidance
Return-to-school criteria and classroom ventilation
• Keep children home if they have fever, heavy cough, or breathing difficulty.
• Return when fever-free for 24 hours without medication and symptoms are improving.
• Encourage cross-ventilation in classrooms, outdoor assemblies, and staggered snack breaks to reduce indoor crowding.
Office policies and sick leave
• Promote a “stay-home-when-sick” policy; remote work where feasible during peaks.
• Improve ventilation in meeting rooms; schedule shorter, smaller in-person meetings.
• Provide hand sanitizer and encourage masking during surges.
Buses, metros, and ride-shares
• Wear masks in crowded transport; open windows where possible.
• Off-peak travel reduces exposure.
• For ride-shares, sit in the rear seat, keep a window slightly open, and avoid conversation if symptomatic.
Public health surveillance and response in India
IDSP, ICMR, NIV Pune: who does what
• IDSP (Integrated Disease Surveillance Programme) compiles nationwide data on outbreaks, including respiratory illnesses.
• ICMR coordinates research and surveillance; NIV Pune is a reference lab for respiratory virus diagnostics and characterization.
How data informs advisories?
• When ILI/SARI surveillance detects increased positivity for a virus like HMPV, advisories may recommend strengthened masking/hygiene, hospital preparedness, and public messaging. These systems also help distinguish HMPV from influenza or COVID 19 surges.
What communities can do to help?
• Cooperate with contact tracing and outbreak investigations.
• Encourage early care-seeking for high-risk individuals.
• Share accurate information from official channels; counter myths within WhatsApp groups and resident welfare associations.
Unique insight: Local data transparency—notice boards at schools or RWAs showing weekly absenteeism and a “respiratory season barometer”—can build trust and improve timely preventive action.
If symptoms persist beyond two weeks or you’re in a high risk group, consult a doctor online with Apollo 24|7 for further evaluation.
Conclusion
HMPV may be less famous than flu, RSV, or COVID 19, but it is a steady contributor to respiratory illness in India—especially in cooler months and during times of increased social mixing. The good news: the basics work. If there’s an HMPV outbreak in your city or school, lean on the same proven measures—mask in crowded indoor spaces, keep indoor air fresh, wash hands often, and stay home when sick. For most people, HMPV is manageable at home with rest, fluids, and fever control, though infants, older adults, pregnant women, and those with chronic health issues deserve closer attention. Testing with an RT PCR respiratory panel can clarify what’s causing symptoms and guide household precautions. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7; if you notice red flags like fast breathing or confusion, seek urgent in person care right away. By staying informed through IDSP/ICMR updates, looking out for one another, and taking commonsense steps at home, school, and work, we can navigate HMPV seasons with confidence and protect the most vulnerable among us.Consult a Top General Physician
Consult a Top General Physician

Dr. S Vijayaraghavan
General Physician/ Internal Medicine Specialist
31 Years • MD (Gen. Med.)
Chennai
Apollo Speciality Hospitals OMR, Chennai
(175+ Patients)

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Divya Lekha Gunta
General Practitioner
10 Years • MBBS, MD (Pathology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam
Consult a Top General Physician

Dr. S Vijayaraghavan
General Physician/ Internal Medicine Specialist
31 Years • MD (Gen. Med.)
Chennai
Apollo Speciality Hospitals OMR, Chennai
(175+ Patients)

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Divya Lekha Gunta
General Practitioner
10 Years • MBBS, MD (Pathology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam
More articles from General Medical Consultation
Frequently Asked Questions
1) Is HMPV dangerous for babies?
HMPV can cause bronchiolitis and pneumonia in infants, especially under two years. Watch for fast breathing, poor feeding, or dehydration. If any red flags appear, seek urgent care. Keywords: is hmpv dangerous for babies; human metapneumovirus symptoms in children.
2) How long does HMPV last in kids and adults?
Most recover in 5–10 days; coughs may linger 1–2 weeks. High risk groups may have longer courses or complications. Keywords: how long does hmpv last in kids; hmpv treatment at home for adults.
3) When should I get an HMPV RT PCR test in India?
Test if symptoms are moderate/severe, you’re high risk, there’s a local surge, or the result will change care. Consider a home collection. Keywords: hmpv RT PCR test home collection; hmpv infection India update.
4) How is HMPV different from flu, RSV, and COVID 19?
Symptoms overlap widely; testing distinguishes them. No vaccine exists for HMPV yet; flu and COVID 19 vaccines reduce severe disease. Keywords: hmpv vs rsv vs flu differences; hmpv vs covid cough and fever.
5) What are the best prevention steps during an HMPV outbreak in Indian cities?
Mask in crowded indoor spaces, ventilate rooms, practice hand hygiene, and stay home when sick. Schools and offices should improve air flow and support sick leave. Keywords: hmpv outbreak in Indian cities; hmpv transmission and prevention.