How To Increase Your Chances Of Normal Delivery?
Discover practical tips and expert guidelines to improve your chances of a normal vaginal delivery, including exercise, nutrition, and prenatal care strategies.


Introduction
If you’re hoping for a normal delivery, you’re not alone. A vaginal birth can offer shorter recovery, lower complication risks, and a quicker return to daily life for many parents and babies. While no one can guarantee how labour unfolds, you can absolutely improve your chances of normal delivery with the right preparation, support, and evidence-based choices. In this guide, we’ll demystify what truly influences your chances, from prenatal habits and fitness to the labour-room strategies that matter most. You’ll discover how to choose a supportive provider, create a flexible birth plan, use positions and natural comfort measures, and make smart decisions about induction, monitoring, and pain relief. We’ll also cover special scenarios—like VBAC and breech—and how to pivot safely if plans change. Throughout, you’ll see where high-quality research (WHO, ACOG, NICE, and Cochrane) supports specific steps you can take. Whether this is your first birth or not, this practical, science-informed playbook can help you feel prepared, confident, and ready to improve your chances of a normal, positive delivery experience.
What Is a “Normal Delivery” and Why Aim for It?
A normal delivery means a vaginal birth without major surgical intervention. It may still include medical support—like labour augmentation, pain relief, or assisted delivery (vacuum/forceps)—if needed for safety. Vaginal birth is associated with benefits such as shorter hospital stays, lower infection risk, less postoperative pain, and faster return to mobility for many people. Babies may benefit from lower respiratory complications and exposure to maternal microbiota. That said, a cesarean is the safest option in specific situations—like placenta previa, certain fetal positions/distress, or complications such as severe preeclampsia. The goal isn’t “vaginal birth at all costs,” but a safe, healthy birth with shared decision-making.
A realistic mindset helps. Labour is unpredictable; what you can control is your preparation and your team. Evidence emphasises woman-centered care, continuous support, mobility, and avoiding unnecessary interventions as ways to improve chances of a normal delivery while preserving safety. Keeping the focus on progress and wellbeing, rather than rigid expectations, reduces stress—which itself can help labor progress more smoothly. Consider your preferences as “strong wishes” rather than absolutes so your plan can adapt to real-time needs.
Factors That Affect Your Chances
Your chances of normal delivery reflect a mix of modifiable and non-modifiable elements:
• Non-modifiable: First-time birth (nulliparity), age (older maternal age may increase certain risks), pelvic shape and fetal size, and certain medical conditions. These inform planning and monitoring.
• Modifiable: Pre-pregnancy and pregnancy BMI, fitness level, stress/fear, timing of hospital admission, provider and hospital practices (e.g., cesarean rates, protocols for induction and monitoring), and presence of continuous labour support.
Provider and hospital practices are powerful. Facilities with lower cesarean rates and policies supporting mobility, intermittent monitoring when appropriate, and non-pharmacologic comfort often see higher vaginal birth rates. Ask about your provider’s cesarean rate for low-risk first-time births and the hospital’s policies (such as freedom to move in labour, access to tubs/showers, and doula-friendly practices).
Understanding your own risk profile helps you and your clinician build a plan: if you have gestational diabetes, hypertension, or anaemia, proactive management can increase your chances of normal delivery. For example, treating anaemia can improve stamina and reduce the likelihood of interventions. As you track your progress, remember that many factors can be optimised by choices you make before and during labour.
Consult Top Specialists
Prenatal Habits That Improve Your Odds
Regular antenatal care ensures early detection and management of issues that can affect labour. Screenings for anaemia, gestational diabetes, and blood pressure allow timely action. If needed, Apollo 24|7 offers convenient home collection for tests like haemoglobin, fasting glucose, or HbA1c—useful for monitoring anaemia and glucose control during pregnancy.
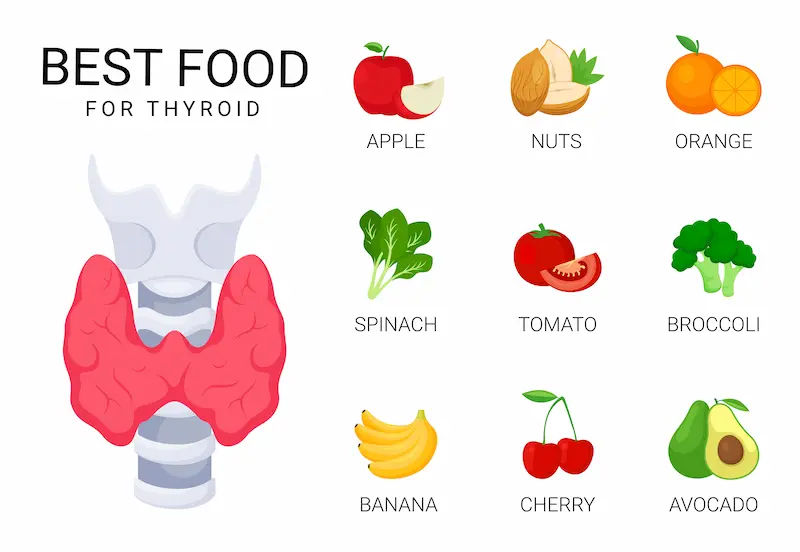
Healthy weight gain supports labour progress. Follow guidance tailored to your pre-pregnancy BMI; gaining too much or too little can raise risks. Focus on a nutrient-dense diet: iron-rich foods (lentils, leafy greens, lean meats) for anaemia prevention; calcium and vitamin D for bone and muscle function; and adequate protein to support tissue health. Hydration matters, too—dehydration can exacerbate contractions and fatigue.
Lifestyle habits that boost your chances of normal delivery include:
• Routine moderate exercise (see next section) and daily walking.
• Sleep hygiene: 7–9 hours with side-lying positions to optimise blood flow and reduce back strain.
• Smoking cessation and limiting alcohol, both of which impact fetal growth and placental health.
• Stress reduction: mindfulness, prenatal yoga, or brief daily breathing practices help lower anxiety and may improve pain coping in labour.
If you develop symptoms like persistent headaches, visual changes, severe swelling, decreased fetal movement, or bleeding, contact your doctor promptly. If symptoms persist beyond two weeks or you’re uncertain about warning signs, consult a doctor online with Apollo 24|7 for further evaluation. Early management of complications can be the difference between a smooth vaginal birth and an unplanned cesarean.
Physical Preparation: Fitness, Pelvic Floor, and Perineal Care
Exercise is one of the best evidence-based ways to prepare for a normal delivery. ACOG recommends most pregnant people engage in at least 150 minutes per week of moderate-intensity aerobic activity, spread over several days. Brisk walking, stationary cycling, swimming, and low-impact aerobics can build endurance for labour’s “marathon.” Light strength training supports posture, pelvic stability, and stamina. Always tailor intensity to your current fitness and talk to your clinician if you have complications.
Pelvic floor muscle training (PFMT) helps you learn to contract—and crucially, to relax—muscles you’ll use in second stage. While research most strongly shows PFMT prevents urinary incontinence, many clinicians observe it helps with pushing efficiency and body awareness. Aim for daily sets (quick squeezes plus longer holds) and include “release” practice so you don’t over-tighten. Consider a short session with a pelvic floor physiotherapist for personalised guidance.
Perineal massage from 34–35 weeks can increase perineal elasticity and reduce severe tearing and episiotomy, especially in first-time births, according to guidance from professional bodies like RCOG. Use clean hands and a natural oil, apply gentle downward and side pressure at the vaginal opening for a few minutes, 3–4 times per week. If you have infections, bleeding, or discomfort, ask your clinician before starting. Long-tail terms to integrate: perineal massage for vaginal birth; pelvic floor training in pregnancy.
Mindset and Support: Classes, Doulas, and Your Birth Plan
Confidence is a labour tool. Quality childbirth classes give you a toolkit: how labour progresses, when to go to the hospital, breathing and visualisation, positions, and how to navigate interventions. Learning pain-coping techniques reduces fear, which can slow progress. Practice a few techniques regularly so they’re second nature on the day.
Continuous labour support—a trained doula, experienced birth partner, or dedicated midwife—has some of the best evidence for improving chances of normal delivery. A Cochrane review shows continuous support reduces the likelihood of cesarean, lowers need for pain medication, and increases satisfaction. Partners can prepare by learning counter-pressure, massage, and phrases that cue effective breathing. A doula can coordinate these comfort measures and help you advocate respectfully.
Create a flexible birth plan. Highlight preferences such as:
• Mobility and upright positions during labour.
• Intermittent monitoring when appropriate.
• Access to water (tub/shower), birth ball, and dim lighting.
• Stepwise pain relief: starting with non-pharmacologic options, then nitrous or epidural if desired.
• Avoiding routine amniotomy or episiotomy unless needed.
Use the BRAIN acronym for decisions in labor: Benefits, Risks, Alternatives, Intuition, and Next/Not now. Long-tail terms: natural pain relief during labor; low-intervention birth plan.
Consult Top Specialists
Approaching Labor: Induction, Onset, and Early Labor Strategies
Spontaneous labour is associated with higher rates of vaginal birth in many settings. However, induction is appropriate for medical reasons (e.g., prolonged pregnancy, preeclampsia, concerns for baby). Evidence from a large U.S. trial suggests elective induction at 39 weeks in low-risk first-time mothers, within supportive settings, did not increase and may reduce cesarean risk compared with expectant management. This highlights that context and practice style matter: if induction is needed, a patient-centred, stepwise approach can still support a normal delivery.
The Bishop score (cervical dilation, effacement, consistency, position, and fetal station) predicts induction success. If your cervix is “unripe,” cervical ripening with a balloon catheter or prostaglandins may improve your chances of vaginal birth compared with starting strong contractions on a firm, closed cervix. Ask about your Bishop score and ripening options.
In early labour, rest and hydration are underrated. Many first-time parents do best labouring at home through early labour, arriving at the hospital once contractions are longer, stronger, and closer (often the “5-1-1” cue: every 5 minutes, lasting 1 minute, for at least 1 hour—if your clinician agrees). Early admission can increase the cascade of interventions for some. At home, use:
• Light meals and plenty of fluids or electrolytes.
• Position changes every 20–30 minutes.
• Warm shower or bath for comfort (if membranes intact).
• A calm environment: low lights, low noise, familiar music.
Long-tail terms: early labour at home guidelines; induction vs spontaneous labour outcomes.
In-Labour Tactics: Positions, Comfort, Monitoring, and Pain Relief
Mobility and upright positions in labour are linked to shorter labours and less need for epidurals or operative births in some studies. Use gravity: slow dancing holds, lunges with a chair, side-lying with a peanut ball, hands-and-knees to relieve back labour, and supported squats for brief periods. Rotate positions every 20–30 minutes unless something clearly works.
Comfort measures with solid evidence include:
• Continuous support (doula/partner).
• Water immersion in active labour which reduces epidural use and may improve birth experience.
• Heat packs on the lower back or lower abdomen.
• TENS units for early/active labour back pain.
• Focused breathing: lengthen exhalation; pair exhales with a mantra.
• Counter-pressure/hypnobirthing techniques.
Monitoring: For low-risk labours, intermittent auscultation is often appropriate and supports mobility. If continuous electronic fetal monitoring is needed, ask for wireless telemetry and wireless IV pumps so you can keep moving. When labour slows, consider non-invasive steps first: bladder emptying, hydration, position changes, nipple stimulation.
Pain relief: Epidurals are safe and effective for many; they may limit mobility but increasingly can be dosed lightly to preserve some movement. Nitrous oxide offers flexible, short-acting relief. IV opioids may help early on but can cause drowsiness. Discuss with your provider how to pair pain relief with strategies that preserve your chances of normal delivery (e.g., peanut ball, side-lying “flying cowgirl” positions). Long-tail terms: upright positions for labour; natural pain relief during labour.
Special Scenarios and When Plans Change
VBAC (vaginal birth after cesarean): Many people are candidates for VBAC, and success rates can exceed 60–70% depending on history and setting. A supportive facility with immediate surgical capability and a provider comfortable with VBAC improves safety and chances. Discuss your individual factors (reason for prior cesarean, inter-pregnancy interval, cervical status).
Breech: If your baby is breech at 36–37 weeks, ask about external cephalic version (ECV)—a procedure to gently turn the baby head-down. ECV increases chances of vaginal birth in eligible patients. Techniques like spending time on hands-and-knees or using a forward-leaning inversion may offer comfort but have limited evidence for turning babies.
Big baby (suspected macrosomia) and twins: Ultrasound estimates of fetal weight can be off by 10% or more. Many people still birth larger babies vaginally; choices around induction or cesarean should consider your pelvis, baby’s position, and progress in labor.
When a cesarean is needed: Sometimes the safest path is surgery. Consider a “gentle cesarean” approach—clear drapes, delayed cord clamping when possible, and immediate skin-to-skin—so you retain aspects of your birth preferences. Remember: the goal is a healthy parent and baby. Long-tail terms: VBAC chances and safety; how to avoid unnecessary c-section.
Red Flags and When to Call a Doctor
Before labour, seek care urgently if you have vaginal bleeding, severe abdominal pain, persistent headache with visual changes, sudden swelling, fever, or decreased fetal movements. During labour, call or go in if contractions are regular and intensifying (per your provider’s guidance), your water breaks with meconium-stained fluid (green/brown), you have relentless pain between contractions, or you feel something is wrong. If your condition does not improve after trying home comfort methods or you’re unsure about symptoms, book a physical visit to a doctor with Apollo 24|7. Quick access to guidance can prevent complications and keep your path toward normal delivery on track.
Postpartum Recovery and Pelvic Floor After Vaginal Birth
Vaginal birth usually allows quicker recovery, but your body still needs rest, nutrition, and pelvic floor care. In the first days, focus on:
• Ice packs or sitz baths for perineal soreness.
• Scheduled pain relief as advised.
• Gentle pelvic floor “reconnect” breaths (inhale to release; exhale to lightly engage).
• Regular hydration and fibre to prevent constipation.
Watch for warning signs: fever, severe perineal pain, heavy bleeding, foul-smelling discharge, or calf pain. Early follow-up, especially if you had a significant tear, supports long-term function. Around 4–6 weeks, consider a pelvic floor physiotherapy check to tailor exercises and address any incontinence or discomfort with intercourse. Investing in recovery protects your wellbeing in future pregnancies and may improve your chances of normal delivery next time, too.
Consult Top Specialists
Conclusion
Aiming for a normal delivery is a worthy goal—and one that’s often within reach when you prepare your body, mind, and care team. Start with strong prenatal habits: regular checkups, targeted exercise, pelvic floor and perineal care, and a nutrient-dense diet. Build a birth plan that favours mobility, continuous support, and stepwise interventions, and choose a provider and hospital whose practices align with a low-intervention, safety-first approach. When labour begins, conserve energy early, use gravity and movement as powerful allies, and lean on comfort techniques—water, heat, counter-pressure, and focused breathing. Know that pain relief and necessary medical steps can be integrated thoughtfully without derailing your chances of normal delivery. If special scenarios arise—VBAC, suspected big baby, or induction—evidence-based discussions help you chart the safest path while preserving your preferences where possible. And if plans change to cesarean, a gentle, personalised approach can still deliver a positive birth experience.
Your body is designed to do this, and your preparation can tilt the odds in your favour. If questions or symptoms arise at any point, consult a doctor online with Apollo 24|7 for timely guidance. For lab monitoring, Apollo 24|7 offers home collection to keep your prenatal care consistent and convenient. Here’s to a safe, confident journey toward the birth you envision.
Consult Top Specialists

Dr Bhawna Garg
Gynaecological Oncologist
26 Years • MBBS, MS, (PGI MS ROHTAK) FELLOWSHIP GYNECOLOGY ONCOLOGY, (CANCER INSTITUTE CHENNAI)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Shruti I
Obstetrician and Gynaecologist
7 Years • MBBS, MS (OBSTETRICS & GYNAECOLOGY)
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Harshitha B R
Obstetrician and Gynaecologist
11 Years • MBBS, DGO( OBS & GYN)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Somdutta Basu
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Bansdroni
Siddhita Healthcare., Bansdroni
Consult Top Specialists

Dr Bhawna Garg
Gynaecological Oncologist
26 Years • MBBS, MS, (PGI MS ROHTAK) FELLOWSHIP GYNECOLOGY ONCOLOGY, (CANCER INSTITUTE CHENNAI)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Shruti I
Obstetrician and Gynaecologist
7 Years • MBBS, MS (OBSTETRICS & GYNAECOLOGY)
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Harshitha B R
Obstetrician and Gynaecologist
11 Years • MBBS, DGO( OBS & GYN)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Somdutta Basu
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Bansdroni
Siddhita Healthcare., Bansdroni
Consult Top Specialists

Dr Bhawna Garg
Gynaecological Oncologist
26 Years • MBBS, MS, (PGI MS ROHTAK) FELLOWSHIP GYNECOLOGY ONCOLOGY, (CANCER INSTITUTE CHENNAI)
Delhi
Apollo Hospitals Indraprastha, Delhi

Dr. Shruti I
Obstetrician and Gynaecologist
7 Years • MBBS, MS (OBSTETRICS & GYNAECOLOGY)
Bangalore
Apollo Clinic Bellandur, Bangalore

Dr. Mona Yadav
Obstetrician and Gynaecologist
19 Years • MBBS, MD (Obstetrics & Gynaecology)
Dombivli
Nulife multispeciality, Dombivli

Dr. Harshitha B R
Obstetrician and Gynaecologist
11 Years • MBBS, DGO( OBS & GYN)
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Somdutta Basu
Obstetrician and Gynaecologist
7 Years • MBBS, MS Obstetrics & Gynaecology
Bansdroni
Siddhita Healthcare., Bansdroni
More articles from General Medical Consultation
Frequently Asked Questions
1) What are the best exercises to increase my chances of normal delivery?
Moderate aerobic activity (walking, swimming, stationary cycling) 150 minutes per week, with light strength training and daily pelvic floor practice. Always clear your plan with your clinician. Related term: exercises for normal delivery in third trimester.
2) Does perineal massage really help with vaginal birth?
Evidence suggests perineal massage from 34–35 weeks can reduce severe tearing and episiotomy, especially in first-time births. Ask your clinician about technique and timing. Related term: perineal massage for vaginal birth.
3) Can I still have a normal delivery if I’m induced?
Yes. Success depends on your cervical readiness (Bishop score), the reason for induction, and a stepwise, supportive approach. In some settings, low-risk induction at 39 weeks did not increase and may reduce cesarean risk. Related term: induction vs spontaneous labour outcomes.
4) Will getting an epidural reduce my chances of normal delivery?
An epidural can limit mobility, but with position aids (peanut ball, side-lying) and patient-centred care, many people still have a normal delivery. Discuss dosing options that preserve some movement. Related term: natural pain relief during labour.
5) How can I improve VBAC chances and safety?
Choose a VBAC-supportive provider and hospital, review your prior cesarean details, manage weight and health conditions, and aim for spontaneous labour when possible. Many candidates have a 60–70% chance of VBAC in supportive settings. Related term: VBAC chances and safety.