Guide to Human Metapneumovirus Hmpv
Learn about Human Metapneumovirus (HMPV): symptoms, transmission, diagnosis, treatment, and prevention. Get essential facts on this common respiratory infection affecting all ages.


Introduction
If you or your family have been down with a “stubborn cold” that turned into a deep cough or wheeze, you may have met human metapneumovirus—better known as HMPV. This common respiratory virus travels much like the flu or RSV, and it can hit hardest in infants, older adults, and anyone with fragile lungs or immunity. The good news: most people get better with rest, fluids, and simple home care. The not-so-good news: there’s no specific antiviral or vaccine—yet.
In this guide, we break down human metapneumovirus in clear, practical terms. You’ll learn what HMPV is, how it spreads, the symptoms to watch for, who’s at risk, and when to consider testing. We’ll cover treatment and recovery tips, prevention that actually works, and what the latest research says about vaccines and new therapies. Whether you’re caring for a child, supporting an older family member, or just want to stay informed, this article will help you feel prepared for HMPV season and beyond.
What Is Human Metapneumovirus (HMPV)?
A quick definition in plain language
Human metapneumovirus (HMPV) is a common respiratory virus that causes colds, bronchitis, bronchiolitis, and
pneumonia. It’s in the same virus family as respiratory syncytial virus (RSV) and tends to circulate in late winter and spring in many regions Apollo 24|7. Most infections are mild and resolve at home, but HMPV can lead to serious illness in infants, older adults, and people with chronic conditions.
Discovery, virology, and how it compares to RSV?
HMPV was first identified in the early 2000s in the Netherlands when scientists examining children with respiratory
illness found a previously unrecognized paramyxovirus. Like RSV, HMPV infects the upper and lower airways,
triggering inflammation that can narrow small airways in young children and people with asthma or COPD.
Reinfections can occur throughout life because immunity wanes, and the virus has different subgroups that evolve over
time. Compared with RSV, HMPV often presents similarly but may be slightly more common in older children, and it
can cause wheezing and pneumonia across age groups.
How does HMPV spread: droplets, close contact, and surfaces?
HMPV spreads through respiratory droplets when someone coughs, sneezes, talks, or sings; by touching contaminated
surfaces and then your face; and through close contact like caring for a sick child. Incubation is typically 3–6 days.
People are usually contagious for several days, and younger children may shed the virus longer. The same everyday actions that help prevent colds and flu—hand hygiene, masking when sick, good ventilation—also reduce the risk of HMPV.
Consult a Top General Physician
Symptoms: What HMPV Looks Like in Real Life?
Typical timeline and incubation period
After exposure, symptoms often begin within 3–6 days and start like a common cold: runny or stuffy nose, sore throat,
cough, and low-grade fever. In many people, symptoms peak around days 3–5 and then gradually improve over 1–2
weeks. A dry cough can linger as a “post-viral cough” for a few weeks while the airway lining heals—especially in
people with asthma or smokers.
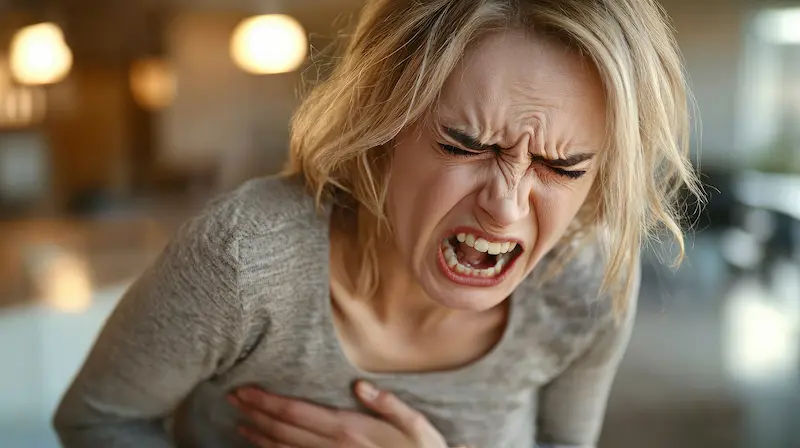
Mild vs. severe illness
- Mild illness: Runny nose, sore throat, cough, fatigue, low fever. Most adults and older children fall into this category
and recover with rest and fluids. - Moderate illness: Fever, persistent coughing fits, chest discomfort, shortness of breath on exertion, wheezing.
- Severe illness: Fast or labored breathing, hypoxia (low oxygen), signs of dehydration, blue lips, or confusion—more
likely in infants, older adults, and those with lung/heart disease or weakened immunity. Severe cases may require oxygen, inhaled medications, or hospitalization.
Children vs. adults: how symptoms differ
In infants and toddlers, HMPV is a common cause of bronchiolitis—swollen small airways that cause noisy breathing,
wheezing, and feeding difficulties Apollo 24|7. In older children, prolonged cough and wheeze are common. Adults often describe a “heavy chest cold” with fatigue and a nagging cough; older adults can develop pneumonia, sometimes without high fever, presenting instead with weakness or confusion. If symptoms persist beyond two weeks or worsen after initial improvement, consult a doctor online with Apollo 24|7 for further evaluation.
Red-flag symptoms you shouldn’t ignore
Seek urgent care if you notice: breathing fast or struggling to breathe; chest pain; bluish lips; oxygen saturation below
92% at rest; dehydration (very few wet diapers or dark urine); confusion; or persistent high fever (>39°C) beyond three
days.
How HMPV Spreads and Who Is at Risk?
High-risk groups (infants, older adults, chronic disease, immunocompromised)
- HMPV affects everyone, but the risk of severe illness is higher in:
- Infants (especially under 6–12 months) and premature babies
- Adults 65+
- People with chronic lung disease (asthma, COPD), heart disease, or neurological conditions
- Immunocompromised individuals (cancer therapy, organ transplant, advanced HIV)
In children, HMPV accounts for a notable share of hospitalizations for lower respiratory tract infections, often
comparable to RSV in some seasons. In long-term care settings, outbreaks can lead to significant morbidity among
residents.
Seasonality and outbreak patterns
In many countries, human metapneumovirus activity peaks in late winter and spring, often after influenza and overlaps partly with RSV. However, seasonality can shift year to year and by region, and disruptions in typical respiratory virus patterns (for example, after COVID-19 mitigation measures) have led to off-season surges in some places.
Household and school spread: practical examples
Close-contact environments—households, daycare centers, schools—are ideal for spread. A coughing child touches a doorknob, a sibling rubs their nose, and within days multiple family members have symptoms. Simple steps like frequent handwashing, opening windows for fresh air, and masking when symptomatic reduce chain transmission. If your child’s school reports increased hMPV cases or “viral pneumonia,” reinforcing these habits at home can help limit spread.
Diagnosis and Testing for HMPV
When to test (and when you don’t need a test)?
Most people with mild symptoms don’t need specific testing because treatment is the same supportive care. Testing may
be useful if you are very young, elderly, immunocompromised, have severe or worsening symptoms, or if the result
might change clinical decisions (e.g., hospital infection control, stopping unnecessary antibiotics). If your condition does
not improve after trying home measures, book a physical visit to a doctor with Apollo 24|7.
PCR and respiratory panels vs. rapid antigen tests
The most common confirmatory test is a PCR-based respiratory panel on a nasal swab, which can detect HMPV along
with RSV, influenza, and SARS-CoV-2. Rapid antigen tests for HMPV are less widely available and generally less sensitive. Viral culture is rarely used outside research. Some clinicians may order simple blood tests (like CBC or CRP) to assess severity or rule out bacterial coinfection; Apollo 24|7 offers a convenient home collection for tests like CBC or
CRP if your clinician recommends them.
Distinguishing HMPV from RSV, flu, and COVID-19
Clinically, human metapneumovirus can look like RSV or flu, and symptoms overlap with COVID-19. Compared with
influenza, HMPV often has more cough/wheeze and less abrupt high fever. Compared with COVID-19, loss of
taste/smell is less common. Age and risk factors guide clinicians, but only testing can definitively tell viruses apart, especially during peak respiratory seasons. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.
Treatment, Recovery, and When to Seek Care
Home care that actually helps (hydration, fever control, rest)
There is no specific antiviral for HMPV. For most people, supportive care works well:
- Hydration: Warm fluids and frequent sips; for toddlers, oral rehydration solutions if intake is poor.
- Fever and pain: Acetaminophen or ibuprofen as directed for age/weight.
- Cough: Honey for children over 1 year; humidified air; saline nasal sprays; avoid OTC cough/cold mixes in young
children unless advised.
Rest and pacing: Expect to feel tired for several days; return to activity gradually.
Inhalers, oxygen, and hospital care: who needs what
People with asthma or COPD may benefit from using their prescribed reliever inhaler during an HMPV flare. In moderate to severe lower respiratory involvement, clinicians may consider inhaled bronchodilators. Oxygen and hospital monitoring are needed if oxygen levels drop or breathing becomes labored. Antibiotics are not effective against viruses; they’re reserved for suspected bacterial complications like bacterial pneumonia or ear infections. In immunocompromised patients, clinicians monitor closely because the disease can be more severe.
Warning signs, timelines, and follow-up
Most uncomplicated illnesses improve in 7–14 days. Seek care urgently for breathing difficulty, persistent high fever,
confusion, signs of dehydration, or oxygen saturation under 92%. If cough or wheeze persists beyond two weeks, especially with fatigue or chest discomfort, a check-in with a clinician helps rule out complications like secondary bacterial infection or asthma exacerbation. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.
Apollo 24|7: when telehealth or lab support makes sense
Use telehealth if you need guidance on home care, dosing for fever medicines, or to assess whether in-person care is
needed. If a clinician recommends labs (for example, CBC or CRP) to evaluate severity, Apollo 24|7 offers a
convenient home collection. For worsening symptoms or high-risk patients, book a physical visit to a doctor with
Apollo 24|7.
Prevention: Simple Steps That Work
Hand hygiene, masks, and ventilation at home
- Wash hands often with soap for 20 seconds; use sanitizer (≥60% alcohol) if soap isn’t available.
- Wear a mask when you are sick or caring for someone ill—especially around infants and older adults.
- Improve ventilation: open windows, use exhaust fans, or run HEPA/air purifiers to dilute indoor viruses.
- These steps reduce risk not only for HMPV but also RSV, flu, and COVID-19. Related term: how to disinfect for
respiratory viruses.
Cleaning high-touch surfaces the right way
HMPV can survive on surfaces for a short period. Clean frequently touched surfaces (doorknobs, phones, toys) daily
when someone is sick. Use household disinfectants as directed; ensure appropriate contact time. Avoid sharing cups and
utensils during illness.
Protecting high-risk family members
- Create “sick zones” at home: the ill person uses one bedroom/bathroom if possible, with masks during brief shared-
space interactions. - Time visits: postpone visits to newborns or elderly relatives until you’re fever-free for 24 hours and improving; consider
masking for a few extra days. - Vaccinate for other respiratory illnesses (flu, COVID-19) to reduce overall burden and confusion. While there’s no
HMPV vaccine yet, these steps lower the chance of multiple infections at once.
What’s Next: Vaccines, Research, and Common Questions?
Vaccine and monoclonal antibody pipeline
Researchers are working on HMPV vaccines using approaches similar to RSV: protein subunit, vector-based, and
mRNA platforms. Monoclonal antibodies targeting HMPV fusion (F) protein are also under study, potentially for high-
risk groups in the future. No vaccine or monoclonal is yet approved for routine use as of now, but clinical trials are
ongoing.
Long-term outcomes, reinfection, and immunity
After infection, immunity provides some protection but wanes over time, and people can be reinfected, often with milder
illness in healthy adults. Children and older adults can experience prolonged cough or wheeze after an HMPV
infection, similar to other viral respiratory infections.
Myths vs. facts
- “Antibiotics cure HMPV.” False—antibiotics target bacteria, not viruses.
- “HMPV is rare.” False—HMPV circulates globally and is a common cause of coughs and chest colds, especially late winter to spring.
“You can’t catch HMPV twice.” False—reinfections occur across the lifespan, though they tend to be less severe in
healthy adults.
Where to find reliable updates?
For trustworthy updates, check the CDC, NIH/NIAID, your national public health authority, and peer-reviewed
journals. If you’re unsure how new guidance applies to your health situation, consult a doctor online with Apollo 24|7.
Conclusion
Human metapneumovirus is part of the familiar family of winter and spring respiratory viruses, but it doesn’t have to catch you off guard. Understanding how HMPV spreads, who’s most at risk, and what symptoms to watch for can help you respond with confidence. For most healthy people, simple home care—hydration, rest, and fever control—leads to recovery within a couple of weeks. For infants, older adults, and those with chronic or immune conditions, early attention to warning signs and quick access to care make a real difference.
While there’s no dedicated HMPV treatment or vaccine yet, prevention remains powerful: wash hands often, mask when you’re sick, ventilate indoor spaces, and avoid close contact with vulnerable people until you’re feeling better. If you’re unsure whether testing or an in-person visit is needed, or your symptoms aren’t improving, consult a doctor online with Apollo 24|7. Preparing your household with these practical steps can help you navigate HMPV season more safely—and protect the people you love.
Consult a Top General Physician
Consult a Top General Physician

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ajay K Sinha
General Physician/ Internal Medicine Specialist
30 Years • MD, Internal Medicine
Delhi
Apollo Hospitals Indraprastha, Delhi
(200+ Patients)
Consult a Top General Physician

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Ajay K Sinha
General Physician/ Internal Medicine Specialist
30 Years • MD, Internal Medicine
Delhi
Apollo Hospitals Indraprastha, Delhi
(200+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
1) How long does HMPV last?
Most people feel better in 7–14 days, though a cough can linger for a few weeks. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7.
2) Is HMPV contagious, and for how long?
Yes. People are typically contagious for several days, starting around symptom onset. Young children may shed longer. Good hygiene and masking when sick reduce the spread.
3) How is HMPV different from RSV or the flu?
Symptoms overlap. HMPV and RSV can both cause wheezing and bronchiolitis; flu often has a sudden high fever and severe body aches. Only testing can tell viruses apart definitively.
4) Do I need antibiotics for HMPV?
No. Human metapneumovirus is viral, so antibiotics don’t help unless there’s a suspected bacterial complication like pneumonia or an ear infection.
5) Is there a vaccine for HMPV?
Not yet. Vaccines and monoclonal antibodies are in development, especially for high-risk groups. Watch for updates from public health sources and your clinician.