Minimal Access Laparoscopic Surgery: A Complete Guide
Know about minimal access laparoscopy surgery, what it is, how it works, comparisson with traditional method, benefits, risks, limits, procedure, recovery, myths, facts and more.

Written by Dr. J T Hema Pratima
Reviewed by Dr. D Bhanu Prakash MBBS, AFIH, Advanced certificate in critical care medicine, Fellowship in critical care medicine
Last updated on 13th Jan, 2026
Introduction
If you’ve been told you may need “keyhole” surgery, you’ve likely heard the term minimal access laparoscopic surgery. This modern approach uses tiny cuts, a camera, and delicate instruments to perform operations that once required large incisions. For most people, that can mean less pain, smaller scars, and a quicker return to normal life compared with open surgery.
In this complete guide, written for the general public, we explain what minimal access laparoscopic surgery is, how it works, which general surgery procedures are commonly done this way, and what to expect before, during, and after your operation. We break down benefits and risks in plain language, explore robotic and single-incision options, and share evidence-based recovery tips you can use.
If you’re considering minimal access laparoscopic surgery, this guide is your step-by-step companion from consultation to recovery.
Consult Top Surgeon for Personalised Advice
What Is Minimal Access Laparoscopic Surgery?
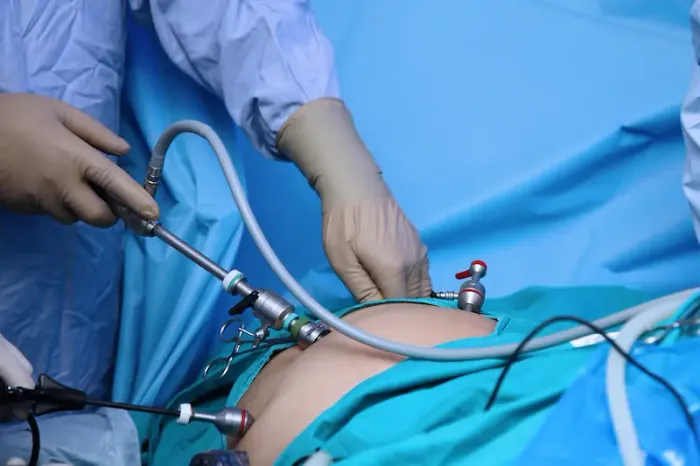
Minimal access laparoscopic surgery often called keyhole or minimally invasive surgery is a technique where surgeons operate through several small cuts (typically 0.5–1 cm), inserting a camera (laparoscope) and long, slim instruments to perform the procedure. The camera broadcasts magnified images to a high-definition screen, allowing the team to see inside with remarkable clarity.
How it differs from open surgery:
1. Incisions: Instead of one large incision (10–20 cm) in open surgery, laparoscopy uses multiple tiny incisions.
2. Visualisation: An HD (sometimes 4K or 3D) camera provides magnified views, helping with precision.
3. Tauma: Smaller incisions and less tissue disruption generally result in less pain and faster recovery.
How Laparoscopy Works: Tools, Camera, and CO2
Surgeons create several small entry points (ports) using trocars—hollow sleeves that allow instruments to pass into the abdomen. A laparoscope (camera) goes through one port, while other ports hold working instruments like graspers, scissors, staplers, suturing devices, and energy instruments (for sealing blood vessels).
Key elements:
1. Pneumoperitoneum: The abdomen is gently inflated with carbon dioxide (CO2) to create working space and move the abdominal wall away from the organs. CO2 is used because it’s non-flammable and easily absorbed by the body.
2. Visualisation: Modern systems provide HD, 4K, or even 3D views. Some centres add fluorescence imaging (using indocyanine green dye) to highlight bile ducts or blood flow, improving safety during complex steps.
3. Energy devices: Advanced bipolar or ultrasonic devices seal vessels efficiently, reducing the need for traditional sutures and helping minimise bleeding.
Common General Surgery Procedures Done Laparoscopically
Many core general surgery operations can be performed via minimal access laparoscopic techniques.
1. Laparoscopic cholecystectomy (gallbladder removal): The most common laparoscopic operation worldwide, typically for gallstones or gallbladder inflammation. Recovery is often days rather than weeks, with lower infection risk than open surgery.
2. Laparoscopic appendectomy: For appendicitis, laparoscopy often shortens hospital stay, reduces wound infections, and speeds return to normal activity compared with open surgery, according to Cochrane reviews.
3. Hernia repair (inguinal, ventral/abdominal wall): Laparoscopic hernia repair can reduce wound complications and pain and allows bilateral inguinal hernias to be fixed through the same small incisions. Recovery is commonly measured in days, not weeks, although technique choice is individualised.
4. Anti-reflux surgery (e.g., Nissen fundoplication): Laparoscopy is the standard approach in many centres for persistent GERD not controlled by medications, offering smaller scars and faster recovery.
5. Colorectal surgery: Many colon and rectal operations are done minimally invasively, which can reduce blood loss and shorten hospital stay. Not all cases are suitable, depending on anatomy, prior surgeries, and disease severity.
6. Bariatric (weight-loss) surgery: Sleeve gastrectomy and gastric bypass are commonly performed laparoscopically or robotically, which helps with mobilisation and recovery in higher-BMI patients.
Benefits Compared with Open Surgery
Evidence consistently shows meaningful benefits of minimal access laparoscopic surgery compared with open approaches for many procedures.
1. Less pain: Smaller incisions and less tissue disruption translate to less postoperative pain for most patients].
2. Shorter hospital stay: Many laparoscopic procedures are same-day or involve 1–2 nights in hospital, while open surgery may require longer stays].
3. Lower infection risk: Keyhole incisions and reduced tissue handling lower the risk of surgical site infections]. WHO guidance recognizes laparoscopy as a strategy to reduce SSI risk where feasible.
4. Faster return to work and daily life: Patients often resume normal activities and work sooner, an important “quality of life” outcome.
5. Fewer wound-related complications: There are typically fewer issues like wound breakdown or large incisional hernias after laparoscopy.
Risks, Limits, and When Open Surgery Is Safer
All surgery carries risks, and minimal access laparoscopic surgery is no exception.
Potential risks:
• Bleeding, infection, or injury to nearby organs (e.g., bowel, bladder, blood vessels). These risks are generally low but vary by procedure [1–4].
• Anesthesia-related effects: Temporary sore throat, nausea, or dizziness are common; serious complications are rare.
• Gas-related discomfort: Shoulder-tip pain or bloating from CO2 usually improves in 24–72 hours.
• Blood clots (DVT/PE): Early mobilization, compression devices, and sometimes medication reduce this risk.
Contraindications and considerations:
1. Unstable patients or those unable to tolerate anesthesia positioning (steep head-up or head-down) may not be candidates.
2. Severe cardiopulmonary disease can make pneumoperitoneum risky.
3. Very extensive adhesions or certain emergency scenarios may favor an open approach.
If you have persistent symptoms (e.g., pain, fever, vomiting) beyond two weeks post-op, consult a doctor online with Apollo24|7 for further evaluation or book an in-person visit if advised. Seek emergency care for severe pain, chest pain, shortness of breath, or uncontrolled bleeding.
Robotic and Single-Incision Variants
Robotic-assisted laparoscopy:
A surgeon controls robotic instruments from a console. The robot provides wristed instruments (greater dexterity), tremor filtration, and high-definition 3D vision. This can be beneficial for complex hernias, colorectal surgery in tight spaces, or revisional bariatric procedures. While “robotic” sounds automated, the surgeon is in control throughout. Costs and access vary by hospital.
Single-incision laparoscopic surgery (SILS):
Some procedures can be done through one incision (often at the belly button) for an even more “minimal” cosmetic result. However, SILS can be technically challenging and may increase instrument crowding. Patient selection matters, and not all operations are appropriate.
Preparing for Minimal Access Laparoscopic Surgery
Preparation often follows ERAS (Enhanced Recovery After Surgery) principles, which have been shown to reduce complications and speed recovery [6].
Pre-op essentials:
Tests: Depending on age and health—blood counts, electrolytes, kidney/liver tests, ECG, chest X-ray, and sometimes blood sugar control (HbA1c) if you have diabetes. Apollo24|7 offers convenient home collection for routine pre-op tests like CBC, CMP, and HbA1c.
Medications: Your team will advise which medicines to continue or pause (e.g., blood thinners). Bring a complete list to your pre-op visit.
• Fasting: Typically no solid food 6–8 hours before anesthesia; clear fluids may be allowed up to 2 hours pre-op per local policy.
• Smoking/alcohol: Stopping smoking and reducing alcohol intake improves healing and lung function.
ERAS-inspired steps you control:
1. Nutrition: Adequate protein intake supports healing; some protocols use pre-op carbohydrate drinks.
2. Activity: Stay active up to surgery day; even gentle walking helps.
3. Bowel prep: Only for certain operations (e.g., colorectal); follow your surgeon’s instructions exactly.
The Day of Surgery: What You’ll Experience
Before surgery:
• Check-in, consent review, and final questions with your surgeon and anesthesiologist.
• IV line placement; sometimes a regional block for pain control.
During surgery:
• General anesthesia is typical. You’ll be positioned to optimize the surgical field (slight tilt depending on the operation).
• The abdomen is insufflated with CO2, ports placed, and the procedure performed under camera guidance.
• The team checks for bleeding, removes instruments, and closes the tiny incisions.
After surgery:
1. Recovery room monitoring: Breathing, pain, nausea control, and early mobilization.
2. Discharge: Many laparoscopic patients go home the same day or after an overnight stay, depending on the procedure and your recovery milestones [1–2].
Recovery and Aftercare at Home
It includes:
Pain and activity includes:
A Pain usually improves rapidly; many patients switch from prescription pain meds to acetaminophen/NSAIDs within a couple of days if appropriate.
Walk frequently to reduce clot risk and bloating. Avoid heavy lifting until your surgeon clears you—often 2–4 weeks depending on the procedure.
Wound care:
Keep incisions clean and dry. Showering is often allowed after 24–48 hours; avoid soaking until incisions heal.
Expect mild bruising or swelling around port sites.
Diet and digestion:
Many resume light meals soon after surgery. After gallbladder removal, a temporary low-fat diet may help. Bowel function can be sluggish initially; fiber and fluids help.
Shoulder-tip pain from CO2 usually eases in 1–3 days.
When to call your doctor:
Fever over 38°C, worsening redness, pus, uncontrolled pain, persistent vomiting, chest pain, or shortness of breath.
If symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for further evaluation, or book a physical visit if your recovery isn’t following the expected course.
Myths vs Facts about Laparoscopic Surgery
1. Myth: Tiny incisions mean zero risk.
2. Fact: Risks are lower for many issues (especially wound infections), but not zero. Serious complications are uncommon but possible [1–3].
3. Myth: Robotic surgery is done by a robot autonomously.
4. Fact: The surgeon controls the instruments at all times.
1. Myth: Laparoscopy always has a faster recovery.
2. Fact: Usually—but not always. Complex disease, prolonged operations, or patient comorbidities can lengthen recovery.
Myth: Laparoscopy isn’t suitable if you’ve had prior surgeries.
Fact: Prior surgeries increase difficulty, but many patients can still have minimal access approaches with experienced teams.
Choosing a Surgeon and Hospital
What to look for:
1. Experience and volume: Surgeons and centers that perform your procedure frequently tend to have smoother workflows and outcomes.
2. Training and credentials: Fellowship training, participation in recognized programs (e.g., SAGES), and maintenance of skills (e.g., FLS—Fundamentals of Laparoscopic Surgery).
3. Team and resources: Anesthesia, nursing, and recovery teams aligned with ERAS and minimally invasive protocols.
4. Communication: Clear expectations about benefits, risks, recovery, and when to seek help.
Conclusion
Minimal access laparoscopic surgery has transformed general surgery by pairing precision with smaller incisions and faster healing. For many common operations—gallbladder removal, appendectomy, hernia repair, and more—patients can expect less pain, shorter hospital stays, fewer wound problems, and a quicker return to daily life compared with open surgery. At the same time, it’s important to remember that laparoscopy is still real surgery: benefits and risks vary by your health profile, the complexity of your case, and the experience of your team.
If your recovery doesn’t follow the expected timeline, or symptoms persist beyond two weeks, consult a doctor online with Apollo24|7 for personalized advice or book an in-person review.
Consult Top Surgeon for Personalised Advice
Consult Top Surgeon for Personalised Advice

Dr. D.s. Sai Babu
Surgical Gastroenterologist
25 Years • F.S.G.E, (PDCC- NIMS) F.M.A.S, F.A.C.S, DIP. M.A.S, F.A.C.S (USA) M.S (GEN-SURGERY) – NTR UNIVERSITY OF HEALTH SCIENCES. M.B.B.S ANDHRA UNIVERSITY.
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda

Dr Karthik Maripeddi
Urologist
13 Years • MBBS MS FMAS MCh URO(OSM)
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda

Dr. Premkumar Balachandran
General and Laparoscopic Surgeon
22 Years • MBBS, MS, FICS, DMAS, FMAS, FRS, FIAGES, Dip. ALS, FCP
Chennai
Apollo Hospitals Greams Road, Chennai
(175+ Patients)

Dr. Ishita Mandal
General Surgeon
7 Years • MBBS(hons.), MS(general surgery), General and laparoscopic surgeon
Kolkata
VDC Clinic, Kolkata

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult Top Surgeon for Personalised Advice

Dr. D.s. Sai Babu
Surgical Gastroenterologist
25 Years • F.S.G.E, (PDCC- NIMS) F.M.A.S, F.A.C.S, DIP. M.A.S, F.A.C.S (USA) M.S (GEN-SURGERY) – NTR UNIVERSITY OF HEALTH SCIENCES. M.B.B.S ANDHRA UNIVERSITY.
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda

Dr Karthik Maripeddi
Urologist
13 Years • MBBS MS FMAS MCh URO(OSM)
Hyderguda
Apollo Hospitals Hyderguda, Hyderguda

Dr. Premkumar Balachandran
General and Laparoscopic Surgeon
22 Years • MBBS, MS, FICS, DMAS, FMAS, FRS, FIAGES, Dip. ALS, FCP
Chennai
Apollo Hospitals Greams Road, Chennai
(175+ Patients)

Dr. Ishita Mandal
General Surgeon
7 Years • MBBS(hons.), MS(general surgery), General and laparoscopic surgeon
Kolkata
VDC Clinic, Kolkata

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
1) Is minimal access laparoscopic surgery safe for older adults?
Yes, many older adults benefit from smaller incisions, less pain, and earlier mobility. A pre-op assessment tailors anesthesia and ERAS steps to reduce risk. If you’re concerned about fitness for anesthesia, consult a doctor online with Apollo24|7.
2) How long is the recovery after a laparoscopic cholecystectomy?
Many people return to light activities within a few days and work within 1–2 weeks, though recovery varies. Follow your surgeon’s plan for lifting and diet progression.
3) What if I’ve had prior abdominal surgeries—can I still have laparoscopy?
Often yes, but adhesions can increase complexity. Your surgeon may discuss a diagnostic laparoscopy first or a hybrid plan. Ask about the chance of conversion to open surgery.
4) Will I have shoulder pain after laparoscopy?
Some people feel shoulder-tip pain from CO2; it typically lasts 1–3 days. Walking, gentle movement, and your pain plan help ease it.
5) What pre-op tests do I need, and can I do them at home?
Tests vary by age and health (e.g., CBC, electrolytes, kidney/liver function, ECG). Apollo24|7 offers convenient home collection for many pre-operative tests to simplify your preparation.


 7 Amazing Health Benefits.webp)
