Pleural Effusion: Signs, Causes, and Types Explained
Discover pleural effusion, including its causes, symptoms, types, diagnosis, and treatment options. Learn when to seek medical care and how to manage recovery.

Written by Dr. Siri Nallapu
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026
Introduction
If breathing feels harder than usual or a persistent chest heaviness won’t go away, one possible reason is a pleural effusion—an abnormal buildup of fluid between the thin layers of tissue that line your lungs and chest wall. While “fluid on the lungs” sounds alarming, pleural effusion is common and has many causes, from heart failure to infections like pneumonia and conditions such as cancer. Most people feel better once the cause is identified and the extra fluid is treated.
In this guide, you’ll learn what pleural effusion is, the signs and symptoms to watch for, what causes it, and the different types including transudative, exudative, empyema, and chylothorax. We’ll explain how doctors diagnose pleural effusion using chest X-rays, ultrasound, and thoracentesis, as well as treatment options ranging from medications to minimally invasive procedures. You’ll also find practical tips for recovery, when to seek help, and what to expect over time, helping you navigate pleural effusion with confidence.
What Is a Pleural Effusion?
A pleural effusion is a buildup of fluid in the pleural space—the thin, lubricated gap between your lungs and the inner chest wall. Normally, only a small amount of fluid sits there to help the lungs glide smoothly as you breathe. When more fluid accumulates, it can compress the lung, leading to shortness of breath, chest discomfort, and a dry cough. Severe effusions can make it difficult to get enough oxygen.
Two main mechanisms cause pleural effusions. First, excess fluid can leak into the pleural space due to pressure or protein shifts in the bloodstream, as seen in heart failure or liver disease. Second, local inflammation or injury in the chest can produce protein-rich fluid, pus, or blood, as in pneumonia, cancer, or trauma. Pleural effusions are classified by type because this points to the underlying cause and guides treatment.
The parietal pleura lines the chest wall, and the visceral pleura covers the lung. Tiny blood vessels continually produce and drain fluid. When production exceeds drainage—or drainage is blocked—fluid accumulates. Pleural effusion is distinct from pneumonia, which affects the lung tissue itself; draining the pleural space often brings quick relief.Consult Top Specialists
Signs and Symptoms You Shouldn’t Ignore
Here’s what to watch for:
Symptoms vary depending on fluid volume and how quickly it accumulates. The most common symptom is shortness of breath, particularly with exertion or when lying down, because the fluid restricts lung expansion. Some people describe a “tight band” around the chest or difficulty taking a deep breath. Other symptoms include a dry cough, chest pain (often sharp and worsens with deep breaths), and fatigue.
On examination, percussion over fluid sounds dull. Breath sounds may be decreased or absent on the affected side. Large effusions can shift the trachea or heart sounds. Small effusions may produce few symptoms and are sometimes found incidentally on chest X-rays.
Red flags requiring urgent care include severe or rapidly worsening breathlessness, chest pain at rest, rapid breathing, bluish lips or fingertips, and fainting. If you have heart or lung conditions and notice sudden changes in breathing or leg swelling, seek prompt evaluation. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. Seek emergency care immediately for severe breathing difficulty.
What Leads to a Pleural Effusion? (Causes and Mechanisms)
Here’s why pleural fluid builds up:
Transudative pleural effusions result from systemic factors that alter pressure and fluid balance. The most common cause is heart failure, where high pressures in the lungs’ blood vessels push fluid outward. Other causes include cirrhosis and kidney disease. These effusions are usually clear and low in protein.
Exudative pleural effusions arise from local inflammation or damage in the chest. Pneumonia can inflame the pleura and produce a parapneumonic effusion; if infected, pus collects (empyema). Cancer can block drainage or inflame the pleura, leading to malignant pleural effusion. Pulmonary embolism, tuberculosis, pancreatitis, and autoimmune diseases are other exudative causes. These effusions are higher in protein and may contain white blood cells, bacteria, or cancer cells.
Rapidly developing effusions after trauma suggest blood (hemothorax). Effusions that fluctuate with weight or salt intake often suggest heart failure or kidney disease. A slowly enlarging unilateral effusion in an older adult, especially with weight loss, may indicate malignancy.
Types of Pleural Effusion (and What Each One Means)
Here’s how pleural effusions are categorised:
Transudative pleural effusion
• Usually due to heart failure, cirrhosis, or nephrotic syndrome
• Often bilateral and clear, with low protein and low LDH; improves when the underlying condition is treated
Exudative pleural effusion
• Higher protein/LDH, often due to infections, cancer, pulmonary embolism, or autoimmune disease
• Requires targeted investigation and may need drainage
Parapneumonic effusion and empyema
• Accompanies pneumonia; if bacteria invade, it becomes empyema (pus)
• Low pleural fluid pH or frank pus indicates urgent drainage and antibiotics; intrapleural medications can help break down thick pus
Malignant pleural effusion
• Caused by cancer (lung, breast, lymphoma)
• May require repeated thoracentesis, an indwelling pleural catheter, or pleurodesis
Tuberculous effusion
• Typically an exudate with high lymphocytes and elevated ADA; requires anti-tuberculous therapy
Hemothorax
• Blood in the pleural space, usually from trauma or post-surgical bleeding; requires urgent evaluation
Chylothorax vs pseudochylothorax
• Chylothorax: Milky fluid rich in triglycerides; managed with drainage, diet, or surgery
• Pseudochylothorax: Long-standing effusion with high cholesterol, often from chronic inflammation
Consult Top Specialists
Loculated and subpulmonic effusions
• Loculated: Pockets of fluid trapped by adhesions; more challenging to drain
• Subpulmonic: Fluid beneath the lung and diaphragm; ultrasound helps clarify
How Doctors Diagnose Pleural Effusion
Here’s how diagnosis works:
Imaging
• Chest X-ray shows blunted costophrenic angle and fluid layering; lateral views help identify free-flowing fluid
• Ultrasound detects small amounts of fluid, guides safe drainage, and identifies loculations
• CT scan provides detailed assessment of underlying lung disease and complex effusions
Thoracentesis and pleural fluid analysis
• Needle removes fluid for analysis and symptom relief
• Tests include protein, LDH, glucose, pH, cell counts, Gram stain, cytology, triglycerides, and ADA
Light’s criteria
• Classifies effusions as exudates if pleural fluid protein/serum protein >0.5; pleural fluid LDH/serum LDH >0.6; or pleural fluid LDH >2/3 the upper limit of normal serum LDH
Advanced testing
• If cancer is suspected, options include repeat sampling, image-guided pleural biopsy, thoracoscopy, or PET-CT
• For TB, ADA and interferon-gamma testing assist diagnosis
If blood tests are needed to assess causes, Apollo 24|7 offers home collection with fast reporting.
Treatment Options: From Simple to Specialised
Here’s how pleural effusions are treated:
Treat the underlying cause
• Transudative: Diuretics, fluid/salt restriction, and optimisation of heart, liver, or kidney function
• Exudative: Antibiotics for infections, anti-TB therapy, anticoagulation for clots, or targeted cancer treatment
Procedures to remove fluid
• Thoracentesis for rapid relief; may need repeating
• Chest tube drainage for large, infected, or bloody effusions; intrapleural medications or surgery if complex
Preventing recurrence
• Pleurodesis seals pleural layers to reduce repeat fluid buildup
• Indwelling pleural catheter allows intermittent home drainage
Recovery and follow-up
• Follow-up imaging monitors reaccumulation and lung expansion
• Pulmonary rehabilitation and breathing exercises help recovery
If symptoms persist or worsen, seek urgent care or consult a doctor online with Apollo 24|7.
Complications, Outlook, and Living Well
Here’s what to consider:
Potential complications
• Untreated infections can lead to trapped lung
• Procedure-related complications are rare but can include pain, bleeding, infection, or pneumothorax
• Re-expansion pulmonary oedema is uncommon but possible
Outlook
• Prognosis depends on the cause: heart failure and pneumonia-related effusions often resolve; malignant effusions may recur
• Focus is on symptom relief and quality of life
Living well
• Sleep with head elevated if breathlessness worsens lying flat
• Pace activities and use breathing exercises
• Monitor weight if heart failure is present, reduce salt, and stay updated on vaccinations
• Track pillows needed and walking tolerance to help tailor therapy
Conclusion
Pleural effusion may sound intimidating, but understanding it clarifies the path forward. It’s fluid around the lungs that restricts expansion, causing shortness of breath, chest tightness, and dry cough.
Recognising the type of effusion guides treatment. Transudative effusions respond to optimising heart or kidney function. Exudative effusions, caused by infections, cancer, TB, or clots, may need thoracentesis or chest tube drainage. Many patients feel immediate relief after fluid removal. Longer-term solutions like pleurodesis or an indwelling pleural catheter improve comfort and reduce hospital visits.
Modern ultrasound guidance and evidence-based protocols make diagnosis and treatment safer. Persistent breathlessness or chest discomfort warrants prompt consultation. Apollo 24|7 offers online consultations and home blood collection for relevant tests. With proper care, most people can breathe easier and return to daily activities.Consult Top Specialists
Consult Top Specialists

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
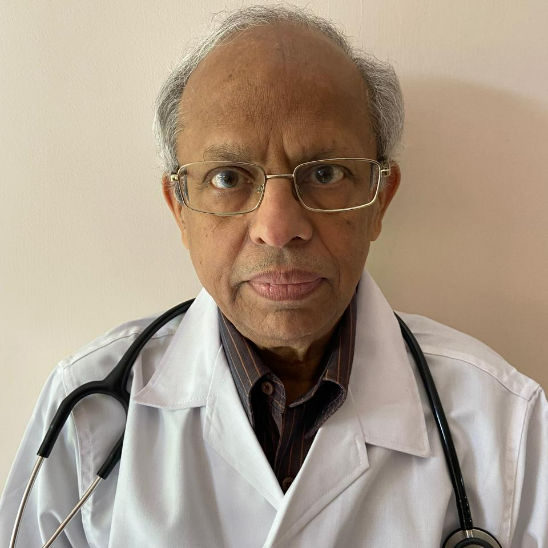
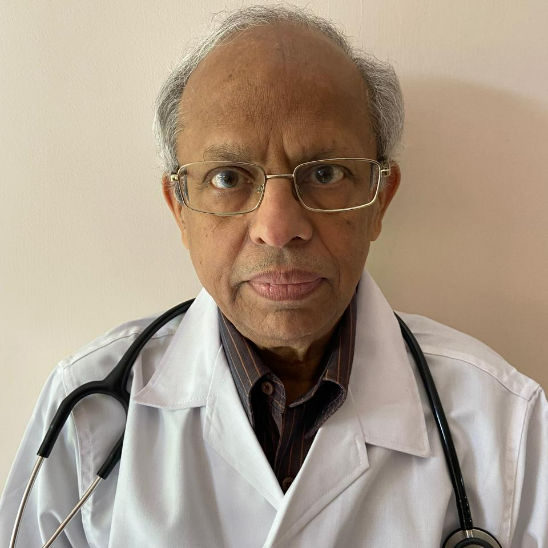
Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
Consult Top Specialists

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
Consult Top Specialists

Dr. P Sravani
Pulmonology Respiratory Medicine Specialist
3 Years • MBBS, MD
Visakhapatnam
Apollo Clinic Vizag, Visakhapatnam
Dr. Ambuj Kumar
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS, MD (Pulmonary Medicine)
New Delhi
Smriti Gynaecology and Lung Centre, New Delhi

Dr Rakesh Bilagi
Pulmonology Respiratory Medicine Specialist
10 Years • MBBS MD PULMONOLOGIST
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Dr. E Prabhakar Sastry
General Physician/ Internal Medicine Specialist
40 Years • MD(Internal Medicine)
Manikonda Jagir
Apollo Clinic, Manikonda, Manikonda Jagir
(150+ Patients)

Dr. K Prasanna Kumar Reddy
Pulmonology Respiratory Medicine Specialist
16 Years • MBBS, DTCD (TB&CHEST), DNB (PULM MED), FCCP
Hyderabad
Apollo Medical Centre Kondapur, Hyderabad
More articles from General Medical Consultation
Frequently Asked Questions
1) Is pleural effusion the same as pneumonia?
No. Pneumonia is an infection inside the lungs; pleural effusion is fluid in the space around the lungs. Pneumonia can cause a “parapneumonic effusion,” which sometimes needs drainage.
2) How is a pleural effusion diagnosed?
Doctors use imaging (chest X-ray, ultrasound, CT) and often thoracentesis (pleural tap) for pleural fluid analysis. Light’s criteria help classify exudative versus transudative pleural effusions.
3) What are the most common causes of pleural effusion?
Heart failure (transudative), pneumonia and empyema (exudative), and cancers like lung or breast (malignant pleural effusion) are common causes.
4) Will the fluid come back after it’s drained?
Sometimes. If the underlying cause persists (e.g., cancer), fluid can recur. Options like pleurodesis or an indwelling pleural catheter help prevent or manage recurrence.
5) When should I see a doctor?
Seek urgent care for severe or rapidly worsening breathlessness. If symptoms persist beyond two weeks or you’re unsure of the cause, consult a doctor online with Apollo 24|7 for guidance.
.webp)