Prostate Gland Problems: BPH, Prostatitis & Cancer Guide
Learn about the three main prostate problems—BPH, prostatitis, and prostate cancer. Discover symptoms, diagnosis, treatments, prevention tips, and when to consult a doctor.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Md Yusuf Shareef MBBS
Last updated on 13th Jan, 2026
Introduction
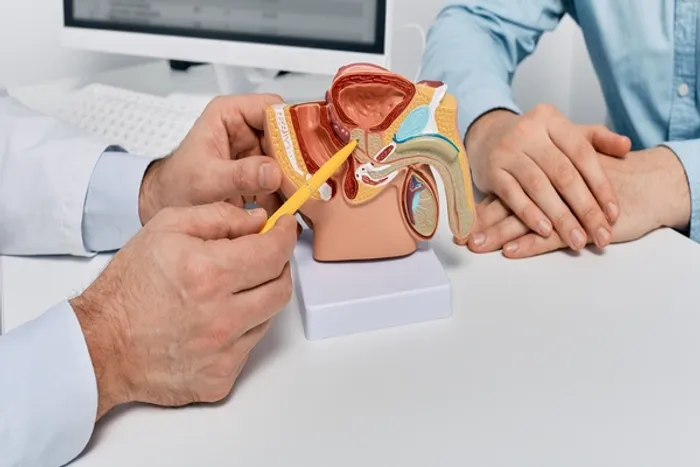
If you’re over 40, chances are you’ve heard about prostate problems—but knowing which issues to watch for and what to do next can feel confusing. The prostate gland is a small, walnut-sized organ just below the bladder, and as men age, it becomes prone to three main issues: benign prostatic hyperplasia (BPH, or an enlarged prostate), prostatitis (inflammation, often with pelvic pain), and prostate cancer. This guide breaks down what the prostate does, how these problems differ, the signs to take seriously, and modern diagnostic and treatment options. We also share lifestyle tips that support prostate health, explain screening in plain language, and highlight less invasive options. Where appropriate, we point to how to consult a doctor online with Apollo 24|7 or use at-home test collection services. By the end, you’ll know what’s normal, what’s not, and how to take control of your prostate health with confidence.
Prostate Gland Basics—What It Does and How It Changes
Here's an overview of the prostate and why it matters:
Where the prostate sits and why it matters
The prostate is a small gland located under the bladder, wrapped around the urethra, the tube that carries urine out. It produces seminal fluid that nourishes and protects sperm. Because it encircles the urethra, even small changes—like swelling or growth—can affect urine flow, causing hesitancy, weak stream, or frequent nighttime urination (nocturia).
How the gland changes with age
With age and hormonal shifts, especially dihydrotestosterone (DHT), the prostate often grows. Many men never notice symptoms, but enlarged tissue can compress the urethra. Inflammation (prostatitis) can occur at any age, and the risk of prostate cancer rises with age, family history, and ancestry, particularly in men of African descent.
Why “prostate problems” can feel similar
Because the gland and urethra are closely linked, BPH, prostatitis, and cancer can share urinary symptoms. Tests like prostate-specific antigen (PSA), digital rectal exam (DRE), urinalysis, and imaging are important to distinguish among causes.
Consult Top Specialists
The 3 Main Prostate Gland Problems at a Glance
Here's what you need to know about each condition:
Benign Prostatic Hyperplasia (BPH)
- What it is: Noncancerous enlargement of the prostate that can squeeze the urethra.
- Common signs: Slow stream, straining, feeling of incomplete emptying, frequent urination, especially at night.
- Who’s affected: Very common with aging—about half of men by age 60, up to 90% by age 85 show BPH changes.
Prostatitis
- What it is: Inflammation of the prostate. Can be acute (bacterial), chronic bacterial, or chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) where infection isn’t found but pain persists.
- Common signs: Pelvic or perineal pain, painful urination, painful ejaculation, urinary frequency/urgency; fever or chills if acute infection.
- Who’s affected: Can affect younger and middle-aged men; it’s a leading cause of urology visits under age 50.
Prostate Cancer
- What it is: Malignant growth in the prostate gland.
- Common signs: Often none early on; sometimes similar urinary symptoms as BPH. Advanced disease may cause bone pain or weight loss.
- Who’s affected: Risk increases with age, family history, and African or Caribbean ancestry. Early detection improves survival.
Symptoms and Warning Signs—What to Watch For
Here's what to look out for:
Urinary changes
- Trouble starting or stopping, weak stream, dribbling, and nocturia are classic signs of BPH.
- Urgency, burning, or pelvic pressure may suggest prostatitis.
- Blood in urine or semen warrants prompt evaluation.
Pain and sexual function
- Dull ache in the lower back, groin, or perineum can indicate prostatitis.
- Painful ejaculation and erectile difficulties can occur with prostatitis or after some treatments.
- New, persistent bone pain may signal advanced prostate cancer.
When to seek care
- Urinary retention, fever with urinary pain, or severe pelvic pain requires urgent attention.
- Persistent symptoms beyond two weeks should be discussed with a clinician. Consult a doctor online with Apollo 24|7 if needed.
How Prostate Problems Are Diagnosed?
Here's how doctors confirm and monitor prostate conditions:
Initial evaluation
- History and physical examination, including DRE. A DRE can detect asymmetry, nodules, or tenderness.
- Lab tests: Urinalysis and urine culture check for infection; PSA assesses prostate activity.
Imaging and advanced tests
- Ultrasound (transrectal) and MRI for better visualization.
- Uroflowmetry and post-void residual measurement quantify obstruction in BPH.
If cancer is suspected, MRI-targeted biopsy can improve diagnostic accuracy.
Practical note on testing
Several factors can elevate PSA, including recent ejaculation or biking. Repeat testing after resolving infection or waiting 48 hours post-ejaculation improves accuracy. Apollo 24|7 offers home collection for routine tests like PSA, vitamin D, or HbA1c.
Problem 1: Benign Prostatic Hyperplasia (BPH)
Here's what to know about BPH:
How common BPH is and why it happens
BPH is extremely common with aging; DHT drives growth of inner prostate zones, narrowing the urethra. Risk factors include age, family history, metabolic syndrome, and low physical activity.
Symptoms, risks, and quality of life
Lower urinary tract symptoms include hesitancy, weak stream, straining, urgency, and nocturia. Severe obstruction can lead to bladder changes, infections, stones, or kidney strain.
Treatment options—stepwise approach
- Watchful waiting: Track symptoms, timed voiding, avoid bladder irritants.
- Medications: Alpha-blockers relax muscles; 5-alpha-reductase inhibitors shrink the gland; combination therapy for larger prostates.
- Minimally invasive procedures: Rezūm or UroLift for faster recovery.
- Surgery: TURP or HoLEP for severe obstruction or complications.
Problem 2: Prostatitis (Inflammation and Pelvic Pain)
Here's what you need to know:
Types and typical timelines
- Acute bacterial prostatitis: Sudden fever, chills, pelvic pain, painful urination—urgent antibiotics required.
- Chronic bacterial prostatitis: Recurrent UTIs with the same organism, intermittent discomfort.
- CP/CPPS: Pelvic or perineal pain lasting three months or more without infection; affects quality of life and sexual function.
Management strategies
- Bacterial forms: Culture-directed antibiotics, hydration, pain control, stool softeners.
- CP/CPPS: Multimodal care—alpha-blockers for voiding symptoms, anti-inflammatories, neuropathic pain agents, pelvic floor therapy, stress reduction.
- Lifestyle: Warm baths, avoid triggers, moderate caffeine, alcohol, spicy foods.
When to seek help
Fever, severe pelvic pain, or difficulty urinating requires urgent care. Persistent symptoms beyond two weeks should be evaluated online with Apollo 24|7 or in person.
Problem 3: Prostate Cancer—Risk, Screening, and Treatment
Here's the key information:
How common it is and who’s at risk
Prostate cancer is common in men. Risk increases with age, family history, and African or Caribbean ancestry. Early detection improves survival.
Screening basics—PSA and DRE
- PSA reflects prostate activity but can be elevated by BPH or prostatitis.
- Shared decision-making is recommended for ages 55–69; higher-risk men may discuss screening earlier (45–50).
If cancer is found—staging and options
- Low-risk cancers: Active surveillance with PSA, DRE, periodic MRI/biopsy.
- Localised higher-risk cancer: Surgery or radiation therapy.
- Advanced/metastatic: Hormonal therapy, chemotherapy, PSMA-targeted therapy.
Prevention and Lifestyle for a Healthier Prostate Gland
Here's practical guidance:
Diet and weight
Eat more vegetables, fruits, pulses, whole grains; limit processed meat and saturated fat. Obesity is linked to more severe urinary symptoms.
Movement and pelvic floor
Regular aerobic activity reduces urinary symptoms. Pelvic floor relaxation and strengthening help manage dribbling or pelvic pain.
Bladder-friendly habits
Limit evening fluids, caffeine, alcohol. Manage constipation to reduce pressure on the prostate and urethra.
Navigating Screening Decisions and PSA Nuances
Here's how to approach screening:
Pros and cons in plain language
- Early detection can save lives.
- Overdiagnosis of slow-growing cancers can lead to anxiety or unnecessary treatment.
- Individualised decision-making is key.
Fine-tuning the PSA conversation
- Repeat testing if elevations may be due to prostatitis or recent ejaculation.
- Additional tools like percent-free PSA, PSA density, MRI, and risk calculators help refine biopsy decisions. Consult a doctor online with Apollo 24|7 if uncertain.
Living Well with Prostate Problems—Practical Strategies
Here's how to manage day-to-day:
Daily routines that help
Morning hydration, tapering in the evening. Double-void before bed. Warm baths or compresses for pelvic discomfort.
Medication and device tips
Take alpha-blockers at night to reduce dizziness. Consider discreet urinals for travel. Use smartphone reminders for active surveillance.
Partner and mental well-being
Open communication about sexual effects or pelvic pain helps coping and intimacy. Brief counselling or sex therapy can assist couples.
Conclusion
Prostate health matters more than many men realise—urinary comfort, sexual function, sleep quality, and long-term well-being are all linked to this small gland. Most issues fall into BPH, prostatitis, or prostate cancer, and while symptoms can overlap, the path forward becomes clear with evaluation. Treatments have advanced: lifestyle strategies, medications, minimally invasive procedures, and sophisticated imaging allow personalised care. Screening for prostate cancer is not one-size-fits-all; informed, shared decision-making helps balance early detection with overdiagnosis risks. If you notice urinary changes or pelvic discomfort, start with small lifestyle adjustments, and consult a doctor online with Apollo 24|7 if symptoms persist. Home collection for tests like PSA, vitamin D, or HbA1c is available, making monitoring convenient. Attending to prostate health now pays off in comfort, function, and long-term well-being.
Consult Top Specialists
Consult Top Specialists

Dr. Moin Mohammed Bavakatti
Urologist
13 Years • MBBS, MS (General Surgery), Mch (Urology), DNB (Urology), Diploma in Minimal Access Surgery, Fellow of Internal College of Robotic Surgeons), Vinci Surgical system, Fellow in Endocrinology, Clinical and Research fellow in Laparoscopic Urology, Laser Endourology & Laparoscopic & Robotic Urology, Fellowship in 3D laparoscopic Urology
Bengaluru
Dr Moin Mohammed Bhavikatti Clinic, Bengaluru
(150+ Patients)
Dr. Mohammed Rehan Khan
Urologist
8 Years • MBBS, MS (General Surgery), Mch (Urology)
Barasat
Diab-Eat-Ease, Barasat

Dr. Kunal Kumar Mehar
Urologist
10 Years • Mbbs, Ms, Mch
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Yogesh Taneja
Urologist
15 Years • MBBS , MS (General surgery), DNB (Genito Urinary Surgery)
Gurugram
Procyon Health, Gurugram

Dr. Pramod B R
Urologist
10 Years • MBBS, MS, MRCS, MCh
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru
(50+ Patients)
Consult Top Specialists

Dr. Moin Mohammed Bavakatti
Urologist
13 Years • MBBS, MS (General Surgery), Mch (Urology), DNB (Urology), Diploma in Minimal Access Surgery, Fellow of Internal College of Robotic Surgeons), Vinci Surgical system, Fellow in Endocrinology, Clinical and Research fellow in Laparoscopic Urology, Laser Endourology & Laparoscopic & Robotic Urology, Fellowship in 3D laparoscopic Urology
Bengaluru
Dr Moin Mohammed Bhavikatti Clinic, Bengaluru
(150+ Patients)
Dr. Mohammed Rehan Khan
Urologist
8 Years • MBBS, MS (General Surgery), Mch (Urology)
Barasat
Diab-Eat-Ease, Barasat

Dr. Kunal Kumar Mehar
Urologist
10 Years • Mbbs, Ms, Mch
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Yogesh Taneja
Urologist
15 Years • MBBS , MS (General surgery), DNB (Genito Urinary Surgery)
Gurugram
Procyon Health, Gurugram

Dr. Pramod B R
Urologist
10 Years • MBBS, MS, MRCS, MCh
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru
(50+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
What’s the difference between BPH and prostate cancer symptoms?
Both can cause urinary problems. BPH is a benign enlargement; early prostate cancer may have no symptoms. PSA, DRE, and imaging help differentiate.
Can prostatitis cause a high PSA?
Yes. Infection or recent ejaculation can temporarily raise PSA. Treat infection first, then consider repeating the test.
What are minimally invasive BPH options?
Rezūm and UroLift reduce obstruction with quicker recovery than surgery. Suitability depends on prostate size, anatomy, and symptom severity.
How do I reduce nighttime urination?
Taper evening fluids, reduce salt and caffeine late in the day, double-void before bed, and manage constipation.
When should I consider PSA screening?
Most men discuss PSA between 55–69; higher-risk men may consider 45–50. Frequency and follow-up should be personalised.