Guide to Category/radiation Oncology
Explore radiation oncology, its purpose, treatment process, and recent advancements to understand how it helps in managing cancer effectively.


Introduction
Hearing the word "cancer" can be overwhelming, and navigating the treatment options that follow is a daunting task. Among the most common and effective treatments is radiation therapy, a field of medicine known as radiation oncology. But what exactly is it? In simple terms, radiation oncology is the medical use of high-energy radiation to control or kill cancer cells. Think of it as a highly focused and powerful beam, like a sniper, designed to target cancer cells with precision while sparing the surrounding healthy tissue as much as possible. This guide will walk you through everything you need to know, from the basic science and different types of treatment to the step-by-step process and how to manage side effects. Our goal is to demystify this advanced therapy and empower you or your loved one with knowledge and confidence for the journey ahead.
What is Radiation Oncology? The Science of Targeted Cancer Treatment
At its core, radiation oncology is a specialised branch of medicine dedicated to treating cancer with radiation. It's not a one-person show; it involves a team of experts, including your radiation oncologist (a doctor who specialises in this field), medical physicists, dosimetrists, and radiation therapists. They all work together to create a personalised plan for you.
How Does Radiation Therapy Actually Work?
The radiation used in cancer treatment works by damaging the DNA inside cells. Cancer cells are particularly vulnerable because they divide and grow much faster than most healthy cells. When their DNA is damaged beyond repair, they lose the ability to multiply and eventually die. It's important to understand that the radiation is carefully controlled. Modern technology allows the beams to be shaped and aimed directly at the tumour from multiple angles, concentrating the dose on the cancer and minimising exposure to healthy organs. This precision is the cornerstone of modern radiation oncology.
The Multidisciplinary Team: Your Radiation Oncologist and Support Staff
Your care team is your greatest ally. Your radiation oncologist leads the team, diagnosing the cancer, determining if radiation is the right course, planning the treatment, and monitoring your progress. Radiation therapists are the professionals who operate the machines and deliver your daily treatment. Dosimetrists and medical physicists work behind the scenes, using sophisticated software to calculate the exact dose and distribution of radiation to ensure it's both effective and safe.
The Main Goals: Why Choose Radiation Oncology?
Radiation therapy is a versatile tool. Depending on the type, stage, and location of the cancer, it can be used with different goals in mind.
Curative Intent: Eradicating Cancer
For many patients, the goal of radiation treatment is to cure the cancer completely. It can be used as the primary treatment, sometimes in combination with chemotherapy (chemoradiation). This is common for cancers like prostate, head and neck, cervical, and some lung cancers. In these cases, the radiation is delivered at a high enough dose to destroy all cancer cells within the targeted area.
Palliative Care: Easing Symptoms and Improving Quality of Life
When a cure isn't possible, radiation oncology plays a crucial role in palliative care. Here, the goal is to shrink tumours that are causing pain, pressure, or other debilitating symptoms. For example, it can relieve pain from cancer that has spread to the bones, reduce bleeding, or open up a blocked airway or esophagus. This approach significantly improves a patient's quality of life.
Neoadjuvant and Adjuvant Therapy: Working with Other Treatments
Radiation often teams up with other treatments:
- Neoadjuvant: Given before surgery to shrink a large tumour, making it easier to remove.
- Adjuvant: Given after surgery to kill any remaining microscopic cancer cells that couldn't be seen or removed, reducing the risk of the cancer coming back.
Consult a Radiation Oncologist for the best advice
Types of Radiation Therapy: From External Beams to Internal Seeds
There are several ways to deliver radiation, and the choice depends on your specific situation.
External Beam Radiation Therapy (EBRT)
This is the most common type, where radiation is delivered from a machine outside the body called a linear accelerator. Techniques have become incredibly precise.
- IMRT (Intensity-Modulated Radiation Therapy): This advanced form of EBRT allows the radiation beam to be broken up into many "beamlets," and the intensity of each can be adjusted. This creates a custom-shaped dose that perfectly conforms to the tumour, even if it's wrapped around a sensitive structure like the spinal cord.
- IGRT (Image-Guided Radiation Therapy): IGRT involves taking images (like tiny CT scans) just before or during treatment. This ensures you are in the exact same position every day, accounting for subtle changes like organ movement or breathing, which enhances accuracy.
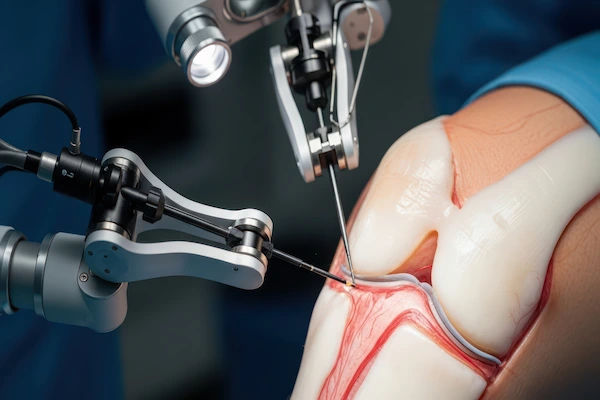
- Stereotactic Radiosurgery (SRS) and Radiotherapy (SBRT): This is a highly precise technique that delivers a very high dose of radiation in just one or a few treatments. SRS is typically for brain tumours (like Gamma Knife), while SBRT is for tumours elsewhere in the body (like lung or liver). It's so accurate it's often considered a non-surgical alternative.
Internal Radiation Therapy (Brachytherapy)
Instead of an external beam, brachytherapy places a radioactive source directly inside or very close to the tumour. Think of it as planting a seed that emits radiation from within. This allows a high dose to be given to the cancer with a rapid drop-off in dose to surrounding tissues. It's commonly used for prostate, cervical, and uterine cancers.
Systemic Radiation Therapy
Here, radioactive substances are given orally or through a vein. They travel through the bloodstream to target cancer cells. A common example is Radioactive Iodine (I-131) used to treat some types of thyroid cancer.
The Patient's Journey: A Step-by-Step Guide to Radiation Treatment
Knowing what to expect can significantly reduce anxiety. The process is methodical and patient-focused.
Step 1: Consultation and Simulation
Your journey begins with a consultation with your radiation oncologist. If radiation is recommended, the next step is a "simulation." This is a planning session where you are positioned on a CT scanner. Therapists may use special molds or masks to help you stay still. They might also make tiny tattoo dots (the size of a freckle) on your skin to ensure precise positioning for every treatment. This session is all about planning; no radiation is delivered.
Step 2: The Treatment Planning Phase
After simulation, your medical team gets to work. Using the CT scan images, your radiation oncologist, dosimetrist, and physicist design a 3D plan. They delineate the tumour and critical organs, and the computer calculates how to deliver the optimal dose. This complex process can take several days to a week.
Step 3: The Treatment Sessions Themselves
A typical course of external beam radiation treatment is outpatient and painless, much like getting an X-ray. Each session lasts about 15-30 minutes, though most of that time is spent positioning you correctly. The actual radiation delivery only takes a few minutes. You won't feel anything during the treatment, and you are not radioactive afterward. Treatments are usually given daily, Monday through Friday, for several weeks.
Managing Side Effects of Radiation Treatment
Side effects are a common concern, but it's important to know that they are usually manageable and often limited to the area being treated.
Common Side Effects and Why They Occur
Side effects occur because radiation can affect some healthy cells near the tumour. The most common is fatigue. Skin reactions (like a sunburn) are also frequent when treating areas near the skin. Other effects depend on the treatment
area: for example, radiation therapy for head and neck cancer might cause mouth sores or difficulty swallowing, while abdominal radiation could cause nausea.
Tips for Managing Fatigue, Skin Reactions, and More
- Fatigue: Listen to your body. Balance rest with light activity, like short walks. Prioritise tasks and don't hesitate to ask for help.
- Skin Care: Use mild, fragrance-free soap and lukewarm water. Gently pat the skin dry. Avoid sun exposure and wear soft, loose-fitting clothing over the treated area. Your team can recommend specific creams.
- General Wellness: Good nutrition and hydration are vital. A dietitian can help if you have eating difficulties. If
symptoms like severe skin breakdown or persistent pain occur, it's crucial to consult your doctor. For ongoing support,
you can easily consult a radiation oncologist online with Apollo24|7 to discuss management strategies.
Advanced Technologies in Modern Radiation Oncology
The field of radiation oncology is constantly evolving. Technologies like proton therapy, which uses protons instead of X-rays, offer an even greater potential to spare healthy tissue because protons can be controlled to deposit their energy directly in the tumour and then stop. Artificial intelligence is also being integrated to speed up treatment planning and enhance precision. These advancements mean treatments are becoming more effective, faster, and safer with fewer side effects, offering new hope to patients.
Conclusion
Facing cancer is a profound challenge, but understanding your treatment options can restore a sense of control. Radiation oncology represents a powerful and precise weapon in the fight against cancer, backed by decades of research and technological innovation. It's a field defined not just by its ability to target disease, but by its commitment to patient care and quality of life. Remember, you are at the center of a dedicated team of experts working tirelessly to create the best possible outcome for you. By asking questions, following your team's guidance, and caring for your well-being, you are taking active steps on your path to healing. If you have any concerns during your treatment, always communicate openly with your radiation oncologist.
Consult a Radiation Oncologist for the best advice
Consult a Radiation Oncologist for the best advice

Dr. Rupam Manna
Radiation Specialist Oncologist
7 Years • MBBS MD(RADIO THERAPY), CCEBDM
Barasat
Diab-Eat-Ease, Barasat

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr.priyank Ks Chaudhary
Radiologist
10 Years • MBBS DMRD & DNB
Lucknow
Apollo Clinic Hazratganj, Lucknow
Dr. Priya C
Radiation Specialist Oncologist
9 Years • MBBS
Bengaluru
Solasta Aesthetics, Bengaluru

Dr Devashish Tripathi
Radiation Specialist Oncologist
20 Years • MBBS, PLAB, MRCP (UK)- General Medicine, FRCR (Oncology), Certificate of Completion of Training (CCT)- Clinical Oncology
Delhi
Apollo Hospitals Indraprastha, Delhi
Consult a Radiation Oncologist for the best advice

Dr. Rupam Manna
Radiation Specialist Oncologist
7 Years • MBBS MD(RADIO THERAPY), CCEBDM
Barasat
Diab-Eat-Ease, Barasat

Dr. Sanchayan Mandal
Medical Oncologist
17 Years • MBBS, DrNB( MEDICAL ONCOLOGY), DNB (RADIOTHERAPY),ECMO. PDCR. ASCO
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata

Dr.priyank Ks Chaudhary
Radiologist
10 Years • MBBS DMRD & DNB
Lucknow
Apollo Clinic Hazratganj, Lucknow
Dr. Priya C
Radiation Specialist Oncologist
9 Years • MBBS
Bengaluru
Solasta Aesthetics, Bengaluru

Dr Devashish Tripathi
Radiation Specialist Oncologist
20 Years • MBBS, PLAB, MRCP (UK)- General Medicine, FRCR (Oncology), Certificate of Completion of Training (CCT)- Clinical Oncology
Delhi
Apollo Hospitals Indraprastha, Delhi
More articles from General Medical Consultation
Frequently Asked Questions
1. Is radiation therapy painful?
The actual treatment is painless, similar to getting an X-ray. You will not see, feel, or hear the radiation during the procedure. However, side effects that develop over the course of treatment (like skin irritation or mouth sores) can cause discomfort, which your team will help you manage.
2. How long does a typical course of radiation treatment take?
A full course of external beam radiation typically requires daily treatments (Monday to Friday) for 2 to 8 weeks, depending on the cancer type and goal of treatment. Each daily session itself lasts only about 15-30 minutes.
3. Will I be radioactive after treatment?
With standard external beam radiation, no. You are not radioactive and pose no risk to others. However, if you receive internal radiation (brachytherapy) or systemic radiation, you may be temporarily radioactive, and your medical team will provide specific safety instructions.
4. What are the long-term side effects of radiation therapy?
Most side effects are temporary. However, some long-term effects can develop months or years after treatment, depending on the area treated. These can include changes to the skin, fertility issues, or a small increased risk of developing a second cancer later in life. Your radiation oncologist will discuss these potential risks with you before treatment begins.
5. Can I work during radiation therapy?
Many people continue to work, especially if they have a flexible schedule or can work part-time. However, fatigue is a common side effect, so it's important to listen to your body and adjust your schedule as needed. Discuss your work situation with your care team for personalised advice.



 Ayurvedic Uses, Benefits, and Side Effects.webp)