Guide to Radiation Therapy Myths And Facts
Know about radiation therapy, what it is, how it works, top radiation therapy myths debunked, side effects, advanced technology and more.


Introduction
A diagnosis of cancer is life-altering, and the treatment path can feel overwhelming. When your oncologist mentions radiation therapy, it's common for a wave of fear and uncertainty to follow. Visions of glowing green sludge and debilitating sickness, often portrayed in pop culture, can cloud your judgment. This guide is designed to demystify the process, debunk the most common radiation therapy myths, and arm you with the facts. We'll walk you through what to truly expect, how technology has revolutionized the field, and how to approach your treatment with confidence and clarity.
What is Radiation Therapy, Really?
Radiation therapy (or radiotherapy) is a highly effective cancer treatment that uses focused, high-energy beams to destroy cancer cells by damaging their DNA. Contrary to the scary image of a blanket of radiation, think of it more like a skilled sniper. The goal isn't to harm your entire body but to precisely target the tumor while sparing as much healthy surrounding tissue as possible. It's one of the most common cancer treatments, used in over half of all cancer cases, either alone or in conjunction with surgery or chemotherapy.
Consult an Oncologist for Personalised Advice
How Modern Radiation Therapy Works
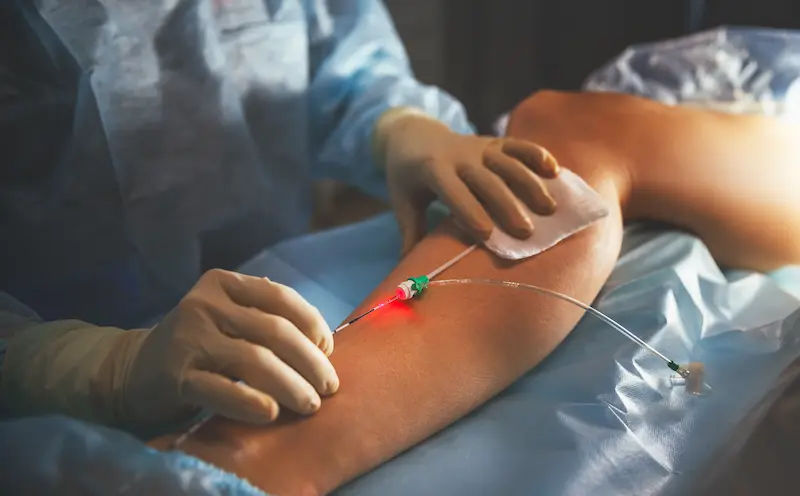
Most patients receive external beam radiation, where a machine called a linear accelerator directs the radiation beams at the tumor from outside the body. The process begins with a meticulous planning session called simulation, where you are positioned using custom molds and tiny tattoo dots are placed on your skin to ensure exact positioning for every single treatment. This level of precision is the cornerstone of modern radiation oncology.
The Goal: Precisely Targeting Cancer Cells
The fundamental principle is that cancer cells are less able to repair the DNA damage caused by radiation compared to healthy cells. While some healthy cells are affected, they have a remarkable ability to recover. Treatments are typically administered in small daily doses over several weeks (a course known as fractionation), which allows healthy cells time to heal between sessions, maximizing cancer cell kill and minimizing side effects of radiation therapy.
Top Radiation Therapy Myths Debunked
Let's tackle the biggest fears head-on and replace them with facts.
Myth 1: Radiation Therapy Will Make Me Radioactive
This is perhaps the most pervasive myth. Patients often worry they will be a danger to their family, especially children and pregnant partners.
The Fact: Understanding External Beam Radiation
With external beam radiation, the most common type, the radiation does not stay in your body. The effect is similar to getting a standard X-ray. The radiation beam passes through your body during the treatment session, and once the machine is off, no radiation remains. You are not radioactive and cannot expose others to radiation. There is no need for isolation. (A less common type, internal radiation or brachytherapy, does involve temporary radioactivity, but your medical team will provide specific safety instructions for that specific scenario).
Myth 2: Radiation Therapy Is Extremely Painful
The idea of being "zapped" by energy beams sounds inherently painful.
The Fact: The Sensation During Treatment
The treatment itself is painless. You will not see, hear, or feel the radiation beams during the session. You may hear humming or clicking from the machine as it moves around you, but you will not experience any sensation from the radiation itself. The discomfort associated with radiation therapy comes from the side effects that may develop over time, such as skin irritation or fatigue, not the actual treatment delivery.
Myth 3: Radiation Will Cause Severe Burns and Irreversible Skin Damage
The term "radiation burn" is outdated and misleading.
The Fact: Modern Techniques and Skin Care
While the skin in the treatment area can react much like a sunburn—becoming red, dry, itchy, or peeling—modern techniques like IMRT (Intensity-Modulated Radiation Therapy) allow doctors to control and shape the radiation dose with millimeter precision, dramatically reducing skin exposure. Furthermore, your care team will provide specific skin care during radiation protocols (e.g., using recommended moisturizers, avoiding sun exposure) to manage this reaction. For the vast majority, these skin changes are temporary and heal completely after treatment ends.
Myth 4: Radiation Therapy Always Causes Nausea and Hair Loss
Many assume that all cancer treatment has uniform, whole-body side effects.
The Fact: Site-Specific Side Effects
This is a critical point: side effects are almost entirely localized to the area being treated. Nausea and vomiting are only common if the treatment area is near the stomach or abdomen. Similarly, hair loss only occurs in the specific area where the radiation beam enters and exits. For example, radiation to the head will cause scalp hair loss, but radiation to the prostate or breast will not. This site-specific nature is a key advantage and differentiator from chemotherapy, which is a systemic treatment.
Myth 5: Radiation Causes Other Cancers Later
The irony of using radiation to treat cancer only to cause another one is a deep-seated fear for many.
The Fact: Weighing the Risks and Benefits
While there is a very small long-term risk of developing a secondary cancer many years later due to radiation exposure, this risk is statistically low (often estimated at less than 1 in 1000) and is carefully weighed against the significant and immediate life-saving benefit of treating your primary cancer. Modern technology's precision continues to make this risk even smaller. For most patients, the benefit of controlling their current cancer far outweighs this minimal potential risk.
The Reality of Radiation Therapy Side Effects
Understanding what to expect can make the journey less daunting.
Common Short-Term Side Effects and Management
Fatigue is the most common universal side effect, often building up over the course of treatment. Site-specific effects include skin changes (as discussed), sore throat or trouble swallowing with head/neck radiation, and urinary frequency with pelvic radiation. Your radiation oncology team is an expert in managing these effects with medications, nutritional advice, and supportive care. If symptoms like difficulty swallowing or painful urination become severe, it's crucial to consult your doctor or an oncologist online with Apollo24|7 for immediate management strategies.
Long-Term Effects and Follow-Up Care
Some effects, like slight skin darkening or tissue firmness in the treated area, can be long-lasting. More significant long-term effects depend entirely on the treatment area (e.g., dry mouth after head/neck radiation). Your care doesn't end with the last treatment; you will enter a long-term follow-up plan to monitor your recovery and manage any late effects.
The Advanced Technology Behind Modern Treatment
The field has evolved astronomically from its origins.
IMRT, IGRT, and Proton Therapy: A New Era of Precision
It includes:
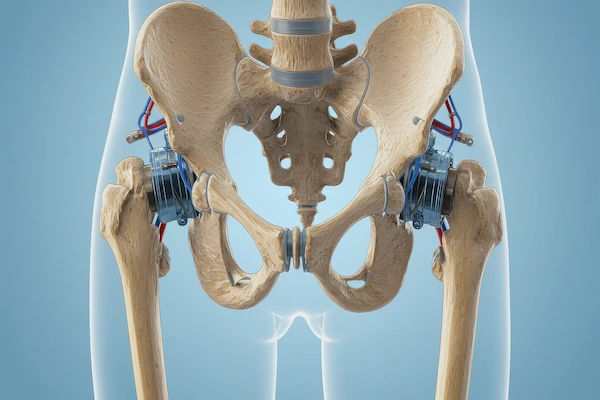
- IMRT (Intensity-Modulated Radiation Therapy) allows the radiation beam to be broken into tiny "beamlets," each with its own intensity. This allows the dose to be sculpted to the exact 3D shape of the tumor, avoiding critical organs.
- IGRT (Image-Guided Radiation Therapy) involves taking images (like a CT scan) immediately before each treatment to ensure the tumor is aligned perfectly. This accounts for day-to-day changes in organ position (like a full vs. empty bladder).
- Proton Therapy is an advanced form that uses protons instead of X-rays. Protons have a unique physical property that allows them to deposit most of their energy directly in the tumor with virtually no exit dose, further sparing healthy tissue. This is especially beneficial for cancers located near critical structures, like in the brain or spine.
Conclusion
Fear often stems from the unknown. By dismantling the myths and understanding the facts about radiation therapy, you can replace anxiety with empowerment. This treatment is a powerful, precise, and well-tolerated weapon in the fight against cancer. Your medical team is dedicated to your well-being every step of the way, from precise planning to managing side effects. Armed with accurate information, you can approach your radiation therapy not as a frightening ordeal, but as a targeted, effective step on your path to healing.
Consult an Oncologist for Personalised Advice
Consult an Oncologist for Personalised Advice

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Praveen Kumar Garg
Surgical Oncologist
26 Years • MBBS, M.S.(Gen.Surg.), M.Ch.(OncoSurg.)
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr. Ruquaya Ahmad Mir
Surgical Oncologist
20 Years • MBBS, DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Gopal Kumar
Head, Neck and Thyroid Cancer Surgeon
15 Years • MBBS, MS , FARHNS ( Seoul, South Korea ), FGOLF ( MSKCC, New York )
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Raja T
Oncologist
20 Years • MBBS; MD; DM
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)
Consult an Oncologist for Personalised Advice

Dr Gowshikk Rajkumar
Oncologist
10 Years • MBBS, DMRT, DNB in Radiation oncology
Bengaluru
Apollo Clinic, JP nagar, Bengaluru

Dr. Praveen Kumar Garg
Surgical Oncologist
26 Years • MBBS, M.S.(Gen.Surg.), M.Ch.(OncoSurg.)
Delhi
Apollo Hospitals Indraprastha, Delhi
(50+ Patients)

Dr. Ruquaya Ahmad Mir
Surgical Oncologist
20 Years • MBBS, DNB
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Gopal Kumar
Head, Neck and Thyroid Cancer Surgeon
15 Years • MBBS, MS , FARHNS ( Seoul, South Korea ), FGOLF ( MSKCC, New York )
Delhi
Apollo Hospitals Indraprastha, Delhi
(25+ Patients)

Dr. Raja T
Oncologist
20 Years • MBBS; MD; DM
Chennai
Apollo Hospitals Greams Road, Chennai
(200+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
1. How long does a typical radiation therapy session last?
Each session is very quick. While you may be in the room for 15-30 minutes for precise positioning, the actual time the machine is delivering radiation is typically only 1 to 5 minutes.
2. Can I work during radiation treatment?
Many people continue to work full-time, especially if their side effects of radiation therapy are manageable. Others scale back their hours or take leave, largely due to fatigue. It depends on your individual reaction and the physical demands of your job.
3. Will radiation therapy affect my fertility?
Radiation to the pelvic area can affect fertility in both men and women. It is absolutely crucial to discuss fertility preservation options (like sperm banking or egg freezing) with your oncologist before starting treatment.
4. What should I avoid during radiation treatment?
Your team will provide specific instructions. Generally, you should avoid sun exposure on the treatment area, avoid using hot or cold packs on the skin, and use only approved lotions and soaps. Tight, rough clothing over the area is also often discouraged.
5. Is it safe to be around pets during radiation therapy?
Yes, it is perfectly safe. Since you are not radioactive with external beam radiation, you cannot harm your pets or be harmed by them. In fact, the companionship of a pet can be a great source of comfort during treatment.