What Leads To Signs Of Ringworm And Types
Discover the causes of ringworm, identify common signs like the circular rash, and learn about the different types of fungal infections (tinea) that affect skin, scalp, and nails.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026
Introduction
If you’ve spotted an itchy, ring-shaped rash on your skin or scalp, you might be wondering if it’s ringworm—despite the name, there’s no worm involved. Ringworm is a common fungal infection that can affect nearly any part of the body, and it spreads easily through people, pets, and shared items. The good news: with the right information and timely treatment, most cases clear up quickly. In this guide for the general public, we break down what leads to signs of ringworm and the different types you should know, from athlete’s foot and jock itch to scalp infections in children. You’ll learn how ringworm spreads, how to recognize it, what treatments work, and when to see a doctor. We also include practical prevention tips, pet-related guidance, and unique insights clinicians wish more people knew. If symptoms persist beyond two weeks or keep coming back, consult a doctor online with Apollo 24|7 for further evaluation. Let’s demystify ringworm so you can take confident next steps.
What Is a Ringworm? The Basics You Need to Know
Myth-busting the name:
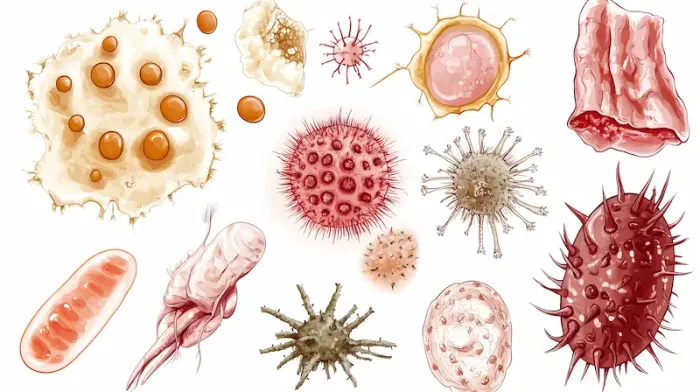
Ringworm is not caused by worms. It’s a superficial fungal infection (dermatophytosis) that affects the skin, scalp, hair, or nails. The most common culprits belong to dermatophytes such as Trichophyton, Microsporum, and Epidermophyton species .
Why the “ring”: On skin, ringworm often creates a round or oval patch with a raised, scaly border and clearer center. The edge may itch, burn, or feel tender.
Common names you’ll hear:
• Tinea corporis (body)
• Tinea capitis (scalp)
• Tinea pedis (athlete’s foot)
• Tinea cruris (jock itch)
• Tinea manuum (hand)
• Tinea faciei (face)
• Tinea barbae (beard area)
• Tinea unguium/onychomycosis (nails)
How common:
Ringworm is among the most frequent skin infections worldwide, affecting children, athletes, and anyone in warm, humid environments. It is also common in households with kittens or puppies due to Microsporum canis transmission.
Unique insight:
Many people treat only the center of the patch. Because the fungus lives at the active border, applying antifungal cream slightly beyond the visible edge helps ensure complete coverage and better results.
Names and myths to know
• “Ringworm” = “tinea” + body site. No parasitic worms are involved.
• Tinea versicolor is a different yeast infection (Malassezia), not ringworm, and is treated differently.
How ringworm looks and feels?
• Itchy, red, scaly rings on the body; on the scalp, scaling and hair loss patches; on the feet, scaling between toes or on soles; in the groin, red-brown rash with sharp border.Consult a Top General Physician
What Causes Ringworm and How Does Infection Start?
The fungi:
Dermatophytes digest keratin, the protein in skin, hair, and nails. Trichophyton rubrum and Trichophyton interdigitale commonly cause skin and foot infections; Microsporum canis is often linked to pets; Trichophyton tonsurans commonly cause scalp ringworm in children.
Entry points:
Tiny breaks in the skin, maceration from sweat, and prolonged moisture under clothing or footwear help spores establish infection. Warm, humid climates further encourage growth.
Incubation: After exposure, signs of ringworm typically appear in 4–14 days for skin, and up to a couple of weeks for scalp infections.
Unique insight:
Fungi can “hibernate” in items like brushes and hats. Even if skin looks clear, reusing contaminated items can cause quick reinfection unless they’re cleaned or replaced.
Common risk factors
• Close skin-to-skin contact (sports like wrestling)
• Sharing towels, clothing, brushes, or athletic gear
• Occlusive footwear, sweaty environments
• Minor skin trauma (shaving, scratching)
• Pets (especially kittens/puppies) and farm animals
• Diabetes, obesity, immunosuppression (steroids, chemotherapy)
Typical dermatophyte species
• Trichophyton rubrum: body, feet, nails
• Trichophyton tonsurans: scalp (human-to-human)
• Microsporum canis: pets-to-people
• Trichophyton interdigitale: interdigital feet, nails
• Trichophyton verrucosum: cattle-associated
Types of Ringworm by Body Site (Tinea Patterns)
• Tinea corporis (body): Round, expanding, scaly patches with raised borders; may itch or sting. Seen on torso, arms, or legs.
• Tinea capitis (scalp): Common in school-aged children. Creates scaly patches with hair breakage and hair loss; may cause tender, boggy inflammation called a kerion (can scar if untreated).
• Tinea pedis (athlete’s foot): Itchy scaling in toe webs, dry scaling on soles (“moccasin” type), or vesicles on the arch; can crack and invite bacteria.
• Tinea cruris (jock itch): Red-brown rash with a well-defined edge in the inner thighs and groin; often spares the scrotum; commonly spreads from athlete’s foot via towels or clothing.
• Tinea manuum (hands): Ringworm on the hands often accompanies an athlete's foot; one-hand dryness and scaling is a classic pattern.
• Tinea faciei (face) and tinea barbae (beard): Can mimic eczema or razor burn; tinea barbae can be deeper with pustules in hair follicles (often from animals).
• Tinea unguium (onychomycosis): Thick, discolored, brittle nails; toenails more commonly affected. Requires oral medication for cure in most adults.
Special note on scalp and nails
Tinea capitis and onychomycosis usually need prescription pills to clear because creams can’t reach hair shafts or nail beds effectively.
Signs and Symptoms to Watch For
Typical signs of ringworm:
• Round/oval scaly patch with an advancing, raised border
• Central clearing with more active, red edge on skin sites
• Itching or burning; sometimes mild pain with cracking
• On scalp: scaly patches with hair breakage; tender swelling (kerion)
• On nails: thickening, discoloration, crumbling
Time course: With proper antifungal treatment, most skin ringworm begins to improve in a few days and clears within 2–4 weeks; nails and scalp take longer
Red flags that merit prompt care
• Rapid swelling or pus (kerion)
• Spreading rash despite correct treatment
• Fever or signs of bacterial infection (honey-colored crusts, increased pain)
• Diabetes or immunosuppression with worsening rash
• Extensive body involvement or recurrent infections
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation.
How Ringworm Spreads?: People, Pets, and Places
• People-to-people: Skin-to-skin contact (sports, caregiving), sharing personal items (towels, combs, hats).
• Pets and farm animals: Kittens and puppies can carry Microsporum canis without obvious lesions. Cattle transmission (T. verrucosum) occurs via hands or equipment. Veterinary treatment and environmental cleaning are key.
• Fomites and environments: Locker rooms, communal showers, gym mats, and tight footwear create humidity that favors fungal survival. Spores can persist on surfaces and fabrics.
• Contagious period: Individuals are usually less contagious after 24–48 hours of appropriate antifungal therapy, but continue to complete the course to prevent relapse.
Unique insight: For households, simultaneous treatment of an asymptomatic athlete’s foot can prevent “ping-pong” reinfection of jock itch or body ringworm.
Practical prevention in shared spaces
• Wear flip-flops in locker rooms
• Disinfect gym equipment and mats
• Avoid sharing gear; wash practice clothing after each use
• Use breathable fabrics and rotate shoes so they fully dry
Diagnosis and Tests: Getting It Right
• Clinical diagnosis: Dermatologists can often identify ringworm by appearance and body site. Dermoscopy may reveal characteristic scaling at the border.
• KOH test: A quick office test where skin scrapings are examined under a microscope after potassium hydroxide application to reveal hyphae (fungal filaments).
• Fungal culture: Helpful for stubborn, recurrent, or scalp/nail cases to identify the species and guide therapy. Results may take 1–3 weeks.
• Wood’s lamp: Some Microsporum species fluoresce green under UV light, but many common Trichophyton species do not—so a negative result doesn’t rule out ringworm.
When to see a doctor:
If over-the-counter treatment fails after two weeks, if scalp or nails are involved, or if you have extensive or recurrent disease. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7. For suspected scalp or nail infection requiring tests (like fungal culture), ask your clinician about sample collection options. Apollo 24|7 offers a convenient home collection for several lab tests; your clinician can advise if a home sample is suitable for fungal studies.
Why testing matters?
• Confirming ringworm prevents misdiagnosis (e.g., eczema or psoriasis) and avoids steroid creams that can worsen fungal infections (tinea incognito).
Treatment Options That Work
1. Over-the-counter (OTC) topicals:
lotrimazole, miconazole, terbinafine, and tolnaftate creams or gels are effective for limited skin ringworm. Apply twice daily to the affected area and 2 cm beyond the border for 2–4 weeks, and continue 1 week after clearing to reduce relapse.
2. Prescription topicals:
Stronger azoles or allylamines may be used for persistent cases or certain sites (e.g., groin).
3. Oral antifungals:
Needed for most scalp and nail infections, widespread tinea corporis, or tinea barbae. Common choices include terbinafine, itraconazole, fluconazole, or griseofulvin (especially for tinea capitis in children).
Treatment duration varies:
• Scalp: typically 6–8 weeks
• Nails: 6–12 weeks for fingernails; 12+ weeks for toenails
Symptom relief:
Cool compresses, anti-itch lotions (non-steroidal), and keeping the area dry can help. Avoid strong topical steroids alone—they can mask ringworm and worsen spread (tinea incognito).
Unique insight:
If an athlete's foot is present, treat it simultaneously to prevent recurrent jock itch or body ringworm. Replace or disinfect old footwear and insoles to reduce reinfection.
Special situations
• Children:
Scalp ringworm usually requires oral medication plus medicated shampoo (e.g., selenium sulfide or ketoconazole) to reduce shedding spores during the first two weeks.
• Pregnancy:
Many topical antifungals are considered low risk; oral antifungals are generally avoided unless clearly needed—speak with your clinician.
• Diabetes or immunosuppression:
Seek medical advice early; infections may be more extensive or stubborn.
Home Care and Prevention: What Actually Helps?
Hygiene habits:
• Keep affected skin clean and dry; change sweaty clothes promptly.
• Use separate towels for body and feet; wash towels and clothing in hot water and dry on high heat.
• Don’t share personal items (towels, hats, razors, brushes).
Footwear and clothing:
• Choose breathable fabrics and moisture-wicking socks.
• Rotate shoes; use antifungal powders for sweaty feet.
• For an athlete's foot, shower sandals in communal areas.
Environmental cleaning:
• Disinfect frequently touched surfaces and gym equipment.
• For pet-associated ringworm, vacuum frequently and clean with appropriate disinfectants; ask your vet about environmental decontamination for Microsporum canis.
Unique insight:
Mark the edge of the rash with a washable skin-safe marker before treatment. If the border keeps expanding after 7 days of correct therapy, that’s a clue you need medical review.
Household and pet considerations
Have pets examined by a veterinarian if anyone in the household has recurrent ringworm—especially kittens and puppies. Treating pets and humans in parallel reduces reinfection.
Complications and Conditions That Mimic Ringworm
Complications:
• Kerion (inflammatory scalp mass) that can scar without prompt treatment
• Secondary bacterial infection (pain, pus, fever)
• Nail deformity or persistent discoloration
Look-alikes:
• Nummular eczema, psoriasis, pityriasis rosea, granuloma annulare, contact dermatitis, impetigo, and tinea versicolor (not true ringworm). When in doubt, a KOH exam or culture can clarify.
Unique insight:
Steroid creams may quickly reduce redness and itching, but can also drive the fungus deeper and alter appearance—leading to larger, more stubborn infections (tinea incognito). If a “mysterious rash” gets better on steroids, then rebounds or spreads, ask about fungal testing.
Ringworm in Children, Athletes, and High-Risk Groups
Children:
• Scalp ringworm is common. Kids can often return to school/daycare after starting appropriate treatment, typically after 24–48 hours, per local guidelines.
• Use antifungal shampoo adjuncts in the early weeks to reduce spread.
Athletes:
• Wrestlers are prone to tinea gladiatorum from close contact and shared mats. Regular skin checks, prompt treatment, and mat disinfection reduce outbreaks.
• Return-to-play policies often require 72 hours of therapy for skin ringworm and covering lesions; follow team or federation guidelines.
High-risk groups:
• People with diabetes, obesity, or weakened immunity may have more extensive or recurrent ringworm and benefit from early medical care.
• If your condition is not improving or you’re unsure about return-to-school or return-to-play timing, consult a doctor online with Apollo 24|7.
Consult a Top General Physician
Conclusion
Ringworm is common, contagious, and very treatable. Understanding what leads to the signs of ringworm—the fungi that feed on keratin, the conditions that help them thrive, and the everyday ways they spread—empowers you to spot it early and act fast. For many skin infections, consistent use of over-the-counter antifungal creams clears the rash within 2–4 weeks. For scalp and nail involvement, or when infections are widespread or recurrent, prescription therapy is often needed to fully eradicate the fungus. Keep in mind that treating an athlete's foot, cleaning shared items, and addressing pets when relevant can prevent the frustrating cycle of reinfection. If symptoms persist beyond two weeks, worsen, or you’re unsure about the diagnosis, consult a doctor online with Apollo 24|7 for personalized advice and treatment. With the right plan, most people can get back to clear, comfortable skin—and keep it that way.
Consult a Top General Physician

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Swagato Podder
General Practitioner
5 Years • MBBS
Kolkata
GRD POLYCLINIC, Kolkata

Dr. Moumita Roy
General Physician/ Internal Medicine Specialist
8 Years • MBBS , MD (Anesthesiology)
Kolkata
VDC Clinic, Kolkata

Dr. Arif Ahmed
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Genl. Med.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
Consult a Top General Physician

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Chethan T L
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD, DNB (General Medicine)
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr. Swagato Podder
General Practitioner
5 Years • MBBS
Kolkata
GRD POLYCLINIC, Kolkata

Dr. Moumita Roy
General Physician/ Internal Medicine Specialist
8 Years • MBBS , MD (Anesthesiology)
Kolkata
VDC Clinic, Kolkata

Dr. Arif Ahmed
General Physician/ Internal Medicine Specialist
9 Years • MBBS, MD (Genl. Med.)
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
More articles from General Medical Consultation
Frequently Asked Questions
Introduction If you’ve spotted an itchy, ring-shaped rash on your skin or scalp, you might be wondering if it’s ringworm—despite the name, there’s no worm involved. Ringworm is a common fungal infection that can affect nearly any part of the body, and it
Ringworm can spread until effective treatment is started. People are usually less contagious after 24–48 hours of appropriate antifungal therapy, but you should complete the full course to prevent relapse and ongoing transmission. This applies to skin ringworm and tinea capitis in children.
What’s the best treatment for ringworm on the body?
For limited tinea corporis, over-the-counter creams like clotrimazole or terbinafine applied twice daily for 2–4 weeks are effective. Apply 2 cm beyond the rash border and continue for a week after the rash clears to reduce recurrence. If there’s no improvement in 2 weeks, consult a doctor online with Apollo 24|7.
Can I get ringworm from my cat or dog?
Yes. Kittens and puppies often carry Microsporum canis and can transmit it to humans. If you suspect a pet-related ringworm, have your animal examined and treated by a veterinarian, and clean the home environment to reduce spores.
How do I tell ringworm from eczema or psoriasis?
Ringworm tends to have a ring shape with a more active, scaly edge and central clearing. Eczema and psoriasis usually lack a sharply advancing ring. A quick KOH test can confirm ringworm. If your rash worsens with steroid-only creams, ask about fungal testing.
What if my ringworm keeps coming back?
Persistent ringworm may signal untreated athlete’s foot, contaminated items (shoes, hats, brushes), or pet transmission. Treat all affected areas simultaneously, disinfect or replace fomites, and consider medical review for a KOH/culture. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7.
.webp)



