Understanding Dilated Cardiomyopathy: Causes, Symptoms, and Treatment
Dilated cardiomyopathy (DCM) weakens and enlarges the heart, leading to fatigue, swelling, and breathlessness. Learn its causes, symptoms, diagnosis, and advanced treatments—from medications to devices—that can improve quality of life and outcomes.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
Your heart, the tireless engine of your body, can sometimes weaken and enlarge, a condition known as dilated cardiomyopathy (DCM). This common form of cardiomyopathy affects millions worldwide, diminishing the heart's ability to pump blood effectively and leading to symptoms like breathlessness, fatigue, and swelling. But what causes this crucial muscle to falter? More importantly, is there a cure? This article demystifies DCM, exploring its root causes—from genetics and infections to lifestyle factors—and detailing the modern, effective treatment strategies that can manage the condition, dramatically improve quality of life, and even reverse some damage. Whether you're seeking answers for yourself or a loved one, understanding DCM is the first step toward taking control of your heart health.
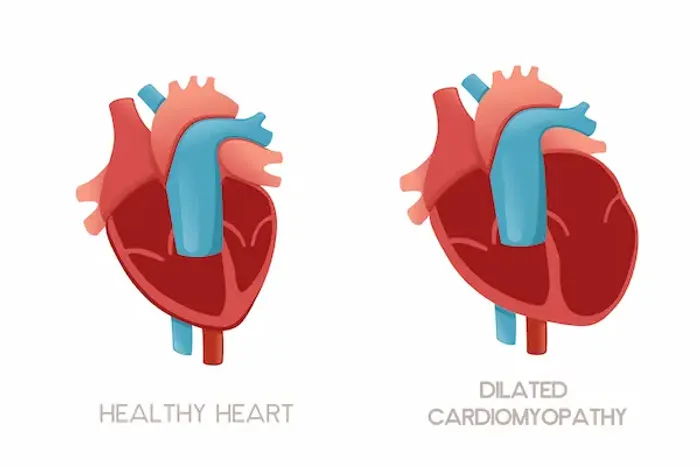
What is Dilated Cardiomyopathy (DCM)?
Dilated cardiomyopathy (DCM) is a disease of the heart muscle where the main pumping chamber, the left ventricle, becomes enlarged (dilated) and weak. This weakening means it can't contract effectively, leading to a reduced ejection fraction—the percentage of blood pumped out with each heartbeat. A normal ejection fraction is between 55% and 70%; in DCM, it often falls below 40%. As the heart's pumping power declines, it struggles to supply the body with enough oxygen-rich blood, a condition known as heart failure. It's the most common type of cardiomyopathy and a leading reason for heart transplants.
How DCM Affects Your Heart's Function
Think of a healthy heart ventricle as a strong, elastic balloon that squeezes powerfully. In DCM, the balloon becomes stretched out, thin, and flabby. It fills with more blood but can only push a fraction of it out to the body. The heart compensates by beating faster and holding onto salt and water, which initially helps but eventually leads to fluid buildup in the lungs, legs, and abdomen, causing the classic symptoms of heart failure.
What Causes Dilated Cardiomyopathy? The Known Triggers
In many cases, the exact cause remains unknown (idiopathic DCM). However, decades of research have identified several key triggers that can lead to this enlarged heart condition.
Genetic and Inherited Factors
In about 20-35% of cases, DCM runs in families. Specific genetic mutations can affect the proteins that make up the heart muscle, making it prone to dilation and weakness. If a first-degree relative has DCM, other family members are often advised to undergo screening.
Previous Heart Damage (Ischemic Cardiomyopathy)
The most common identifiable cause is damage from a heart attack or severe coronary artery disease. When arteries are blocked, heart muscle cells die from lack of oxygen, forming scar tissue. This scarred area doesn't pump, forcing the remaining healthy muscle to work harder, which can lead to dilation over time.
Infections and Myocarditis
Viral infections (like COVID-19, Coxsackievirus, or influenza) can sometimes trigger myocarditis—inflammation of the heart muscle. This inflammation can damage the muscle cells, leading to DCM. In some cases, the heart recovers fully; in others, the damage is permanent.
Toxins and Lifestyle Factors
Prolonged, heavy alcohol abuse is a major culprit, as ethanol is directly toxic to heart muscle cells. Certain chemotherapy drugs (e.g., doxorubicin) and illicit drugs like cocaine and amphetamines can also cause irreversible damage leading to DCM.
Other Medical Conditions and Pregnancy-Related Causes
Uncontrolled high blood pressure, thyroid disorders, diabetes, and sleep apnea can all place chronic strain on the heart. Additionally, a rare condition called peripartum cardiomyopathy can develop in the last month of pregnancy or after delivery, though the reasons are not fully understood.
Recognizing the Signs: Symptoms of DCM
The symptoms of DCM are primarily those of heart failure and often develop gradually. They include:
- Shortness of breath (dyspnea): Especially during activity or when lying flat.
- Fatigue and weakness: Due to reduced blood flow to muscles and organs.
- Swelling (edema): In the legs, ankles, feet, and abdomen from fluid retention.
- Weight gain: Rapid gain from fluid buildup.
- Heart palpitations: A fluttering or pounding sensation in the chest caused by arrhythmias.
- Dizziness or fainting: From irregular heart rhythms or low blood pressure.
- It's crucial not to ignore these signs. If you experience persistent shortness of breath or unexplained swelling, consulting a doctor online with Apollo24|7 for further evaluation is a critical first step.
How is Dilated Cardiomyopathy Diagnosed?
Diagnosis involves a multi-step process to confirm DCM, assess its severity, and try to identify the cause.
Initial Consultation and Physical Exam
A doctor will discuss your symptoms, medical history, and family history. During the physical exam, they will listen for lung crackles (fluid), a heart murmur, and check for signs of fluid retention.
Key Diagnostic Tests
- Echocardiogram: The Primary Tool: This ultrasound of the heart is the gold standard for diagnosing DCM. It provides a moving image, allowing doctors to see the enlarged chambers, measure the ejection fraction, and check valve function.
- ECG, Blood Tests, and Advanced Imaging: An electrocardiogram (ECG) detects abnormal heart rhythms and damage. Blood tests, including BNP (a hormone that rises in heart failure), can support the diagnosis. Apollo24|7 offers convenient home collection for these crucial blood tests. Cardiac MRI or CT scans provide even more detailed images of heart structure and tissue characteristics.
Is There a Cure? The Goals of DCM Treatment
While there is no outright cure that makes DCM disappear completely, modern treatment is highly effective at managing the condition, relieving symptoms, stopping progression, and in some cases, reversing the damage. The goals are to improve heart function, manage symptoms, and prevent sudden cardiac death.
Lifestyle Modifications: The Foundation of Management
This is non-negotiable. It includes a low-sodium diet to reduce fluid retention, fluid restriction, regular physical activity (as tolerated), complete avoidance of alcohol and tobacco, and weight management.
Core Medications for DCM
A combination of drugs is typically used:
- ACE inhibitors or ARBs/ARNIs: Relax blood vessels, making it easier for the heart to pump.
- Beta-blockers: Slow the heart rate, reduce blood pressure, and protect the heart from stress hormones.
- SGLT2 Inhibitors: A newer class of drugs proven to reduce hospitalization and death in heart failure.
- Diuretics ("water pills"): Help the kidneys remove excess fluid, relieving swelling and breathlessness.
- Mineralocorticoid receptor antagonists: Help reduce scarring and further remodeling of the heart.
Implantable Devices: ICDs and CRT
An Implantable Cardioverter-Defibrillator (ICD) is a small device placed in the chest to detect and stop life-threatening arrhythmias, a key method for sudden cardiac death prevention. Cardiac Resynchronization Therapy (CRT) uses a special pacemaker to help the heart's chambers beat in sync, improving efficiency.
Advanced Surgical Procedures
For advanced cases, a left ventricular assist device (LVAD)—a mechanical pump that helps the heart pump blood—can be a long-term solution or a bridge to a transplant. A heart transplant is considered when all other treatments have failed.
The Future of DCM Treatment: Ongoing Research
Research is focused on gene therapies to correct inherited mutations, stem cell treatments to regenerate damaged heart tissue, and more targeted medications. The future of cardiomyopathy management is moving towards highly personalized medicine based on an individual's genetic and molecular profile.
Living with Dilated Cardiomyopathy: Prognosis and Quality of Life
The prognosis for DCM has improved dramatically over the last 20 years thanks to modern medications and devices. Many people live long, active lives with well-managed DCM. Adherence to treatment and lifestyle changes is the single biggest factor in determining dilated cardiomyopathy life expectancy and quality of life. Regular follow-up with a cardiologist is essential.
Conclusion
The journey through understanding dilated cardiomyopathy reveals a condition rooted in various causes—from our genes to our lifestyle choices. While the word "cure" might imply a finality we don't yet have, the reality is far more hopeful. Today's treatment arsenal offers powerful tools to not just manage but significantly improve heart function, allowing individuals to reclaim their vitality. The path forward involves partnership: between you and your healthcare team, between medication and lifestyle, and between vigilance and hope. By taking proactive steps, seeking expert care, and adhering to your prescribed plan, you can powerfully influence your heart's health and your overall well-being. Don't wait for symptoms to worsen; take control of your heart health today.
Consult a Specialist for the best advice

Dr Syed Mateen Pasha
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Vivek D
General Physician
4 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Harshendra Jaiswal
General Physician/ Internal Medicine Specialist
12 Years • MBBS , MD (General medicine)
Kolkata
108 DHANA DHANVANTARI Clinic, Kolkata
(25+ Patients)

Dr. Syed Ismail Ali
General Practitioner
7 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Dhanraj K
General Physician/ Internal Medicine Specialist
25 Years • MBBS, MD Internal Medicine - Osmania Medical College, Hyderabad
Hyderabad
Apollo Hospitals Jubilee Hills, Hyderabad
(425+ Patients)
More articles from General Medical Consultation
Frequently Asked Questions
Can dilated cardiomyopathy be reversed?
In some cases, yes. If the cause is addressed early (e.g., stopping alcohol consumption, treating myocarditis, or with aggressive medication therapy), the heart muscle can recover some strength and reduce in size, a process called reverse remodeling.
What is the difference between ischemic and non-ischemic cardiomyopathy?
Ischemic cardiomyopathy is caused by blockages in the heart's arteries (like from a heart attack). Non-ischemic cardiomyopathy includes all other causes, such as genetic, viral, alcoholic, or hypertensive causes. DCM can be either type.
Is dilated cardiomyopathy a death sentence?
Absolutely not. While it is a serious condition, it is not an immediate death sentence. With modern treatment, many people manage their condition effectively for decades, maintaining a good quality of life.
Can you exercise with dilated cardiomyopathy?
Yes, but it must be done carefully and under the guidance of your doctor. Regular, moderate exercise is often encouraged as it strengthens the body and improves cardiovascular efficiency. Strenuous activity may be restricted.
What foods should be avoided with cardiomyopathy?
The most important dietary change is to drastically reduce sodium (salt) intake, as it causes fluid retention. Processed foods, canned soups, fast food, and salty snacks are major sources. Limiting fluids and avoiding alcohol are also critical.




