Vasectomy Myths Debunked: Separating Fact from Fiction
Considering a vasectomy? Don't let misinformation stand in your way. We debunk common myths about vasectomy pain, permanence, sexual function, and the link to cancer.

Written by Dr. Dhankecha Mayank Dineshbhai
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026

Introduction
The decision to undergo a vasectomy is a significant one, often made after careful consideration with a partner. Yet, for many men, this rational choice is clouded by a fog of misinformation, old wives' tales, and outright myths. These misconceptions, often perpetuated by pop culture and a general reluctance to discuss male reproductive health openly, can create unnecessary fear and anxiety. It's time to set the record straight. This guide will cut through the noise and debunk the most common vasectomy myths with clear, evidence-based facts. We'll explore everything from its impact on your sex life to the realities of the procedure and recovery, empowering you to make a confident, informed decision about your health and future. Understanding the truth is the first step toward taking control of your reproductive choices.
What is a Vasectomy? A Quick Overview
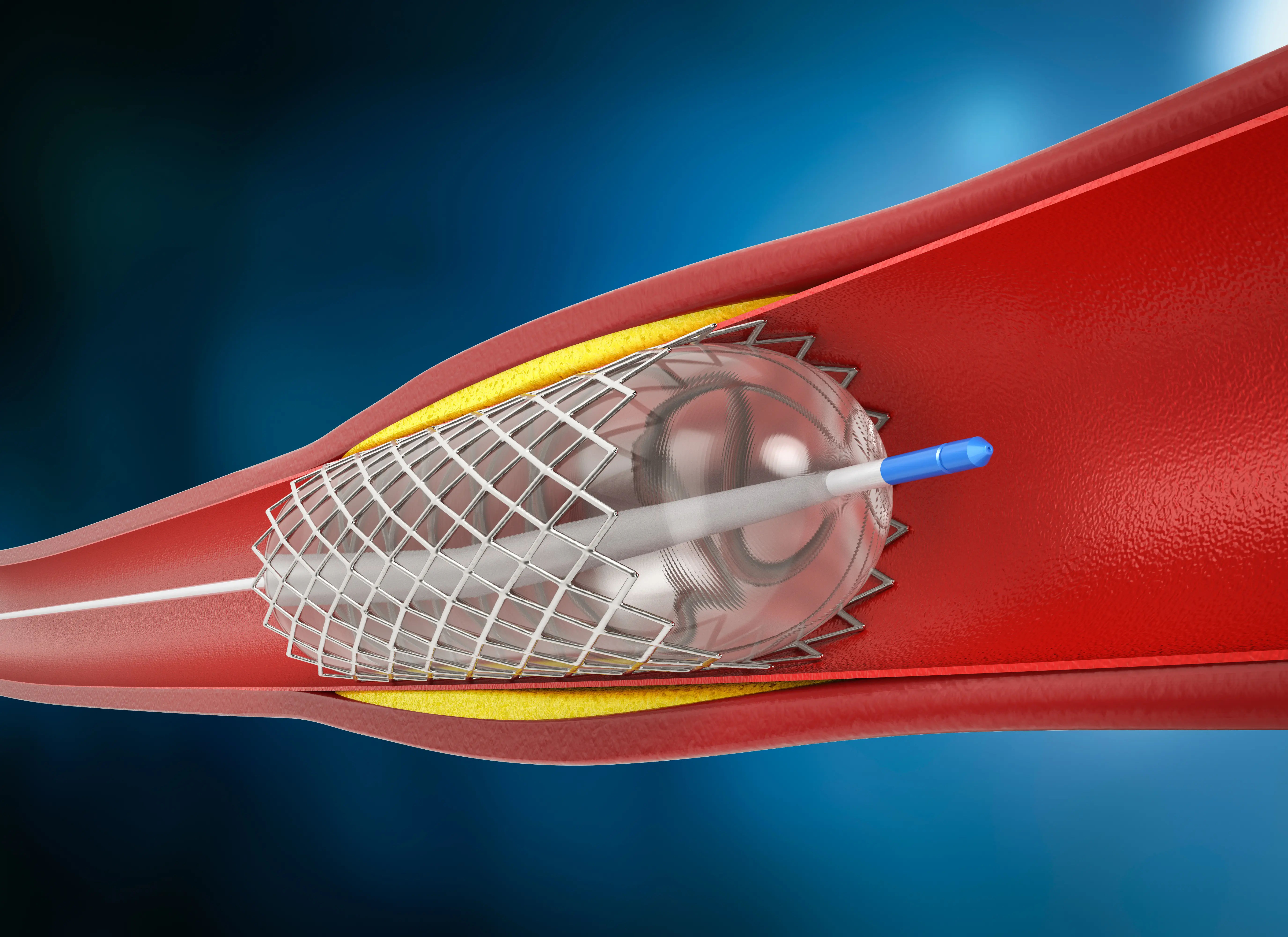
A vasectomy is a simple surgical procedure for male sterilization. Its goal is to prevent pregnancy by interrupting the pathway sperm take to get into semen. During the procedure, the vas deferens—the two tubes that carry sperm from the testicles to the urethra—are cut, sealed, or clipped. This prevents sperm from mixing with seminal fluid during ejaculation. It's crucial to understand that a vasectomy does not remove the testicles, and it only blocks the transport of sperm; it does not stop the production of sperm or hormones.
The No-Scalpel Vasectomy Technique
The modern standard is the no-scalpel vasectomy, a minimally invasive technique. Instead of a traditional scalpel, the urologist uses a special instrument to make a tiny puncture in the skin. This approach typically results in less bleeding, a lower risk of infection, and a faster recovery compared to the conventional method. The entire procedure is usually completed in about 15-20 minutes under local anesthesia.
Consult Top Specialists
Myth 1: A Vasectomy Affects Your Sex Drive and Performance
The Myth: Perhaps the most pervasive fear is that a vasectomy will diminish your libido, impair your ability to get an erection, or otherwise negatively impact your sexual performance.
The Fact: This is completely false. A vasectomy does not affect your sex drive or sexual function.
The Science Behind Libido and Testosterone
Your sex drive (libido) and erectile function are primarily governed by hormones, specifically testosterone, which is produced in the testicles. A vasectomy does not involve the testicles themselves or their blood supply; it only interrupts the vas deferens. Your body continues to produce testosterone at the same levels as before. Sperm cells that are no longer transported are simply reabsorbed by the body, a natural and harmless process.
Psychological Benefits: Less Anxiety, More Enjoyment
In fact, many men report an improvement in their sex life post-vasectomy. The elimination of anxiety about unplanned pregnancy can lead to a more relaxed, spontaneous, and enjoyable sexual experience for both partners. The pressure associated with other forms of birth control is removed, allowing couples to focus on intimacy.
Myth 2: You'll Become Less of a Man
The Myth: This myth ties masculinity directly to fertility, suggesting that an infertile man is somehow less virile or manly.
The Fact: A vasectomy does not change who you are. It does not alter your hormone levels, your voice, your body hair, your muscle mass, or any other physical characteristic associated with masculinity.
Defining Masculinity Beyond Fertility
Masculinity is a complex blend of identity, behavior, and social expectations that extends far beyond the biological ability to father children. Traits like integrity, responsibility, strength, and providing for one's family are pillars of masculinity that are entirely unaffected by a vasectomy. Choosing a vasectomy is often a responsible decision made by a man to care for his family's future and his partner's well-being.
What Actually Controls Male Characteristics?
Your male characteristics are controlled by testosterone produced in the Leydig cells of your testicles. Since a vasectomy doesn't touch these cells or their blood supply, your hormonal profile remains unchanged. You will not experience menopause or any kind of hormonal shift.
Myth 3: A Vasectomy is 100% Effective Immediately
The Myth: You are sterile immediately after the procedure.
The Fact: This is dangerously incorrect. It takes time and follow-up testing to achieve sterility.
The Crucial Role of Post-Vasectomy Semen Analysis
After the vasectomy, there is still sperm stored in the reproductive tract beyond the blockage point. It can take several weeks and numerous ejaculations (usually 15-20) to clear out all remaining sperm. You must use another form of birth control until your doctor confirms you are sterile.
How to Confirm You're Sterile
The only way to confirm the vasectomy's effectiveness is through a post-vasectomy semen analysis (PVSA). Your urologist will schedule this test typically around 12 weeks after the procedure. The lab will analyze a sample to ensure the sperm count is zero. Only after you receive the official "all-clear" from your doctor are you considered sterile.
Myth 4: The Procedure is Extremely Painful and Risky
The Myth: A vasectomy is a horribly painful operation with a high risk of complications.
The Fact: While no surgery is entirely without discomfort or risk, a vasectomy is one of the safest and least painful surgical procedures performed today.
Modern Anesthesia and Pain Management
The procedure is done under local anesthesia, meaning you are awake but the area is completely numb. Most men report feeling only slight pressure or tugging sensations. Any post-operative pain is usually mild and manageable with over-the-counter pain relievers like ibuprofen, applying ice packs, and wearing supportive underwear for a few days.
Comparing Vasectomy Risks to Female Sterilization
The risk of major complications from a vasectomy (e.g., infection, significant bleeding, hematoma) is very low, generally under 2%. When compared to tubal ligation (female sterilization), which is a more invasive abdominal surgery requiring general anesthesia, the vasectomy is significantly safer, less expensive, and has a much easier recovery.
Myth 5: Vasectomies Cause Long-Term Health Problems
The Myth: Vasectomies lead to serious issues like prostate cancer or chronic pain.
The Fact: Extensive research has debunked the link to prostate cancer, and while chronic pain can occur, it is rare.
Debunking the Link to Prostate Cancer
Early studies suggesting a link between vasectomy and prostate cancer have been thoroughly disproven by larger, more robust research. Major health organizations, including the American Urological Association (AUA) and the World Health Organization (WHO), have concluded there is no causal relationship between vasectomy and prostate cancer.
Understanding Post-Vasectomy Pain Syndrome (PVPS)
A small percentage of men (estimated at 1-2%) may experience chronic testicular pain after a vasectomy, known as Post-Vasectomy Pain Syndrome. The cause isn't always clear, but it can often be managed with medication or further treatment. It's important to discuss this potential risk with your urologist, but understand that it is an uncommon outcome. If you experience persistent discomfort after your recovery period, consult a doctor online with Apollo24|7 for advice on next steps.
Myth 6: Vasectomy Reversal is Always Successful
The Myth: If I change my mind later, a reversal is a simple and guaranteed fix.
The Fact: Vasectomy reversal is a complex microsurgery that is not always successful and should not be relied upon.
The Realities of Vasectomy Reversal Surgery
Reversal is a much more involved procedure than the original vasectomy. Success rates, defined by the return of sperm to the semen, decrease over time. While rates can be high (up to 90-95%) within the first 10 years, they drop significantly after that. Even if sperm return, achieving a pregnancy is not guaranteed.
Why You Should Consider Vasectomy Permanent
You should only choose a vasectomy if you are certain you do not want to father more children. While reversal is an option, it is expensive, not covered by most insurance, and its success is uncertain. Sperm banking before the procedure is a recommended alternative for men who are unsure about their future fertility desires.
Myth 7: It's a Major Surgery with a Long Recovery
The Myth: You'll be bedridden for weeks and unable to work.
The Fact: Vasectomy is a minor outpatient procedure with a remarkably quick recovery.
Typical Vasectomy Recovery Timeline
- Day of Procedure: Rest with ice applied to the scrotum.
- Next 2-3 Days: Most men can return to sedentary jobs or light activities. Avoid heavy lifting and strenuous exercise.
- Within a Week: Many resume all normal activities, including exercise.
- The no-scalpel vasectomy technique further accelerates this timeline, with many men feeling fine within a day or two.
Tips for a Smooth Recovery Process
The key to an easy recovery is to follow your doctor's orders: rest for the first 24 hours, use ice packs to reduce swelling, wear a jockstrap or supportive briefs for added comfort, and avoid heavy straining for about a week. Listening to your body is paramount.
Conclusion: Making an Informed Decision
Debunking these common vasectomy myths reveals a simple truth: vasectomy is a safe, highly effective, and straightforward form of permanent birth control. The fears surrounding it are largely based on fiction, not medical science. By separating fact from fiction, you can evaluate the procedure based on its real benefits and minimal risks. The decision is a personal one that should be made through open conversation with your partner and a detailed consultation with a qualified urologist. Don't let outdated myths stand in the way of making a responsible choice for your family planning. If you have specific health concerns or questions about your suitability for the procedure, book a physical visit to a doctor with Apollo24|7 to get personalized, professional advice.
Consult Top Specialists
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Divya Lekha Gunta
General Practitioner
10 Years • MBBS, MD (Pathology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Hari Krishna
General Physician/ Internal Medicine Specialist
13 Years • MD (Gen. Med. )
Chennai
Apollo Hospitals Greams Road, Chennai
(50+ Patients)
Consult Top Specialists

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr Divya Lekha Gunta
General Practitioner
10 Years • MBBS, MD (Pathology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr D M Karthik
General Practitioner
4 Years • MBBS, Fellowship in Diabetes Mellitus, Advance certificate in Diabetes Mellitus, Derma Nutrition Certification
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Hari Krishna
General Physician/ Internal Medicine Specialist
13 Years • MD (Gen. Med. )
Chennai
Apollo Hospitals Greams Road, Chennai
(50+ Patients)