What Leads To Signs Of Leaky Gut Syndrome Diet Test Treatment
Discover what leads to signs of leaky gut syndrome, effective diet strategies, reliable tests, helpful supplements, and lifestyle habits to support gut health. Learn practical steps to manage symptoms and when to consult a doctor.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
Feeling bloated, foggy, or fatigued and wondering if it’s “leaky gut syndrome”? You’re not alone. Online searches for leaky gut have skyrocketed as more people connect digestive upset with skin issues, low energy, and even joint pain. While “leaky gut syndrome” isn’t a formal medical diagnosis, the science does recognize a real process called increased intestinal permeability—when the gut lining becomes less selective and lets more substances pass into the bloodstream. That can fuel inflammation and discomfort in some people.
In this guide, we’ll unpack what actually leads to signs often linked with leaky gut syndrome, which tests help (and which don’t), practical diet ideas, and evidence-based treatment steps. You’ll also see where the research stands, so you can filter hype from helpful advice. If symptoms persist beyond two weeks or feel severe, you should talk to a clinician. If you’re looking for convenient, expert guidance, you can consult a doctor online with Apollo 24|7 for further evaluation and a personalized plan.
Note: Throughout this article, we use “leaky gut” in quotes to reflect common language and also refer to the medical
term “increased intestinal permeability.”
What “Leaky Gut Syndrome” Really Means
Understanding what “leaky gut” really refers to helps clarify the difference between popular claims and clinical reality.
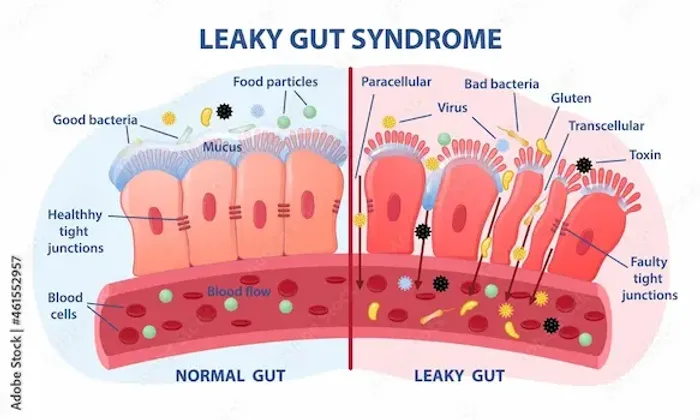
A popular term vs. a medical process
“Leaky gut syndrome” is a popular umbrella term, but in medicine we focus on the gut barrier and “intestinal
permeability.” Your gut lining is made of epithelial cells connected by tight junctions that normally control what gets
through. If those junctions loosen, larger molecules can pass into the body, potentially activating the immune system
and fueling symptoms in susceptible people.
Where research stands
- Established: Increased permeability occurs in known conditions like celiac disease, inflammatory bowel disease (IBD),
some cases of irritable bowel syndrome (IBS), and after NSAID use or alcohol intake. - Unsettled: Whether increased permeability alone causes a wide range of symptoms in otherwise healthy people is less clear. Many experts caution that while the concept is real, “leaky gut syndrome” as a stand-alone diagnosis is not standardized.
- Practical takeaway: Focus less on the label and more on identifying root causes, ruling out serious disease, and using validated steps to calm symptoms.
Unique insight: Think of the gut like a coffee filter. If the filter is torn (barrier disrupted) or the coffee grounds are very fine (dietary and microbial factors), more particles slip through—changing the “brew” your body has to handle. Improving both the filter (lining integrity) and the grounds (diet and microbiome) produces the best result.
How a Healthy Gut Barrier Works
A strong gut barrier is central to preventing immune overactivation and maintaining overall well-being.
Multiple layers of protection
- Physical barrier: Mucus layer, epithelial cells, and tight junction proteins (e.g., claudins, occludin).
- Immune barrier: Secretory IgA and antimicrobial peptides patrol the lining
- Microbial barrier: Beneficial gut microbes produce short-chain fatty acids (especially butyrate) that nourish colon cells and reinforce the barrier.
Consult Top Specialists Here
Regulators of permeability
- Diet and microbial metabolites (like butyrate) generally strengthen the barrier.
- Stress hormones, certain medications (NSAIDs), alcohol, infections, and inflammatory signals can loosen tight junctions.
- Proteins like zonulin modulate junctions, but real-world clinical testing for “zonulin” is controversial due to assay limitations.
Why it matters
A resilient barrier reduces immune overactivation. When it’s impaired, more bacterial fragments (e.g., LPS), dietary antigens, or toxins may cross into circulation, potentially exacerbating symptoms in conditions like IBS, celiac disease, or metabolic syndrome.
Unique insight: Barrier health is not binary. It fluctuates daily with sleep, stress, and meals. Small consistent choices—
fiber, fermented foods, gentle exercise—often outperform “miracle cures.”
Signs People Notice—and What They May Indicate
Recognising symptom patterns helps determine whether further evaluation is needed.
Common digestive signs of “leaky gut”
- Bloating, gas, abdominal discomfort
- Irregular bowel habits (constipation, diarrhea)
- Food triggers or sensitivity patterns
Beyond the gut (nonspecific)
- Fatigue or “brain fog”
- Headaches, skin flares (acne, eczema), joint aches
- Mood changes (anxiety, low mood)
These are real experiences, but they are nonspecific and overlap with IBS, celiac disease, thyroid disorders, iron deficiency, or even sleep deprivation. Increased permeability can accompany some of these issues, but is rarely the only driver.
When symptoms suggest a specific condition
- Frequent diarrhea, weight loss, anemia: consider celiac disease or IBD.
- Severe bloating with high-carb foods: consider SIBO or carbohydrate malabsorption.
- Nocturnal symptoms, rectal bleeding, fever: urgent evaluation for IBD/infection.
If you notice red-flag symptoms like blood in stool, persistent fever, unintentional weight loss, or symptoms disrupting sleep, book a physical visit to a doctor with Apollo 24|7 for timely assessment.
Unique insight: Track “clusters” rather than isolated symptoms—e.g., bloating + loose stools + urgency points one way; fatigue + constipation + dry skin may suggest a different workup. Clusters help your clinician choose the right test, not just a catch-all “leaky gut” label.
What Leads to Increased Intestinal Permeability
Understanding triggers can guide diet, lifestyle, and treatment choices.
Diet patterns
- Low fiber, ultra-processed foods: Associated with reduced microbiome diversity and less butyrate, which may weaken
barrier function. - Emulsifiers in processed foods: Certain emulsifiers (e.g., carboxymethylcellulose) altered the microbiome and metabolism and increased GI symptoms.
- High alcohol intake: Known to increase permeability and inflammation.
- Artificial sweeteners: Some can alter glucose tolerance via the microbiome in susceptible individuals.
Medications and infections
- NSAIDs (e.g., ibuprofen): Increase small intestinal permeability; chronic use raises risk of GI injury.
- Gastrointestinal infections: Temporarily increase permeability and can trigger post-infectious IBS in some.
Stress, sleep, and exertion
- Acute psychological stress increases small intestinal permeability in controlled studies.
- Severe sleep disruption and extreme endurance exercise can also impair barrier function.
Medical conditions
- Celiac disease, IBD, IBS (subset), nonalcoholic fatty liver disease, type 1 diabetes (subset): All show permeability changes in research.
Unique insight: Consider a “threshold model.” A single factor may not trigger symptoms, but stacking several—NSAIDs + poor sleep + alcohol + ultra-processed foods—can push you over your personal threshold. Removing just one load (e.g., switch from daily NSAIDs to alternatives) can make a noticeable difference.
Tests: What’s Valid, What’s Not, and When to Use Them
Knowing which tests are meaningful helps avoid unnecessary expense and confusion.
Tests with clearer clinical roles
- Rule-out tests guided by symptoms:
- Celiac serology (tTG-IgA with total IgA) when diarrhea, iron deficiency, or family history is present
- Stool calprotectin if inflammatory bowel disease is suspected
- Breath tests for SIBO in select cases of bloating/gas
- Basic labs (CBC, iron studies, B12, vitamin D, thyroid, CRP) to catch common contributors to fatigue and GI symptoms
Permeability-specific tests
- Lactulose–mannitol test: Measures urinary sugar excretion ratio after ingestion to estimate small intestinal permeability.
- “Zonulin” blood or stool tests: Many commercial assays are unreliable and may not measure zonulin accurately, limiting their clinical utility.
- Stool microbiome panels: Interesting but currently limited in actionability for most individuals; results should be interpreted with caution.
Tests to avoid or be cautious with
- IgG food “sensitivity” panels: Not recommended by major allergy/immunology groups; IgG often reflects exposure, not intolerance or allergy.
How to decide on testing
- Start with history and red flags to prioritize rule-out testing.
- Consider a time-boxed diet/lifestyle trial (4–8 weeks). If symptoms persist, consult a doctor online with Apollo 24|7 to tailor further tests.
Unique insight: Testing is most powerful when it changes your next decision. Before any test, ask: “What will I do differently based on a positive or negative result?” If the answer is “nothing,” reconsider the test.
Diet Strategies That Support the Gut Lining
A gut-friendly diet forms the foundation of barrier support and symptom management.
Foundations first
- Fiber-rich plants: Aim for 25–35 g/day from vegetables, fruits, legumes, whole grains, nuts, and seeds.
- Fermented foods: Yogurt, kefir, kimchi, sauerkraut, tempeh.
- Mediterranean-style eating: Emphasizes plants, olive oil, fish, and minimally processed foods.
Strategic eliminations (time-limited)
- Low-FODMAP diet: Can reduce bloating and IBS symptoms; best done with a dietitian and followed by structured reintroduction.
- Gluten trial: If celiac disease is ruled out, a 2–4 week gluten reduction may help some with IBS-like symptoms.
Foods to consider reducing
- Ultra-processed foods with emulsifiers and artificial sweeteners if you notice sensitivity.
- Alcohol to low/moderate intake; avoid binge patterns.
“Gut-soothing” additions
- Omega-3–rich foods (fatty fish, walnuts), berries, extra-virgin olive oil, and green tea.
- Bone broth and collagen can be included, though evidence for rapid gut healing is limited.
Example day (leaky gut syndrome diet plan)
- Breakfast: Plain yogurt or kefir with oats, chia, blueberries, and walnuts.
- Lunch: Lentil and vegetable soup, olive-oil-dressed salad, whole-grain toast.
- Snack: Banana with peanut butter; green tea.
- Dinner: Grilled salmon, quinoa, roasted broccoli and carrots; sauerkraut on the side.
Unique insight: Aim for 30 different plant foods per week. Variety fosters microbiome diversity, which supports the barrier. If that feels daunting, add two new plants per week rather than eliminating five foods at once.
Helpful Supplements (and Ones to Skip)
Supplements can be useful when paired with diet and lifestyle changes.
Supplements with some supportive evidence
- Probiotics: Certain strains (e.g., Lactobacillus rhamnosus GG, Bifidobacterium longum) may reduce IBS symptoms and support barrier function.
- L-glutamine: An amino acid that fuels gut cells; dosing often ranges from 5–10 g twice daily.
- Zinc carnosine: Some studies suggest benefit in NSAID-related gut injury and permeability; typical studied doses range around 37.5–75 mg/day.
Other options with mixed or emerging evidence
- Vitamin D (if deficient)
- Curcumin, omega-3s
Proceed with caution or skip
- “Detox” cleanses, extreme herb combos, or high-dose regimens without a clear diagnosis.
- Multi-ingredient “leaky gut repair” powders with proprietary blends.
Unique insight: Supplements should supplement—not replace—diet, sleep, and stress care. Treat them like a 4–8 week experiment with clear goals, then decide whether to continue.
Lifestyle Habits That Strengthen the Gut
Small lifestyle adjustments can support barrier function and symptom relief.
Sleep and circadian rhythm
7–9 hours/night supports immune regulation and microbial balance. Keep consistent bed/wake times.
Stress and the gut–brain axis
Brief daily practices (10 minutes) such as diaphragmatic breathing, mindfulness, or yoga can lower stress hormones that
influence permeability.
Movement
Regular moderate exercise (e.g., brisk walking 30 minutes most days) is gut-friendly. Very intense endurance sessions
can transiently increase permeability—fuel and hydrate well.
NSAID alternatives
Discuss acetaminophen or topical NSAIDs for pain flares when appropriate to reduce small-intestinal injury risk.
Unique insight: Anchor one “keystone habit” per day. People who keep one keystone habit are more likely to maintain
other supportive behaviors.
Safe, Step‑By‑Step Treatment Roadmap
A structured approach helps track progress and identify effective strategies.
The 5R framework (evidence-guided)
- Remove: Trim alcohol, ultra-processed foods, and unnecessary NSAIDs; treat infections if present.
- Replace: Ensure adequate digestive support—chew well, consider peppermint oil for IBS symptoms.
- Reinoculate: Add fiber diversity and fermented foods; consider a time-limited probiotic.
- Repair: Trial L-glutamine and or zinc carnosine if appropriate; correct vitamin D deficiency.
- Rebalance: Sleep, stress, movement.
A 4–8 week plan
- Weeks 1–2: Foundation diet, alcohol reduction, sleep schedule, daily walk; track symptoms.
- Weeks 3–4: Add probiotic or glutamine if needed; continue food variety goals.
- Weeks 5–8: Reassess. If improved, expand foods. If not, consult a doctor online with Apollo 24|7 to personalize testing and next steps.
Unique insight: Use a simple symptom score (0–10) twice weekly for bloating, stool consistency, energy, and mood. Objective trends beat guesswork when adjusting your plan.
When to Seek Medical Care and How Apollo 24|7 Can Help
Knowing when to escalate care ensures safety and timely treatment.
Red flags and timelines
- Seek urgent care: Blood in stool, black tarry stools, fever, severe abdominal pain, or unintentional weight loss.
- If symptoms persist beyond two weeks despite diet/lifestyle changes, consult a doctor online with Apollo 24|7.
- Children, older adults, and those with chronic conditions should seek earlier guidance.
Role of testing and follow-up
- Your doctor may order celiac serology, stool calprotectin, breath testing for SIBO, or nutrient labs. Apollo 24|7 offers home collection for tests like vitamin D or HbA1c.
- A dietitian referral can help if you consider a low FODMAP trial or need a personalized leaky gut syndrome diet plan.
Unique insight: “Test light, iterate fast.” Small, reversible changes often bring relief while you and your clinician decide if targeted tests are warranted.
Conclusion
The idea of “leaky gut syndrome” resonates because it offers a simple explanation for complex symptoms. The truth is nuanced: the gut barrier is dynamic, and increased intestinal permeability can accompany many conditions—but it’s rarely the sole cause. The most effective approach is practical and personalized: rule out serious issues, build a gut-friendly plate, reduce processed foods and alcohol, sleep consistently, manage stress, and trial targeted supplements only when they have a clear purpose.
Small, steady changes can meaningfully improve bloating, energy, and overall well-being without resorting to rigid or costly regimens. If you’ve tried these steps for a couple of weeks without improvement—or if you notice red flags—connect with a clinician. If you prefer convenient, trusted care from home, consult a doctor online with Apollo 24|7 to discuss appropriate tests and a tailored plan. Your gut can be remarkably resilient; with the right inputs, the barrier can strengthen, symptoms can settle, and your routine can feel easier again.
Consult Top Specialists Here
Consult Top Specialists Here

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Harish K C
Gastroenterology/gi Medicine Specialist
15 Years • MBBS MD DM MRCP(UK) (SCE-Gastroenterology and Hepatology)
Bangalore
Manipal Hospital, Bangalore

Dr Rohit Sureka
Gastroenterology/gi Medicine Specialist
15 Years • MBBS, DNB General Medicine, DNB Gastroenterology
Jaipur
Apollo 247 virtual - Rajasthan, Jaipur

Dr. Paramesh K N
Gastroenterology/gi Medicine Specialist
16 Years • MBBS, MS ( General Surgery), DNB ( Surgical Gastroenterology)
Hyderabad
Sprint Diagnostics Centre, Hyderabad

Dr. Shivaraj Afzalpurkar
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD General medicine (Gold medalist), DrNB (Gastroenterology), MNAMS
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
Consult Top Specialists Here

Dr Bhargav Vuppumalla
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD GENERAL MEDICINE
Bengaluru
Apollo Medical Center, Marathahalli, Bengaluru

Dr Harish K C
Gastroenterology/gi Medicine Specialist
15 Years • MBBS MD DM MRCP(UK) (SCE-Gastroenterology and Hepatology)
Bangalore
Manipal Hospital, Bangalore

Dr Rohit Sureka
Gastroenterology/gi Medicine Specialist
15 Years • MBBS, DNB General Medicine, DNB Gastroenterology
Jaipur
Apollo 247 virtual - Rajasthan, Jaipur

Dr. Paramesh K N
Gastroenterology/gi Medicine Specialist
16 Years • MBBS, MS ( General Surgery), DNB ( Surgical Gastroenterology)
Hyderabad
Sprint Diagnostics Centre, Hyderabad

Dr. Shivaraj Afzalpurkar
Gastroenterology/gi Medicine Specialist
13 Years • MBBS, MD General medicine (Gold medalist), DrNB (Gastroenterology), MNAMS
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
More articles from General Medical Consultation
Frequently Asked Questions
1) What are the most common signs of leaky gut in adults?
Bloating, gas, irregular stools, and fatigue are commonly reported. They are nonspecific and can overlap with IBS, celiac disease, thyroid issues, and nutrient deficiencies. If symptoms persist, consult a doctor online with Apollo 24|7 for evaluation.
2) Is there a definitive intestinal permeability test at home?
Not really. The lactulose–mannitol test estimates permeability but is influenced by multiple factors and isn’t widely used clinically. Focus first on diet and lifestyle changes; if symptoms persist, your doctor can advise on the right test at the right time.
3) Which foods to heal leaky gut fast?
There’s no “fast cure,” but a Mediterranean-style diet with diverse fiber and fermented foods supports the gut lining. Reduce alcohol and ultra-processed foods. Track what helps you personally.
4) Are zonulin tests accurate for diagnosing leaky gut?
Many commercial zonulin assays are unreliable and may not measure zonulin specifically, limiting their clinical utility. They’re not recommended for routine diagnosis.
5) What’s the best probiotic for leaky gut?
Benefits are strain-specific. Lactobacillus rhamnosus GG or Bifidobacterium longum are common starting points for IBS-like symptoms. Trial one product for 4–8 weeks; if no change, stop. Combine with diet and stress care.