What Leads to Signs of Raynaud’s Disease
Learn what causes Raynaud’s disease, who’s at risk, and how to prevent and manage attacks effectively. Discover practical lifestyle tips, diagnosis, and treatment options.

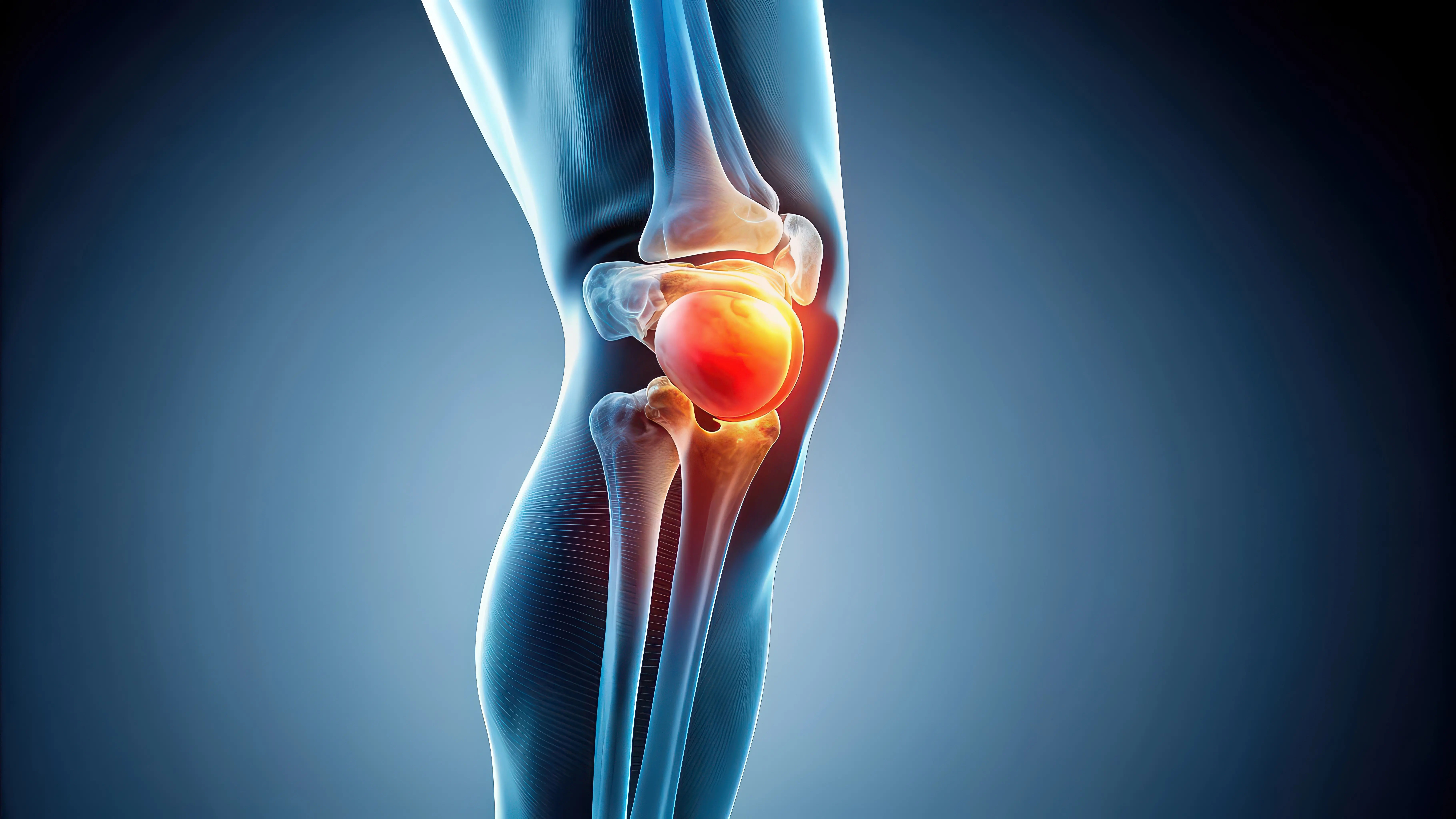
.webp?tr=q-80,f-webp,w-350,dpr-2,c-at_max 700w)
Introduction
When your fingers or toes suddenly turn white or blue in the cold—or even during stress—it can be alarming. These colour changes, along with numbness and tingling, are hallmark signs of Raynaud’s disease (also known as Raynaud’s phenomenon or Raynaud’s disease). This circulation condition causes temporary narrowing of blood vessels in response to triggers like cold temperatures or emotional stress. In this clear, comprehensive guide, we’ll explain exactly what leads to those signs, who’s at risk, how doctors diagnose it, and the most effective ways to prevent and treat attacks. You’ll find practical tips you can use today, trustworthy data from leading medical sources, and guidance on when to seek professional care. Whether you’ve newly noticed symptoms or you’ve been managing Raynaud’s for years, this article will help you understand the disease, Raynaud’s triggers, and the steps you can take to stay comfortable and protect your hands and feet.
Note: If symptoms are frequent, severe, or affecting your daily life, consult a doctor. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. They can also organise lab tests and imaging if needed.
How This Guide Was Planned (Brief Analysis of Top Pages)
Here’s how this guide was developed:
- We reviewed leading resources that rank highly for “Raynaud’s disease” and “Raynaud’s phenomenon,” including Mayo Clinic, NHS, NIAMS (NIH), Cleveland Clinic, and MedlinePlus.
Common structures across these pages include:
- Clear definitions and types (primary vs secondary)
- Signs and symptoms (colour changes: white-blue-red)
- Triggers (cold, stress, vibration, medications)
- Risk factors (sex, age, family history, autoimmune conditions)
- Diagnosis (history, nailfold capillaroscopy, ANA and other blood tests)
- Treatment (warming, stress management, calcium channel blockers)
- Complications (ulcers, infections)
When to see a doctor
What’s often missing: nuanced lifestyle tactics that actually work day-to-day, guidance for special populations (pregnancy, kids), and an explanation of how vasospasm and the nervous system drive the signs. This guide fills those gaps while covering the essentials.
Understanding Raynaud’s Disease (and Phenomenon)
Here’s what to know about Raynaud’s disease:
Raynaud’s disease describes a condition where small arteries that supply your fingers and toes spasm and narrow. This limits blood flow, leading to colour changes (often white to blue to red), numbness, tingling, pain, or a “pins and needles” feeling. The core mechanism is temporary vasospasm—think of it as a sudden “tightening” of the blood vessel in response to cold or stress. The term Raynaud’s phenomenon is often used interchangeably, but many clinicians use “Raynaud’s disease” for cases with no underlying cause (primary) and “Raynaud’s phenomenon” when it’s secondary to another condition.
- Primary Raynaud’s: The most common type, usually milder. Episodes are uncomfortable but generally not dangerous. It often begins between ages 15 and 30 and is more common in women.
- Secondary Raynaud’s: Less common but more serious because it’s triggered by another health issue—often an autoimmune or connective tissue disease such as scleroderma, lupus, or rheumatoid arthritis. Secondary cases can lead to complications like skin sores (digital ulcers) and, rarely, tissue damage.
How common is it? Raynaud’s affects roughly 3–5% of the population, with higher prevalence in colder climates and women. Although cold is a clear trigger, people living in warm regions can still experience attacks—from aggressive air-conditioning or stress—not just outdoor winter weather.
Consult Top Specialists Here
What Leads to the Signs: The “Why” Behind Attacks
Here’s what causes Raynaud’s attacks:
Raynaud’s attacks happen in distinct stages:
- White (pallor): As the vessel spasms, blood flow drops, turning the skin pale and numb.
- Blue (cyanosis): Prolonged low oxygen in the tissues causes a bluish colour and aching.
- Red (reactive hyperaemia): As the spasm resolves and blood rushes back, the area reddens, often throbbing or tingling.
Triggers:
- Cold exposure: Even minor temperature drops—grabbing a cold drink or reaching into the freezer—can trigger an episode.
- Emotional stress: Adrenaline activates the sympathetic nervous system, tightening blood vessels.
- Vibration or pressure: Repeated use of power tools or tight jewellery can compress or irritate vessels.
Some people are more sensitive due to:
- Vessel reactivity or differences in receptor sensitivity
- A more reactive sympathetic nervous system
Underlying autoimmune inflammation or damage
An everyday example: A teacher keeping a chilly classroom window open notices her fingers blanch when handing out cold juice boxes. If she warms her hands first or wears thin gloves, the symptoms reduce. Small behavioural shifts can make a big difference.
Primary vs Secondary: Underlying Causes That Matter
Here’s why the distinction between primary and secondary Raynaud’s matters:
- Autoimmune/connective tissue disease: Scleroderma, lupus, mixed connective tissue disease, rheumatoid arthritis, and Sjögren’s syndrome frequently overlap with Raynaud’s.
- Occupational/environmental: Regular use of vibrating tools, exposure to vinyl chloride, or injury/frostbite can contribute.
- Medications: Beta-blockers, migraine medicines, ADHD stimulants, decongestants, and some chemotherapy agents can worsen attacks.
- Mechanical factors: Tight rings, wristbands, or carpal tunnel syndrome can increase susceptibility.
- If you’ve developed Raynaud’s after starting new medication or a vibration-heavy job, share that timeline with your clinician—it helps guide diagnosis and treatment.
Who Is at Risk?
Here’s who is most likely to develop Raynaud’s:
- Women aged 15–30 (for primary Raynaud’s)
- People living in colder regions or working in cold environments
- Those with a family history
- Smokers or those exposed to nicotine
- People consuming high caffeine
- Individuals with autoimmune disease, hypothyroidism, or peripheral arterial disease
Workers exposed to vibration or cold storage environments
Small daily habits—like wearing tight fitness trackers or handling cold objects—can also trigger attacks.
Recognising the Signs—and When to Worry
Here’s what to watch for:
- Colour changes in fingers or toes: white → blue → red
- Numbness, tingling, stinging, or burning
- Cold fingers or toes despite warm surroundings
- Episodes lasting minutes to an hour
Areas affected may include fingers, toes, ears, nose tip, lips, and sometimes nipples.
Seek medical care promptly if:
- Symptoms are one-sided
- Pain, sores, or skin discolouration persist
- Onset occurs after age 40 or symptoms worsen quickly
- You notice other autoimmune signs (rashes, joint pain, etc.)
Triggers and Prevention Strategies that Actually Work
Here’s how to prevent attacks:
Cold-proofing strategies:
- Dress in layers and prioritise core warmth.
- Use mittens instead of gloves for extreme cold.
- Pre-warm hands before going outside.
- Protect indoors with warm socks or wrist warmers.
- Avoid cold metal or air-conditioned environments unprepared.
Stress control: - Practice paced breathing (inhale 4s, exhale 6s).
- Take micro-breaks to stretch and unclench hands.
- Try biofeedback or mindfulness-based stress reduction.
Lifestyle:
- Stay hydrated.
- Limit caffeine and quit smoking.
- Build a pre-warming routine before exposure to cold.
How Doctors Diagnose Raynaud’s
Here’s how doctors identify Raynaud’s:
- History: Age of onset, triggers, family history, and work environment.
- Physical exam: Skin changes and nail abnormalities.
Tests:
- Nailfold capillaroscopy: Checks capillary shape and density.
- Blood tests: ANA, ESR/CRP, thyroid function, and others.
- Vascular studies: Doppler ultrasound to assess blood flow if needed.
If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7 for evaluation.
Self-Care and Lifestyle Treatment
Here’s how to manage Raynaud’s at home:
- Keep a “Raynaud’s kit” with warmers, gloves, and a thermos.
- Massage hands under warm water during an attack.
- Exercise regularly to boost circulation.
- Moisturise to protect skin and prevent ulcers.
- Use biofeedback to consciously warm hands.
Identify your “cold checkpoints” and pre-warm before exposure.
Medications and Advanced Options
- Here’s how doctors treat persistent Raynaud’s:
- First-line: Calcium channel blockers (nifedipine, amlodipine).
- Other options: Topical nitroglycerin, PDE-5 inhibitors, ARBs, SSRIs.
- Severe cases: IV prostacyclin analogues, sympathectomy, or botulinum toxin injections.
- During pregnancy, medication options may differ—consult your doctor.
Complications and Living Well Long-Term
Here’s how to protect yourself long-term:
Potential complications:
- Digital ulcers
- Infections
- Rarely, tissue damage or gangrene
Prevention:
Inspect fingers and toes daily.- Treat minor cuts early.
- Avoid self-treating severe pain or discolouration—seek care immediately.
Special situations: - Autoimmune overlap requires close monitoring.
- Nipple vasospasm during breastfeeding can improve with warmth.
- Children often experience primary, milder forms but still need evaluation.
- Smart warming tools—like heated gloves or insoles—can help prevent full attacks.
Consult Top Specialists Here
Conclusion
Raynaud’s disease can feel disruptive, but understanding what leads to its signs gives you control. At its core, Raynaud’s is about blood vessels that overreact to cold or stress. With the right mix of prevention (warming routines, stress management), smart daily habits (layered clothing, indoor protection, a ready “Raynaud’s kit”), and medical support when needed, most people reduce attacks and protect their fingers and toes. If your symptoms are new, severe, or associated with sores or other health changes, talk to a clinician to check for secondary causes and tailor a safe treatment plan. Your next step can be simple: identify your top two triggers and add a 60-second pre-warm ritual before they occur. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo 24|7 for a personalised plan.
Consult Top Specialists Here

Dr Sahana Gangatkar
General Physician/ Internal Medicine Specialist
8 Years • MBBS, MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
(25+ Patients)

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ajay K Sinha
General Physician/ Internal Medicine Specialist
30 Years • MD, Internal Medicine
Delhi
Apollo Hospitals Indraprastha, Delhi
(200+ Patients)

Dr. Rohit Basu
General Practitioner
8 Years • MBBS, DNB (General surgery)
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
Dr. Naresh
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (General Medicine)
Mahbubnagar
SIMS HOSPITAL, Mahbubnagar
Consult Top Specialists Here

Dr Sahana Gangatkar
General Physician/ Internal Medicine Specialist
8 Years • MBBS, MD
Bengaluru
Apollo Clinic, JP nagar, Bengaluru
(25+ Patients)

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Ajay K Sinha
General Physician/ Internal Medicine Specialist
30 Years • MD, Internal Medicine
Delhi
Apollo Hospitals Indraprastha, Delhi
(200+ Patients)

Dr. Rohit Basu
General Practitioner
8 Years • MBBS, DNB (General surgery)
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
Dr. Naresh
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD (General Medicine)
Mahbubnagar
SIMS HOSPITAL, Mahbubnagar
More articles from General Medical Consultation
Frequently Asked Questions
What causes Raynaud’s attacks to start so suddenly?
Sudden cold or stress activates the sympathetic nervous system, causing vasospasm in small arteries. This reduces blood flow and triggers the white-blue-red colour changes seen in Raynaud’s phenomenon.
How can I tell if I have primary vs secondary Raynaud’s?
Primary usually starts younger, is symmetric, and has milder symptoms without ulcers. Secondary may start later, be more severe, and occur with other signs of autoimmune disease. Tests like nailfold capillaroscopy and ANA can help distinguish them; ask your doctor or consult Apollo 24|7 online if you’re unsure.
What are the best gloves for Raynaud’s disease?
Layered gloves work best: thin liners plus insulated mittens. For severe cold, try battery-heated gloves or chemical hand warmers. Choose windproof, water-resistant materials.
Can caffeine or smoking trigger Raynaud’s?
Yes. Nicotine constricts blood vessels, and high caffeine can increase sympathetic tone, making attacks more likely. Quitting smoking and moderating caffeine can reduce flare-ups.
What tests will my doctor order for Raynaud’s phenomenon diagnosis?
History and exam come first. Nailfold capillaroscopy evaluates tiny capillaries; blood tests like ANA and ESR/CRP screen for autoimmune causes; thyroid tests and vascular studies may also be used. Apollo 24|7 offers home collection for many of these labs.