Your Guide to New Generation Pacemakers
Know about the new generation pacemaker, how they are different from traditional ones, when you need it, features like smart sensing and safe options and more.

Introduction
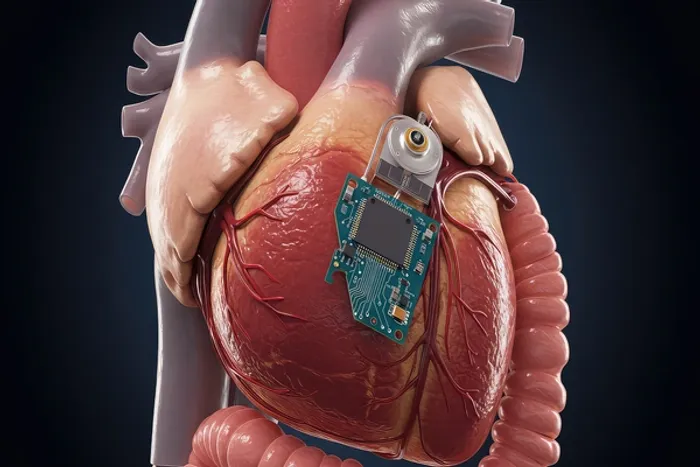
Pacemakers have quietly evolved from simple lifesavers into smart, discreet partners in heart health. New generation pacemakers are smaller, safer, and more connected than ever—some are even leadless and can be checked from home. If you or a loved one has been told you might need a pacemaker, understanding today’s options can help you feel confident and in control. In this guide, we break down what’s truly new about new generation pacemakers: how they work, who needs them, the differences between traditional and leadless devices, how remote monitoring works, what to expect during surgery and recovery, and how to live an active life after implantation. We’ll also cover MRI safety, battery life, potential risks and how modern designs reduce them, plus costs, insurance considerations, and what’s coming next (from physiologic pacing to AI-assisted care). Along the way, we’ll share practical tips and key questions to ask your cardiologist so you can make the best choice for your heart and lifestyle.
Consult a Top General Practitioner for Personalised Advice
What’s Different About New Generation Pacemakers?
The newest pacemakers do more than keep a slow heartbeat steady—they’re designed to fit your life. Three breakthroughs define new-generation pacemakers:
- Leadless designs. Instead of wires (leads) running through a vein into the heart, leadless pacemakers are miniaturised capsules placed directly inside the right ventricle via a catheter. No chest pocket means fewer pocket- or lead-related complications and a quicker recovery in many cases.
- Connected care. Bluetooth-enabled transmitters and secure remote monitoring let your care team track device performance and heart rhythm from home. This can catch issues earlier, reduce clinic visits, and provide peace of mind.
- MRI-conditional capability. Most modern devices are built to be MRI-conditional, allowing many patients to safely undergo MRI scans under specific protocols. This is important, as many people with devices will need MRI imaging in their lifetime.
Do You Need a Pacemaker? Symptoms, Tests, and Timing
Pacemakers are recommended when slow or irregular heart rhythms (arrhythmias) cause symptoms or pose risks. Common symptoms include fatigue, dizziness, near-fainting or fainting (syncope), shortness of breath, exercise intolerance, and episodes of confusion (especially in older adults). Some people feel “pauses” or fluttering. Not all slow heart rates need treatment, but when they do, a pacemaker can restore a safe rhythm.
How doctors decide:
- ECG and Holter monitor: Identify rhythm problems (like sinus node dysfunction or atrioventricular block).
- Event/loop recorders: Useful for intermittent symptoms.
- Echocardiogram: Checks heart structure and pumping function, important for deciding if biventricular pacing (CRT) may help.
- Symptoms + rhythm correlation: If fainting aligns with a serious pause or block, a pacemaker can prevent dangerous recurrences.
When to seek help: Call emergency services for fainting, chest pain, or severe breathlessness. If symptoms of dizziness or fatigue persist beyond two weeks, consult a doctor online with Apollo 24|7 for further evaluation. If testing is advised (for example, thyroid levels or electrolytes that can affect rhythm), Apollo 24|7 offers convenient home collection for common lab tests. Early assessment ensures that if a pacemaker is needed, you’re choosing it for the right reasons.
Today’s Pacemaker Options: Traditional, Leadless, and CRT
Traditional transvenous pacemakers:
- Single-chamber: One lead, usually in the right ventricle (RV), helps when only ventricular pacing is needed.
- Dual-chamber: Leads in the right atrium and RV to coordinate atrial and ventricular beats. Useful for AV block.
- Biventricular (CRT-P): Adds a lead to the left ventricle to resynchronize pumping in certain heart failure patients; can improve symptoms and quality of life.
Leadless pacemakers:
- What’s new: Tiny, self-contained devices implanted directly into the RV via a leg vein. No chest incision or lead wires, so fewer pocket infections and lead problems. Studies and registries report high implantation success and lower major complications compared with traditional single-chamber systems.
- Limitations are narrowing: Early leadless devices paced only the ventricle (VVI). Newer models added atrial-sensing features (for AV synchrony), and a dual-chamber leadless system has been FDA-approved, enabling communication between atrial and ventricular modules for truly dual-chamber leadless pacing. Battery life for leadless systems often approaches a decade or more, depending on pacing needs.
Physiologic pacing (conduction-system pacing):
His-bundle pacing and left bundle branch area pacing (LBBAP) aim to use your heart’s natural wiring, preserving coordinated activation and reducing pacing-induced weakening of the heart. 2023 expert guidance supports physiologic pacing in select patients, especially those needing a lot of RV pacing or who have heart failure. This is an exciting frontier within new generation pacemakers because it prioritises natural heart mechanics.
Smarter Sensing, Safer Imaging, and Connected Care
The smarter and safer options include:
Remote monitoring and apps:
Most new generation pacemakers wirelessly transmit device and rhythm data to secure systems that your clinic can review. This enables earlier detection of battery changes, lead issues, atrial arrhythmias, or heart failure trends, potentially preventing complications and unplanned visits. Professional society guidance recommends routine remote monitoring for cardiac implantable devices. Some systems pair with home hubs or smartphone apps for easy setup.
MRI-conditional devices:
Historically, MRI scans posed risks to patients with older pacemakers. Modern MRI-conditional devices, when scanned under specific protocols in qualified centres, allow many patients to safely undergo MRI. Given how often MRIs are needed over a lifetime, this is a major advantage of new-generation pacemakers. Always carry your device card and inform imaging staff.
Security and reliability:
Manufacturers use encryption and authentication to protect device data. Cybersecurity is an ongoing focus, and FDA oversight requires robust risk management. Remote alerts help your clinic act quickly if thresholds change or if an arrhythmia appears.
The Procedure and Recovery—What to Expect
Before the procedure:
- Your team will review medications (especially blood thinners), check for infection risks, and confirm the device plan.
- You’ll receive local anaesthesia and light sedation for most pacemaker implants. The procedure typically lasts 1–2 hours.
How it’s done:
- Transvenous pacemaker: A small chest incision creates a pocket under the skin. Leads are threaded through a vein into the heart and connected to the generator in the pocket. The system is tested, and the incision is closed.
- Leadless pacemaker: Inserted through a vein in the groin using a catheter, the miniature device is positioned in the right ventricle and attached with tiny tines, then tested and released—no chest pocket needed.
Recovery:
- Many patients go home the same day or after one night. For transvenous systems, you’ll limit arm motion on the implant side for 1–2 weeks to prevent lead displacement. Expect mild soreness; bruising can happen.
- For leadless systems, you’ll follow groin-care instructions and temporarily limit heavy lifting.
Reducing risks:
- Infection prevention includes antibiotics, careful sterile technique, and, in higher-risk patients, an antibacterial envelope (a mesh placed around the generator) can further reduce infections. In a major clinical trial, this approach lowered the risk of serious device infections compared with standard care.
- Watch for warning signs: fever, increasing redness or drainage at the incision, swelling, sudden dizziness, fainting, or palpitations. If your condition does not improve after trying these methods, book a physical visit to a doctor with Apollo24|7 for examination and device checks.
Living Well With New Generation Pacemakers
Everyday life:
- Exercise: Most people gradually return to normal activity in a few weeks. Your device is programmed to accommodate daily exertion; some systems use sensors (like accelerometers) to adjust pacing during activity.
- Travel and airport security: Carry your device card. Walk through airport scanners normally; if screened with a handheld wand, ask staff not to hold it over the device. Leadless systems eliminate bumping at a chest pocket—often more comfortable for seatbelts and backpacks [10].
Electronics and magnets:
- Keep smartphones and wearables at least 6 inches (15 cm) from the device; use the opposite-side pocket. Avoid placing magnetic accessories directly over the device. Household appliances (microwaves, induction stoves) are safe when used as intended. For rare industrial-strength magnets or welding, ask your care team for specific advice.
Follow-up:
- Remote checks occur on a schedule set by your clinic, with in-person visits to review settings and battery status. Battery life varies (often 7–15 years for transvenous, up to ~10+ years for leadless, depending on usage).
- Replacements are straightforward: a new generator is attached to existing leads (if healthy), or a new leadless device is implanted when needed.
Costs, Access, and Choosing the Right Device
What drives cost:
Device type (leadless pacemakers typically cost more than traditional systems), number of leads, hospital setting, and any additional technologies (e.g., antibacterial envelope) all influence cost. Insurance coverage varies by region and policy; medically indicated devices are often covered.
Conclusion
Pacemakers have come a long way—and the latest advances are designed for real life. New generation pacemakers offer sleeker designs (including leadless options), safer imaging access through MRI-conditional systems, and continuous connection via remote monitoring. For many people, this translates to fewer complications, quicker recoveries, and better day-to-day confidence. Your choice of device should match your diagnosis, lifestyle, and long-term goals. Traditional transvenous systems remain excellent and versatile. Leadless pacemakers can be ideal when minimising infection risk or avoiding a chest pocket is important. For those needing resynchronisation, CRT can restore coordinated pumping and improve quality of life. And physiologic pacing approaches help preserve your heart’s natural function when heavy pacing is anticipated. If you’re experiencing ongoing dizziness, fainting, or fatigue, consult a doctor online with Apollo24|7 for evaluation and guidance. With the right information and support, you can choose a pacemaker that not only protects your heart but also fits your life.
Consult a Top General Practitioner for Personalised Advice
Consult a Top General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Shesham Srinidhi
General Practitioner
5 Years • MD(physician)
Hyderabad
Apollo 24|7 Clinic, Hyderabad
(150+ Patients)

Dr Divya Lekha Gunta
General Practitioner
10 Years • MBBS, MD (Pathology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
Consult a Top General Practitioner for Personalised Advice

Dr. Mainak Baksi
General Practitioner
13 Years • MBBS , MD (MPH)
Howrah
Mainak Baksi Clinic, Howrah
(50+ Patients)

Dr. Shesham Srinidhi
General Practitioner
5 Years • MD(physician)
Hyderabad
Apollo 24|7 Clinic, Hyderabad
(150+ Patients)

Dr Divya Lekha Gunta
General Practitioner
10 Years • MBBS, MD (Pathology)
Visakhapatnam
Apollo 24|7 Clinic - Andhra Pradesh, Visakhapatnam

Dr. Siri Nallapu
General Practitioner
5 Years • MBBS
Hyderabad
Apollo 24|7 Clinic, Hyderabad

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore
More articles from General Medical Consultation
Frequently Asked Questions
How long do new-generation pacemakers last?
Many last 7–15 years, depending on how much pacing is needed; leadless models can approach a decade or more. Your clinic will estimate battery life and monitor it via remote checks. (Related keyword: pacemaker battery life years)
Can I get an MRI with a pacemaker?
Most new devices are MRI-conditional. With proper protocols and in a qualified centre, many patients can safely undergo MRI scans. Always carry your device card. (Related keyword: MRI-safe pacemaker compatibility)
Are leadless pacemakers better than traditional ones?
They can reduce pocket and lead complications and improve comfort for some. However, traditional systems remain best for many pacing needs, including CRT. Your condition and goals guide the choice. (Related keyword: leadless pacemaker vs traditional)
Will my phone or smartwatch interfere with my pacemaker?
Keep phones and magnets at least 6 inches from the device and avoid placing magnetic accessories over the implant site. Most everyday electronics are safe when used normally. (Related keyword: pacemaker and smartphone interference)
What signs of infection should I watch for?
Fever, increasing redness or drainage from the incision, swelling, or persistent pain. Seek medical care promptly. If symptoms persist beyond two weeks, consult a doctor online with Apollo 24|7.