Heart Attack Triggers: Common Triggers, Signs And Management Of Heart Attack
Discover the common triggers of heart attacks, including stress, unhealthy habits, and underlying health conditions. Learn how to manage these risks to protect your heart health.

Written by Dr.Sonia Bhatt
Last updated on 3rd Jul, 2025

A heart attack, also known as a myocardial infarction, is a life-threatening condition that occurs when blood flow to a portion of the heart muscle is severely reduced or completely blocked. This disruption is most commonly caused by a blockage in one or more coronary arteries, though other factors can also contribute to the condition. Recognising these triggers and understanding their impact can play a vital role in prevention and timely intervention.
Common Triggers of Heart Attacks
Some of the most common triggers of heart attack are as follows:
1. Emotional Stress and Anxiety
Emotional stress and anxiety can trigger a heart attack by causing a sudden spike in blood pressure and heart rate. This increased strain on the heart may lead to plaque rupture or coronary artery spasms, cutting off blood flow to the heart.
2. Physical Exertion and Overexertion
While regular exercise is crucial for heart health, overexertion can be dangerous, especially for those with underlying heart conditions. Intense physical activity may place excessive stress on the heart, leading to a heart attack in susceptible individuals.
3. Unhealthy Diet and Lifestyle
A diet high in unhealthy fats, sodium, and sugar, combined with a sedentary lifestyle, contributes to risk factors such as obesity, high cholesterol, and hypertension. These conditions significantly increase the likelihood of heart attacks
Medical Conditions Increasing Risk of Heart Attack
The most common medical conditions that increase the risk of heart attack are:
1. Hypertension
High blood pressure, or hypertension, forces the heart to work harder, leading to thickened heart walls and increased stress on coronary arteries. Over time, this can damage the heart and lead to a heart attack.
2. Diabetes
Diabetes damages blood vessels and nerves, increasing the likelihood of plaque buildup in the arteries. High blood sugar levels also contribute to inflammation and narrowing of coronary arteries, raising the risk of heart attacks.
3. Atherosclerosis
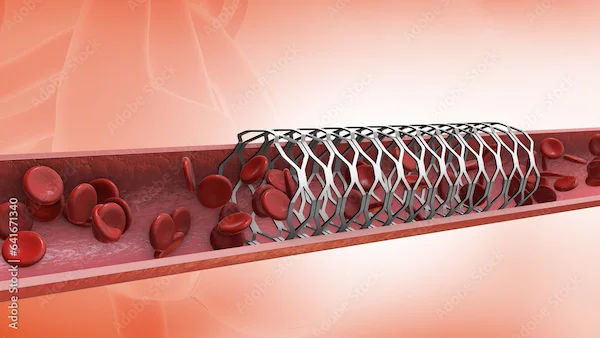
Atherosclerosis, characterised by the buildup of fatty deposits (plaque) in arteries, is a leading cause of heart attacks. Plaque can rupture, leading to the formation of blood clots that block blood flow to the heart.
Environmental and Situational Factors
Environmental and situational factors that may trigger heart attack are as follows:
1. Weather Extremes
Extreme temperatures, particularly cold weather, can constrict blood vessels, raising blood pressure and increasing the risk of heart attacks. Heatwaves can also place undue stress on the cardiovascular system.
2. Air Pollution and Heart Health
Exposure to air pollution and fine particulate matter can lead to inflammation in blood vessels and increase the risk of plaque rupture, contributing to heart attacks.
Demographic Factors
Demographic factors that may lead to a heart attack are as follows:
1. Age and Gender Differences in Heart Attack Triggers
Men are generally at a higher risk of heart attacks at a younger age than women. However, post-menopausal women experience an increased risk due to decreased estrogen levels, which normally provide some cardiovascular protection.
2. Genetic Predisposition
A family history of heart disease significantly increases an individual’s risk of heart attacks. Genetic factors can influence cholesterol levels, blood pressure, and other cardiovascular conditions thus increasing the risk of heart attack.
Role of Medications and Substance Abuse
Some prescription medications and substance abuse may also lead to heart attacks.
1. Impact of Prescription Medication
Certain medications, such as those that increase blood clotting or raise blood pressure, can contribute to heart attack risk. Always consult a healthcare provider about the potential side effects of prescribed medications.
2. Influence of Alcohol, Tobacco, and Drugs
Excessive alcohol consumption, smoking, and recreational drug use (e.g., cocaine or amphetamines) can damage blood vessels, raise blood pressure, and lead to coronary artery spasms, significantly increasing the risk of heart attacks.
Recognising Early Signs and Symptoms
Heart attack signs and symptoms can vary widely. Some individuals experience mild symptoms, others have severe symptoms, and some may not notice any symptoms at all. Some of the common signs and symptoms of heart attack are as follows:
Chest pain or discomfort, often described as pressure, tightness, squeezing, aching, or pain
Pain or discomfort that radiates to the shoulders, arms, back, neck, jaw, teeth, or occasionally the upper abdomen
Cold sweats
Unusual fatigue
Feelings of heartburn or indigestion
Lightheadedness or sudden dizziness
Nausea
Shortness of breath
If you experience any of these symptoms, seek immediate medical attention, as timely treatment can save lives.
Diagnostic Techniques for Heart Attack
A variety of tests may be conducted to confirm and assess the severity of a heart attack. These include:
Electrocardiogram (ECG or EKG): This is often the first test performed to diagnose a heart attack. It records the electrical activity of the heart using sticky patches (electrodes) placed on the chest, arms, and legs. The electrical signals are displayed as waves on a monitor or printed on paper. An ECG can indicate whether a heart attack is occurring or has occurred.
Blood Tests: After a heart attack, certain proteins (cardiac markers) are released into the bloodstream due to heart muscle damage. Blood tests measure these proteins to help diagnose a heart attack.
Chest X-ray: This imaging test provides details about the size and condition of the heart and lungs, helping to rule out other potential causes of symptoms.
Echocardiogram: Using sound waves (ultrasound), this test creates moving images of the heart. It shows how blood flows through the heart and valves, helping identify areas of the heart that may have been damaged.
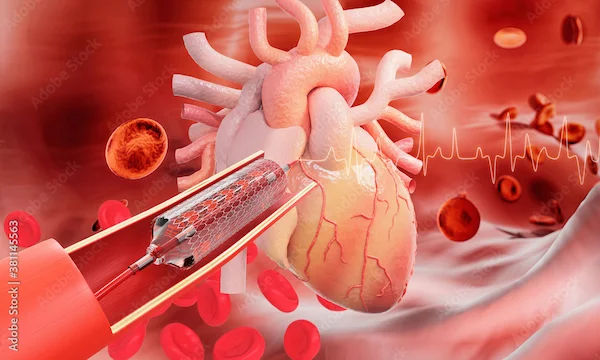
Coronary Catheterisation (Angiogram): In this procedure, a long, thin tube (catheter) is inserted into an artery, usually in the leg, and guided to the heart. A special dye is injected through the catheter, making the coronary arteries visible on X-ray images to detect blockages.
Cardiac Computed Tomography (CT) or Magnetic Resonance Imaging (MRI): These advanced imaging tests create detailed pictures of the heart and chest. A cardiac CT scan uses X-rays, while a cardiac MRI employs a magnetic field and radio waves. Both tests can assess heart damage and provide insights into the severity of the condition.
These tests play a crucial role in accurately diagnosing a heart attack, assessing the extent of damage, and determining the most effective treatment plan.
Prevention and Risk Management
Adopting healthy lifestyle habits can significantly reduce the risk of heart attack while also helping manage these conditions effectively.
Healthy Diet: Consume a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
Regular Exercise: Engage in moderate physical activities like walking, swimming, or cycling for at least 30 minutes regularly.
Quit Smoking and Limit Alcohol: Avoid tobacco products, exposure to secondhand smoke and alcohol intake.
Manage Stress: Practice stress-relief techniques such as yoga, meditation, or deep breathing.
Monitor Health Conditions: Regularly check and control blood pressure, cholesterol, and blood sugar levels.
Understand Risk Factors: Know your family history and discuss it with your healthcare provider to understand your risk of heart disease.
Take Medications as Prescribed: If there are existing conditions such as hypertension, diabetes, or high cholesterol, take prescribed medications consistently.
Implementing these changes can enhance heart health, reduce the risk of complications, and improve the quality of life for individuals at risk of or living with heart conditions.
Conclusion
Heart attacks remain a significant health concern, affecting millions worldwide each year. By understanding the various triggers ranging from emotional stress and lifestyle choices to environmental and demographic factors, we can take proactive steps toward prevention. Early recognition of symptoms, timely medical intervention, and adherence to a heart-healthy lifestyle are vital to reducing the risk and impact of heart attacks. Educating ourselves and others about risk factors, early warning signs, and preventive strategies empowers individuals to make informed decisions about their health. With lifestyle modifications, proper management of pre-existing medical conditions, and regular check-ups, it is possible to significantly lower the risk of heart attacks and enhance overall well-being.
Consult Top Cardiologist
Consult Top Cardiologist

Dr. Sarita Rao
Cardiologist
17 Years • MBBS, DM (Cardiology)
Indore
Apollo Hospitals Vijay Nagar, Indore

Dr. Sumanjita Bora
Cardiologist
9 Years • MBBS, PGDCC
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Ramalinga Reddy
General Physician
5 Years • MBBS MD General medicine
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru