Guide to What You Need Know About Stents
Learn all about stents, including their types, how they are inserted, and what to expect during recovery. Our comprehensive guide provides essential information for patients considering or living with a stent.

Written by Dr. J T Hema Pratima
Reviewed by Dr. Dhankecha Mayank Dineshbhai MBBS
Last updated on 13th Jan, 2026

Introduction
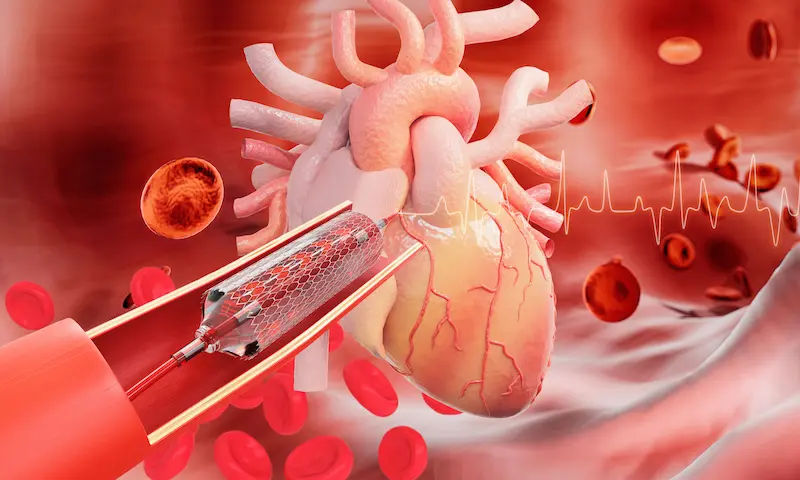
When an artery carrying vital blood to your heart becomes clogged, the consequences can be serious. Thankfully, modern medicine offers a remarkable solution: the stent. This tiny, mesh-like tube acts as a scaffold, propping open narrowed or weakened arteries to restore healthy blood flow. If you or a loved one has been advised to get a stent, it's natural to have questions. What is it made of? How is it placed? What does life look like afterwards? This guide demystifies the entire process, from the procedure itself to the crucial recovery steps. We’ll break down the types of stents, explain why they’re used, and empower you with the knowledge you need to navigate your journey to better heart health, ensuring you can partner effectively with your healthcare team.
What exactly is a stent? More Than Just a Tiny Tube
A stent is a small, flexible, mesh-like tube manufactured from metal or plastic. Its primary purpose is to provide mechanical support to a passageway within the body, preventing it from collapsing or narrowing again after it has been opened. Think of it like a scaffold used in construction; it holds the walls of the artery open so that blood can flow freely to the heart muscle, relieving symptoms like chest pain and preventing heart attacks.
While most people associate stents with heart disease, they are incredibly versatile medical devices. Their application depends on their design and the material they are made from, which are tailored to withstand the specific pressures and environment of the area they are placed in.
The Anatomy of a Stent: Materials and Design
Modern stents are engineering marvels. They are typically laser-cut from a single piece of medical-grade metal alloy, such as cobalt-chromium or platinum-chromium. These materials are chosen for their strength, flexibility, and biocompatibility (meaning they are less likely to cause an adverse reaction in the body). The mesh design allows the stent to be compressed onto a balloon catheter, navigated through the vascular system, and then expanded to its full size. This design also allows the natural artery tissue to grow through and around it, eventually incorporating it into the vessel wall.
A Brief History: How Stenting Became a Lifesaving Standard
The concept of stenting began in the 1980s. While balloon angioplasty (inflating a balloon inside a narrowed artery) was effective, a major problem remained: the artery often narrowed again afterwards, a process called restenosis. The first stent was implanted in a human coronary artery in 1986 by French doctors Jacques Puel and Ulrich Sigwart. It was a revolutionary solution to restenosis, providing a permanent scaffold. The U.S. FDA approved the first coronary stent in 1994. Since then, technology has advanced rapidly, leading to the development of drug-eluting stents that further reduce the risk of re-narrowing.
Consult Top Specialists
Why Would You Need a Stent? The Conditions They Treat
The decision to use a stent is based on the need to quickly and effectively open a blocked passageway to restore essential flow—whether it's blood, bile, or urine.
Coronary Artery Disease: The Primary Reason
The most common use for stents is to treat coronary artery disease (CAD). CAD is caused by atherosclerosis, a buildup of waxy plaque made of cholesterol, fat, and other substances inside the coronary arteries. This buildup narrows the arteries, limiting the supply of oxygen-rich blood to the heart muscle.
Symptoms Leading to a Stent: Angina and Heart Attacks
As arteries narrow, they can cause angina—chest pain or discomfort that occurs when the heart muscle doesn't get enough blood. This often feels like pressure or squeezing in the chest. If a plaque ruptures, a blood clot can form, completely blocking the artery and causing a heart attack (myocardial infarction). In emergency situations, a stent placement procedure is a primary treatment to open the blockage during a heart attack, limiting damage to the heart muscle. In non-emergency situations, it's used to relieve persistent angina that doesn't respond to medication.
Beyond the Heart: Stents in Other Arteries
The utility of stents extends beyond the heart. They are used in:
Carotid Arteries: To prevent strokes by opening blockages in the neck arteries supplying blood to the brain.
Peripheral Arteries: To treat Peripheral Artery Disease (PAD) in the legs, relieving pain and preventing tissue death.
Renal Arteries: To improve blood flow to the kidneys in cases of renal artery stenosis, which can cause high blood pressure and kidney failure.
Aorta: Larger, covered stents (stent-grafts) are used to repair aortic aneurysms, a dangerous bulging of the body's main artery.
Stents for Non-Arterial Issues: Urinary and Bile Ducts
Stents are also crucial in other areas of medicine. Ureteral stents hold open the tubes between the kidneys and bladder to allow urine drainage, often used after kidney stone treatment. Similarly, esophageal stents can open blockages in the throat, and biliary stents are used to open blocked bile ducts caused by cancers or gallstones.
The Stent Placement Procedure: What to Expect
The process of placing a stent is minimally invasive and is most commonly performed during a procedure called angioplasty.
Step-by-Step: The Angioplasty and Stenting Process
1. Access: You will be sedated but awake. A cardiologist makes a small incision, usually in the wrist (radial artery) or groin (femoral artery).
2. Guiding the Catheter: A long, thin, flexible tube (a catheter) is threaded through the artery to the blocked coronary artery using live X-ray (fluoroscopy) guidance.
3. Injecting Dye: A contrast dye is injected through the catheter, making the blood vessels visible on the X-ray screen (coronary angiogram), revealing the location and severity of the blockages.
4. Angioplasty: A guide wire is moved through the blocked artery. A second catheter with a deflated balloon on its tip is passed over the wire to the blockage. The balloon is inflated, compressing the plaque against the artery walls and widening the artery.
5. Stent Placement: The balloon is deflated and removed. A new balloon catheter with the compressed stent mounted on it is positioned at the site of the blockage. The balloon is inflated again, expanding the stent and locking it into place against the artery wall.
6. Final Check: The balloon is deflated and removed, leaving the stent permanently in place. The catheter is removed, and the access site is closed with pressure or a closure device.
Before the Procedure: Preparation and Planning
Preparation involves blood tests, an electrocardiogram (ECG), and possibly imaging tests. You will likely be asked to fast for several hours before the procedure. It's crucial to inform your doctor of all medications you are taking, especially blood thinners or diabetes drugs. If you are on medication for diabetes, consult your doctor on Apollo24|7 for specific instructions on adjusting your doses before the procedure.
After the Procedure: Recovery in the Hospital
Afterward, you'll be moved to a recovery room for monitoring. Nurses will check your vital signs and the access site for bleeding. You'll need to lie flat for a few hours if the groin was used. Most people stay in the hospital overnight for observation before going home. You will be given clear instructions on your new medications, particularly blood thinners.
Consult Top Specialists
Types of Stents: Choosing the Right One For You
Not all stents are the same. The choice between types depends on your specific condition, the location of the blockage, and your risk factors.
Bare-Metal Stents (BMS): The Original Option
These are simple mesh tubes made of metal without any special coating. They are effective at holding the artery open but have a higher risk of the artery re-narrowing (restenosis) because the metal can irritate the tissue, causing excess scar tissue to grow through the mesh. They are sometimes used in larger arteries or for patients who cannot tolerate long-term dual antiplatelet therapy (DAPT).
Drug-Eluting Stents (DES): The Modern Standard
These are the most commonly used stents today. They are coated with a medication that is slowly released (eluted) over time into the surrounding artery tissue. This drug suppresses the excessive tissue growth that causes restenosis. While tremendously effective at preventing re-narrowing, they require a longer period of DAPT (typically 6-12 months, sometimes more) to prevent the rare but dangerous risk of a blood clot forming on the stent itself (stent thrombosis). The drug eluting stent vs bare metal decision is a key discussion you will have with your cardiologist.
The Future is Here: Bioresorbable Vascular Scaffolds
Also known as dissolving stents, these are the latest innovation. Made from materials that dissolve over time (like polylactic acid, similar to dissolvable stitches), they provide temporary support to the artery until it heals and can stay open on its own, then they disappear. This eliminates a permanent metal implant, restores natural vessel function, and may reduce long-term risks. However, they also require very precise placement and are not suitable for all patients or blockages.
Life After a Stent: Recovery, Medication, and Lifestyle
Getting the stent is just the first step. The real work of recovery and maintaining its benefits happens in the weeks, months, and years that follow.
The Critical Role of Dual Antiplatelet Therapy (DAPT)
This is non-negotiable. After a stent is placed, the body sees it as a foreign object, and blood cells can easily stick to it, forming a dangerous clot. To prevent this, you will be prescribed two types of antiplatelet medications (e.g., Aspirin and Clopidogrel/Ticagrelor). It is absolutely vital to take these medications exactly as prescribed without missing a dose. Stopping them early without your doctor's guidance is the biggest risk factor for stent thrombosis, which can cause a sudden, massive heart attack. If you experience any side effects from these medications, consult a doctor online with Apollo24|7 before making any changes to your regimen.
Cardiac Rehabilitation: Your Path to Stronger Health
Cardiac rehab is a supervised program of exercise, education, and counseling designed to improve your heart health after a procedure. It’s a cornerstone of recovery, proven to reduce the risk of future heart problems, build confidence, and provide support. It helps you safely adopt new diet and exercise habits under medical supervision.
Diet and Exercise: Building Sustainable Habits
The stent fixes a current blockage, but it doesn't cure the underlying disease—atherosclerosis. To protect your other arteries and the one with the stent, lifelong lifestyle changes are essential:
Diet: Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated fats, trans fats, sodium, and sugar.
Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, as approved by your doctor.
Other Changes: Manage stress, quit smoking, and limit alcohol.
Potential Risks and Complications
Like any medical procedure, stenting carries some risks, though serious complications are uncommon.
Short-Term Risks: Bleeding, Artery Damage, and Allergic Reaction
Bleeding or Bruising: At the catheter insertion site.
Blood Vessel Damage: The catheter can scrape or tear the artery.
Allergic Reaction: To the contrast dye used during the angiogram.
Kidney Damage: The contrast dye can affect kidney function, especially in those with pre-existing kidney disease.
Apollo24|7 offers a convenient home collection for tests like serum creatinine to monitor your kidney function before and after the procedure.
Arrhythmia: Irregular heart rhythms during the procedure.
Long-Term Considerations: Restenosis and Stent Thrombosis
Restenosis: When the artery becomes narrowed again inside the stent due to tissue growth. This is less common with DES.
Stent Thrombosis: A blood clot forms inside the stent, which is a medical emergency. This is why adhering to DAPT is so critical.
Quick Takeaways: Key Points to Remember
A stent is a tiny mesh tube that props open narrowed arteries to restore blood flow, most commonly in the heart.
It is placed during a minimally invasive procedure called angioplasty via a catheter, usually through the wrist or groin.
The two main types of stents are bare-metal (BMS) and drug-eluting (DES), with DES being the most common today.
The procedure is a treatment, not a cure. Underlying coronary artery disease must be managed with lifestyle changes.
Dual Antiplatelet Therapy (DAPT) is critical after a stent to prevent blood clots. Never stop these medications without your doctor's approval.
Cardiac rehabilitation is a highly recommended program to ensure a safe and effective recovery.
Attend all follow-up appointments and report any new or worsening symptoms, like chest pain after stent placement, to your doctor immediately.
Conclusion
Understanding stents is a powerful step toward taking control of your heart health. These remarkable devices have revolutionized the treatment of blocked arteries, offering a lifeline during heart attacks and a return to normalcy for those suffering from debilitating angina. However, it's crucial to remember that the stent itself is just one part of the solution. Its long-term success is a partnership between the skilled hands of your medical team and your daily commitment to medication adherence and heart-healthy living. By embracing the necessary lifestyle changes and working closely with your cardiologist, you can protect your new stent and your entire cardiovascular system, paving the way for a
Consult Top Specialists

Dr. Anand Misra
General Physician/ Internal Medicine Specialist
14 Years • MBBS, DNB
Mumbai
Apollo Hospitals CBD Belapur, Mumbai

Dr. Ashmitha Padma
General Physician/ Internal Medicine Specialist
5 Years • MBBS, MD Internal Medicine
Bengaluru
Apollo Hospitals Jayanagar, Bengaluru

Dr. Aakash Garg
Gastroenterology/gi Medicine Specialist
12 Years • MBBS, DNB (Medicine), DrNB (Gastroentrology).
Bilaspur
Apollo Hospitals Seepat Road, Bilaspur
(150+ Patients)

Dr. R Gopakumar
Internal Medicine/ Covid Consultation Specialist
31 Years • MBBS, MD(general medicine
Angamaly
Apollo Hospitals Karukutty, Angamaly
(25+ Patients)

Dr. Kumudha Ravi Munirathnam
General Physician/ Internal Medicine Specialist
18 Years • MBBS, DNB (Int Med.), PGD (Diabetology), MNAMS
Chennai
Apollo Speciality Hospitals OMR, Chennai
(200+ Patients)