Guide to New Generation Pacemakers: What to Know
Discover everything about new generation pacemakers, including leadless and dual-chamber options, MRI safety, cardiac physiologic pacing, remote monitoring, recovery, and lifestyle guidance.

Written by Dr. Mohammed Kamran
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 13th Jan, 2026
Introduction
If you or a loved one has been told you might need a pacemaker, you have likely noticed how quickly the technology has evolved. New generation pacemakers are smaller, smarter, and safer than ever—many are MRI-conditional, some are completely leadless, and most now support remote monitoring through a home hub or smartphone. That means fewer clinic visits, earlier detection of problems, and more confidence returning to daily life.
This guide explains what new generation pacemakers are, who needs them, and how they are implanted and cared for. It explores leadless devices, dual-chamber leadless systems, MRI safety, cardiac physiologic pacing, and remote monitoring. You will also find practical advice on living with a pacemaker—from travel and exercise to airport security and smartphones—plus what to ask your doctor to choose the best device for your needs. Whether you are just starting your research or preparing for a procedure, consider this your up-to-date, plain-language resource on new generation pacemakers.
Pacemakers 101 in 2025: What’s Actually New?
Here's a brief overview of the latest advancements in pacemaker technology:
Pacemakers treat slow or irregular heart rhythms by sending small electrical pulses that keep your heartbeat steady. What has changed in the last decade is how these devices are designed and how they connect with your care team.
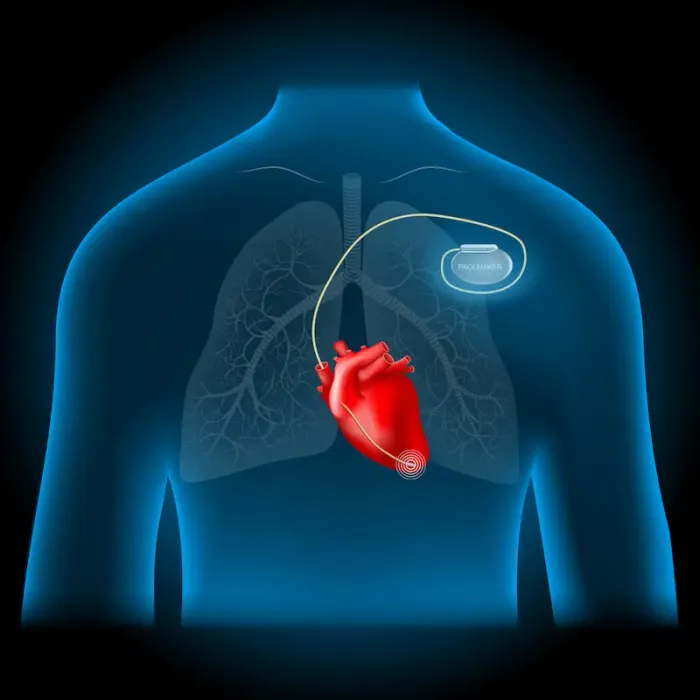
Miniaturisation and leadless options: Traditional systems have a pulse generator placed under the skin with insulated wires (leads) threading into the heart. Today, leadless pacemakers sit entirely inside the heart and are delivered via a catheter from the leg vein—no surgical pocket, no chest scar, and no transvenous leads. Early and mid-term data show fewer lead- and pocket-related complications compared with conventional systems.
MRI-conditional labelling: Many new generation pacemakers are MRI-conditional (some even at 3 Tesla) when scanned under specific protocols, an important shift because over half of device patients will likely need an MRI in their lifetime.
Smarter sensing and communication: Modern devices can adapt rate based on activity, monitor arrhythmias, and transmit updates to your clinic via a home hub or smartphone app. Telemonitoring helps detect issues early and may reduce unplanned visits.Consult Top Specialists
Who Needs a Pacemaker—and When to Consider One
Here's who typically requires pacing support and when to act:
Pacemakers are usually recommended for symptomatic bradycardia causing fainting, fatigue, or dizziness, atrioventricular (AV) block when electrical signals are delayed or blocked, sick sinus syndrome when the heart’s natural pacemaker misfires, and some heart failure patients eligible for cardiac resynchronisation therapy (CRT).
Common symptoms include lightheadedness, fatigue, shortness of breath, and fainting. If these persist beyond two weeks, consult a doctor online or book an in-person appointment if you experience fainting or chest pain. Pre-implant evaluation often includes ECG, echocardiogram, and sometimes extended rhythm monitoring.
The New Landscape: Types of New Generation Pacemakers
Here's a breakdown of modern pacemaker types and their benefits:
Leadless pacemakers: Self-contained capsules implanted directly in the heart via a leg vein, eliminating surgical pockets and transvenous leads. Recent advances include dual-chamber leadless systems, expanding options for patients needing coordinated pacing of both chambers.
MRI-conditional and 3T-ready systems: Devices labelled MRI-conditional allow safe imaging under specific protocols. This is important as many patients will require MRI during the device lifespan.
Cardiac physiologic pacing: His-bundle pacing and left bundle branch area pacing activate the heart’s native conduction system, promoting natural contraction and reducing the risk of pacing-induced cardiomyopathy.
CRT and multipoint pacing: For heart failure patients with dyssynchrony, CRT improves symptoms and outcomes. Multipoint pacing stimulates multiple sites in the left ventricle, enhancing response in select cases.
Smart sensors and remote monitoring: Rate-adaptive sensors learn activity patterns. Bluetooth or proprietary wireless technologies transmit device health, battery status, and rhythm episodes to the clinic, allowing early detection and timely care.
The Implant Journey: Before, During, and After
Here's what to expect throughout the pacemaker implantation process:
Pre-procedure planning: Review symptoms, rhythm reports, imaging, and device options. Discuss MRI needs, vein size, and cosmetic preferences. Blood tests and chest imaging may be ordered.
During the procedure: Leadless pacemakers are implanted via a small puncture in the groin vein using a catheter. Transvenous pacemakers involve creating a chest pocket and threading leads into the heart. Both procedures usually involve local anaesthesia with sedation.
Recovery and early care: Leadless devices require a small groin bandage, while pocket-based devices require incision care and limited arm movement. Patients typically receive a device ID card, remote monitoring setup, and instructions for follow-up checks.
Safety and Risks: What the Latest Data Shows
Here's an overview of complications and safety measures:
Leadless pacemakers reduce pocket and lead-related complications such as fracture, displacement, and haematomas. Infection prevention is key; antibacterial envelopes can reduce major device infections in higher-risk patients. MRI-conditional labelling allows safe scanning when protocols are followed. Remote monitoring adds safety by detecting issues early and reducing emergency visits.Consult Top Specialists
Battery, Replacements, and Upgrades
Here's what you need to know about pacemaker longevity and maintenance:
Battery life typically spans 8–15 years, influenced by pacing burden and programming. Replacement for transvenous systems involves exchanging the generator, while leadless devices may be retrieved or implanted alongside old devices. Upgrades to CRT or physiologic pacing may be considered if clinical needs evolve.
Living Well with New Generation Pacemakers
Here's guidance for day-to-day life with a pacemaker:
Exercise and activity: Resume normal activities after healing. Leadless implants avoid chest pockets, which can benefit athletes.
Travel and airport security: Carry your device card, walk through metal detectors normally, and inform staff if hand wands are used.
Smartphones, wearables, and EMI: Keep strong magnets away from the device site. Bluetooth and Wi-Fi are generally safe. Remote monitoring apps transmit data automatically.
MRI and medical/dental procedures: MRI-conditional devices are safe under protocol. Always inform clinicians about your device.
Cybersecurity: Keep apps and phones updated and use strong passwords.
Remote Follow-Up: How App-Based Monitoring Works
Here's how remote monitoring supports your care:
Device diagnostics, battery trends, lead performance, and rhythm episodes are transmitted to your clinic. Alerts prompt timely intervention. After the initial post-implant check, visits may be remote every 3–6 months, with at least annual in-person reviews.
Cost, Coverage, and Access
Here's what affects pacemaker affordability and availability:
Costs depend on device type, hospital setting, and additional tools such as antibacterial envelopes. Most medically indicated pacemakers are covered by insurance. Leadless and MRI-conditional devices are increasingly available in major centres. Consult your cardiologist and insurer for specifics.
Questions to Ask Your Cardiologist
• Am I a candidate for leadless or MRI-conditional systems?
• Could conduction system pacing or CRT improve my outcomes?
• How long is my expected battery life and what happens at replacement?
• What is my remote monitoring plan?
• Are there activity restrictions?
• How will future MRI scans be handled?
• What is my estimated recovery timeline?
Special Situations
Children and congenital heart disease: Pacing may prioritise growth-friendly routes. Leadless pacing in children is evolving.
Pregnancy: Coordination among obstetrics, cardiology, and anaesthesia is important. MRI needs and delivery planning should be reviewed.
End-of-life and device deactivation: Pacemakers do not restart the heart after non-rhythm death. Discuss advance directives and deactivation preferences with your clinician.
The Future: Biological Pacemakers, Energy Harvesting, and AI
Here's what lies ahead in pacing technology:
Biological pacemakers aim to restore natural rhythm using cells or gene therapy. Energy harvesting could extend battery life. AI may optimise programming and personalise follow-up schedules. Current new generation devices already offer MRI access, fewer complications, and seamless remote care.
Conclusion
Pacemaker technology has advanced quickly—and that’s good news for patients. New generation pacemakers are smaller, smarter, and more adaptable, whether that means a fully leadless device, an MRI-conditional system, or pacing strategies that better mimic the heart’s natural activation. The result is fewer complications in eligible patients, faster recovery for many, and an easier long-term care experience thanks to remote monitoring. For those living with heart failure, CRT options continue to evolve, and for patients who need dual-chamber pacing, leadless systems have reached an important milestone with FDA approval.
Choosing the right pacemaker isn’t about labels; it’s about fit. Your medical history, expected MRI needs, activity goals, and risk profile all shape the best choice. Ask your cardiologist about leadless eligibility, conduction system pacing, and how remote monitoring will be handled day-to-day. If you’re unsure or want a second opinion, consult a doctor online with Apollo24|7. They can help plan pre-op testing (including home collection for labs), coordinate with a specialist, and clarify timing and recovery.
The bottom line: new generation pacemakers expand what’s possible—safer procedures, more flexible imaging, and a connected care experience. With the right device and follow-up plan, most people return to active, confident lives.Consult Top Specialists
Consult Top Specialists
Dr. Praveen Jaiswal
Cardiologist
17 Years • MD(Medicine), DM(Cardiology)
Indore
Apollo Hospitals Vijay Nagar, Indore

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Ranga Manikandan
Cardiologist
6 Years • MBBS., MD., DM.DNB - Cardiology
Madurai
Apollo Speciality Hospitals KK Nagar, Madurai

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult Top Specialists
Dr. Praveen Jaiswal
Cardiologist
17 Years • MD(Medicine), DM(Cardiology)
Indore
Apollo Hospitals Vijay Nagar, Indore

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Ranga Manikandan
Cardiologist
6 Years • MBBS., MD., DM.DNB - Cardiology
Madurai
Apollo Speciality Hospitals KK Nagar, Madurai

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
Consult Top Specialists
Dr. Praveen Jaiswal
Cardiologist
17 Years • MD(Medicine), DM(Cardiology)
Indore
Apollo Hospitals Vijay Nagar, Indore

Dr. Bhethala Sharan Prakash
General Physician/ Internal Medicine Specialist
5 Years • MBBS MD
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr. Sushith C
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru

Dr Ranga Manikandan
Cardiologist
6 Years • MBBS., MD., DM.DNB - Cardiology
Madurai
Apollo Speciality Hospitals KK Nagar, Madurai

Dr. Anand Ravi
General Physician
2 Years • MBBS
Bengaluru
PRESTIGE SHANTHINIKETAN - SOCIETY CLINIC, Bengaluru
More articles from Heart disease
Frequently Asked Questions
1) Is a leadless pacemaker better than a traditional one?
Leadless pacemakers can reduce lead- and pocket-related complications and leave no chest scar. However, not everyone is a candidate. Dual-chamber leadless options are now available for select patients. Discuss with your cardiologist which option best suits your needs.
2) Can I get an MRI with a pacemaker?
Many new generation pacemakers are MRI-conditional (some even at 3 Tesla) and can be scanned safely under specific protocols. Always inform your imaging team about your device before the scan.
3) How long does a pacemaker battery last?
Pacemaker batteries typically last 8–15 years, depending on pacing needs and device settings. Your clinic monitors battery status and schedules replacement in advance to ensure uninterrupted support.
4) Will airport security harm my pacemaker?
It is generally safe. Carry your device card, walk through metal detectors normally, and inform staff if hand wands are used. Avoid lingering near strong magnets.
5) How often will I need checkups?
After the initial healing period, many follow-ups can be conducted remotely every 3–6 months, with at least one in-person clinic visit each year. Seek urgent care if new or severe symptoms arise.