What Leads To Signs Of Prolapsed Hemorrhoids Signs And
Learn about prolapsed haemorrhoids, including their signs, symptoms, and causes. Understand how to identify this condition and explore treatment options.

Written by Dr. Siri Nallapu
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
A prolapsed haemorrhoid can be an uncomfortable, painful, and worrying condition. If you've noticed a soft bulge or lump protruding from your anus, especially after a bowel movement, you might be experiencing this common issue. But what exactly causes a haemorrhoid to prolapse, and how can you tell if that's what you're dealing with? This guide will walk you through the key signs of prolapsed haemorrhoids, delve into the root causes, and outline both at-home and medical solutions to help you find relief. Understanding the "why" behind your symptoms is the first step toward effective management and recovery.
What Are Prolapsed Haemorrhoids? Understanding the Basics
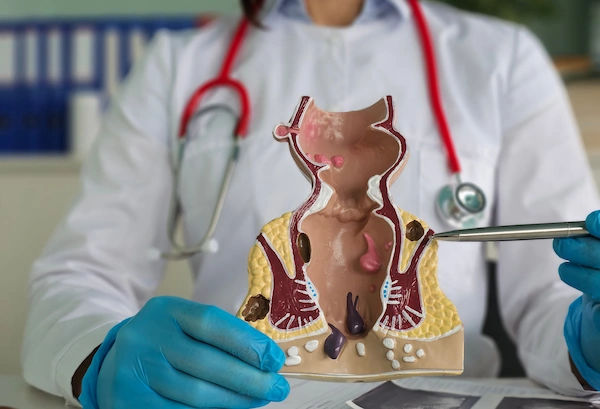
To understand a prolapsed haemorrhoid, it's helpful to first know about haemorrhoids in general. Haemorrhoids are simply cushions of swollen veins and tissue located in the lower rectum and anus. Everyone has them; they only become a problem when they become inflamed, enlarged, or symptomatic.
There are two main types:
- Internal Haemorrhoids: These lie inside the rectum and are usually not visible or painful, as that area lacks pain-sensing nerves.
- External Haemorrhoids: These form under the skin around the anus and can be painful when swollen.
A prolapsed haemorrhoid is specifically an internal haemorrhoid that has become so swollen and enlarged that it stretches and pushes (prolapses) outside the anal opening. This is a common progression of grade III or IV internal haemorrhoids.
The Four Grades of Internal Haemorrhoids
Medical professionals classify internal haemorrhoids into four grades based on the degree of prolapse:
Grade I: No prolapse. Just enlarged blood vessels.
Grade II: Prolapse during straining but reduce (retract back inside) spontaneously.
Grade III: Prolapse during straining and require manual reduction (pushing them back in manually).
Grade IV: Permanently prolapsed and cannot be manually reduced.
Key Signs and Symptoms of a Prolapsed Haemorrhoid
Recognizing the signs is crucial for seeking appropriate treatment. The symptoms of a prolapsed pile can vary from mild annoyance to significant discomfort.
Primary Indicators and Sensations
The most common signs include:
- A Visible Lump or Bulge: The hallmark sign. You may feel or see one or more soft, grape-like lumps protruding from the anus. They are often pinker or redder than the surrounding skin.
- Discomfort and Aching: Unlike the sharp pain of a thrombosed external haemorrhoid, a prolapsed internal one often causes a feeling of fullness, pressure, or a dull ache in the anal region.
- Itching and Irritation (Pruritus Ani): Mucus from the displaced tissue can moisten the anal area, leading to significant itching and skin irritation.
- Bright Red Bleeding: You may notice streaks of bright red blood on the toilet paper, in the toilet bowl, or on the surface of the stool. This is caused by the delicate surface of the haemorrhoid being scratched during wiping or a bowel movement.
- Difficulty Cleaning: The protruding tissue can make it challenging to clean the anal area effectively after a bowel movement, which can exacerbate irritation.
When to Be Concerned: Severity of Symptoms
While common, some symptoms warrant immediate medical attention. If you experience persistent bleeding that leads to lightheadedness, dizziness, or fainting, or if you have severe pain (which may indicate a thrombosed or strangulated haemorrhoid), you should consult a doctor promptly.
What Leads to a Prolapsed Haemorrhoid? The Root Causes
Prolapsed haemorrhoids don't appear out of nowhere. They are the result of increased pressure in the lower rectum, which causes the vascular cushions to swell and eventually prolapse. Several key factors contribute to this pressure build-up.
Chronic Constipation and Straining
This is the number one culprit. When you are constipated, stools become hard and dry, making them difficult to pass. The intense straining and prolonged sitting on the toilet significantly increases abdominal pressure, forcing blood to engorge the haemorrhoidal veins. Over time, this repeated pressure stretches the supportive tissues, allowing the haemorrhoid to prolapse.
Pregnancy and Childbirth
Pregnancy is a major risk factor for developing symptomatic haemorrhoids during pregnancy. The growing uterus places direct pressure on the pelvic veins and the inferior vena cava (a large vein on the right side of the body), slowing blood return from the lower half and causing veins below the uterus to become engorged and swollen. The intense straining during the second stage of labor can then cause existing haemorrhoids to prolapse or new ones to form.
Lifestyle and Dietary Factors
A low-fibre diet is a primary driver of constipation. Without adequate fibre, stools are not bulky and soft, leading to the straining mentioned above. Furthermore, a sedentary lifestyle or prolonged sitting on the toilet (often due to habits like using a phone) keeps constant pressure on the anal veins, contributing to their weakening and prolapse.
Other Contributing Conditions and Habits
- Chronic Diarrhoea: Constant irritation and frequent bowel movements can also inflame and strain the anal region.
- Heavy Lifting: Regularly lifting heavy objects, especially while holding your breath (the Valsalva maneuver), creates a
massive surge in intra-abdominal pressure, similar to straining. - Obesity: Excess weight, particularly around the abdomen, increases pressure on the pelvic veins.
- Ageing: The supportive connective tissues in the rectum and anus naturally weaken with age, making prolapse more
likely. - Genetic Predisposition: Some people may inherit a weaker vein structure in the anal region.
Diagnosing a Prolapsed Haemorrhoid: What to Expect
If you suspect you have a prolapsed haemorrhoid, a proper diagnosis is essential. A doctor can confirm it and rule out other, more serious conditions like anal fissures, abscesses, or in rare cases, colorectal cancer.
The Physical Examination
A doctor will typically start with a visual inspection of the anal area. For a prolapsed haemorrhoid, the diagnosis is often visual, the haemorrhoid is visible around the anal opening. They may ask you to strain as if having a bowel movement to see the extent of the prolapse.
Digital Rectal Exam (DRE) and Anoscopy
To evaluate internal structures, the doctor will likely perform a digital rectal exam, gently inserting a gloved, lubricated finger into the rectum to feel for abnormalities. For a clearer view, they might use an anoscope, a short, lighted tube that allows them to see the anal canal and lower rectum in detail. This is a quick, in-office procedure that provides a definitive diagnosis.
Effective Treatment Options for Prolapsed Piles
Treatment depends on the grade of the haemorrhoid, the severity of symptoms, and its impact on your quality of life.
At-Home Care and Conservative Management (Grades I & II)
For mild to moderate cases, non-invasive approaches are the first line of defense:
- Warm Sitz Baths: Soaking the anal area in warm water for 15-20 minutes, 2-3 times a day, can reduce swelling and provide significant pain relief.
- Dietary Modifications: Increase your intake of high-fibre foods (fruits, vegetables, whole grains) and water. This softens
stools and makes them easier to pass, eliminating the need to strain. - Topical Treatments: Over-the-counter creams, ointments, or suppositories containing hydrocortisone or witch hazel can
temporarily relieve itching and pain. - Proper Hygiene: Gently clean the area with water after bowel movements and pat dry instead of wiping harshly.
Non-Surgical Medical Procedures (Grades II & III)
If conservative measures fail, a doctor can perform minimally invasive procedures in a clinic:
- Rubber Band Ligation: The most common procedure. A small rubber band is placed around the base of the
haemorrhoid, cutting off its blood supply. Within a week, the haemorrhoid shrivels and falls off. - Sclerotherapy: A chemical solution is injected into the haemorrhoid tissue, causing it to shrink.
- Infrared Coagulation (IRC): Infrared light is used to coagulate the blood vessels feeding the haemorrhoid, causing it to
shrink and recede.
Surgical Interventions (Grade IV or Severe Cases)
For large, persistent, or strangulated haemorrhoids, surgery may be necessary:
- Haemorrhoidectomy: The surgical removal of the haemorrhoid. It is the most effective but also has the most painful recovery.
- Haemorrhoidopexy (Stapling): A procedure that blocks blood flow to the haemorrhoidal tissue and staples the prolapsed tissue back into its normal position. Recovery is typically less painful than a haemorrhoidectomy.
If your prolapsed haemorrhoid is causing persistent pain or bleeding that doesn't improve with home care after a week or two, it's crucial to consult a doctor.
Can You Prevent Haemorrhoids from Prolapsing?
Absolutely. Prevention is centered on reducing pressure and strain in the rectal area.
- Eat a High-Fibre Diet: Aim for 25-30 grams of fibre daily to keep stools soft.
- Stay Hydrated: Drink plenty of water throughout the day to aid digestion.
- Exercise Regularly: Physical activity helps prevent constipation and reduces pressure caused by prolonged sitting.
- Avoid Straining and Prolonged Toilet Sitting: Go when you feel the urge, don't linger on the toilet for more than
necessary, and avoid straining. - Practice Proper Lifting Technique: Exhale while lifting the weight; never hold your breath.
Conclusion: Taking Control of Your Rectal Health
Dealing with a prolapsed haemorrhoid can be an embarrassing and painful experience, but it's an incredibly common one that millions of people manage successfully. The key is to understand the signs, like a visible bulge, discomfort, and bleeding, and recognize the primary causes, such as chronic constipation, straining, and lifestyle factors. By adopting a high-fibre diet, staying hydrated, and avoiding habits that increase abdominal pressure, you can often prevent them from occurring or recurring. For existing issues, a range of effective treatments exists, from simple sitz baths to minor medical procedures. Remember, there's no need to suffer in silence. If your symptoms are severe or persistent, seeking professional medical advice is a proactive step toward lasting relief and improved quality of life.
Consult a General Physician for the best advice
Consult a General Physician for the best advice

Dr. Khuda Baksh Nagur
General Physician/ Internal Medicine Specialist
11 Years • MBBS, MD (GENERAL MEDICINE), Certificate Programme clinicians in Diabetes Management
Bengaluru
Medwin multispeciality clinic, Bengaluru
(25+ Patients)

Dr. Tanzeem Shajahan
General Physician/ Internal Medicine Specialist
7 Years • MBBS, MD (General Medicine)
Bengaluru
Medwin multispeciality clinic, Bengaluru

Dr. Soumen Paul
General Physician/ Internal Medicine Specialist
24 Years • MBBS
Kolkata
MCR SUPER SPECIALITY POLY CLINIC & PATHOLOGY, Kolkata
(50+ Patients)

Dr. Imtiyaz Khan
General Physician/ Internal Medicine Specialist
6 Years • MBBS
Bengaluru
Apollo Clinic, Sarjapur Road, Bengaluru

Dr. Shiv Krishna Mitra
General Practitioner
15 Years • MBBS GEN. MED. PGDRM, MCH
Kolkata
Samaritan Clinic, Kolkata
More articles from hemorrhoids
Frequently Asked Questions
1. Can a prolapsed haemorrhoid go away on its own?
Grade II prolapsed haemorrhoids that reduce on their own may improve with conservative care. However, Grade III and IV prolapsed haemorrhoids that require manual reduction or are permanently prolapsed are unlikely to resolve completely without medical intervention.
2. Is it safe to push a prolapsed haemorrhoid back in?
For a Grade III haemorrhoid, it is generally safe and recommended to gently push it back inside the anal canal with a lubricated finger. This can provide relief from discomfort. However, if it is very painful or won't go back in (Grade IV), do not force it and consult a doctor.
3. What is the difference between a prolapsed haemorrhoid and a thrombosed haemorrhoid?
A prolapsed haemorrhoid is an internal haemorrhoid that has slipped out. A thrombosed haemorrhoid is an external haemorrhoid where a blood clot has formed inside it, causing severe, sharp pain and a hard, bluish lump. A haemorrhoid can be both prolapsed and thrombosed.
4. How long does it take for a prolapsed haemorrhoid to heal?
With conservative treatment like sitz baths and diet changes, symptoms can improve within a few days to a week. After procedures like rubber band ligation, it takes 1-2 weeks for the haemorrhoid to fall off. Surgical recovery can take several weeks.
5. Can prolapsed haemorrhoids be a sign of cancer?
While haemorrhoids are common and rarely serious, rectal bleeding can sometimes be a symptom of colorectal cancer. This is why it's important to have any persistent rectal bleeding evaluated by a doctor to rule out more serious conditions.