Finding the Best Hydrocephalus Treatment, A Modern Guide.
Explore modern hydrocephalus treatments, including shunt systems, ETV, and ETV+CPC. Learn symptoms, diagnosis methods, long-term care, and how to choose the best treatment option for infants, adults, and seniors.

Written by Dr. Siri Nallapu
Reviewed by Dr. Shaik Abdul Kalam MD (Physician)
Last updated on 13th Jan, 2026

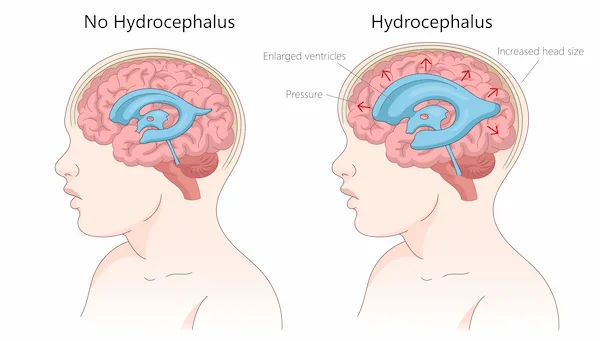
Receiving a hydrocephalus diagnosis for yourself or a loved one can feel overwhelming. Often called "water on the brain," this complex condition involves an accumulation of cerebrospinal fluid (CSF) within the brain's ventricles, leading to increased pressure and potential damage. The immediate and crucial question becomes: what is the best hydrocephalus treatment? The answer isn't one-size-fits-all; it depends on the type of hydrocephalus, the patient's age, and the underlying cause. This guide cuts through the confusion to provide a clear, modern overview of the most effective treatment pathways. We will explore the two primary surgical interventions, shunt systems and endoscopic third ventriculostomy (ETV), break down their pros and cons, and discuss what life looks like after treatment. Our goal is to empower you with knowledge, helping you engage in informed conversations with healthcare professionals about the best treatment plan for your specific situation.
What is Hydrocephalus? Beyond "Water on the Brain"
Hydrocephalus is more than just an excess of fluid; it's a disruption of the delicate ecosystem that protects our brain. Understanding this is key to understanding its treatment.
The Cerebrospinal Fluid (CSF) System Explained
Cerebrospinal fluid is a clear, nourishing liquid that constantly flows around the brain and spinal cord, acting as a shock absorber, delivering nutrients, and removing waste. This fluid is produced within the brain's ventricles (hollow chambers) and is eventually absorbed into the bloodstream. Hydrocephalus occurs when this cycle is interrupted—either because too much fluid is produced, its flow is blocked, or it isn't absorbed properly.
Types of Hydrocephalus; Congenital vs. Acquired
Congenital Hydrocephalus: Present at birth, often due to genetic conditions or developmental disorders like spina bifida.
Acquired Hydrocephalus: Develops after birth from injury or illness, such as a head trauma, brain tumor, stroke, or infection like meningitis.
Normal Pressure Hydrocephalus (NPH): A specific type that occurs in older adults, where ventricles enlarge but pressure may be intermittently normal. It's famously characterized by a triad of symptoms: gait disturbance (trouble walking), dementia, and urinary incontinence.
Recognizing the Signs; Symptoms of Hydrocephalus Across Ages
Symptoms vary dramatically based on age, which is why awareness is critical for early diagnosis and seeking the best treatment.
Symptoms in Infants and Babies
Unusually large or rapidly increasing head circumference
A bulging or tense soft spot (fontanel) on the head
Prominent scalp veins
Downward gaze of the eyes ("sunsetting eyes")
Vomiting, sleepiness, and irritability
Symptoms in Children and Adults
Headaches (often severe and upon waking)
Nausea and vomiting
Blurred or double vision
Problems with balance, coordination, and walking
Lethargy, drowsiness, and cognitive decline
Urinary incontinence
Symptoms in Older Adults (Normal Pressure Hydrocephalus)
The classic NPH triad is:
1. Gait Disturbance: A shuffling, wide-based walk, feeling "glued to the floor."
2. Cognitive Impairment: Slowed thinking, forgetfulness, and apathy.
3. Urinary Incontinence: A loss of bladder control, often occurring later.
How is Hydrocephalus Diagnosed?
A timely and accurate diagnosis is the first step toward effective treatment. If symptoms in adults or infants suggest hydrocephalus, a doctor will perform a neurological exam and likely recommend imaging.
The Role of Imaging: Ultrasound, CT, and MRI Scans
Ultrasound: Often used for infants whose fontanels are still open. It's a quick, radiation-free initial screening tool.
CT Scan (Computed Tomography): Provides detailed cross-sectional images of the brain quickly, making it excellent for emergency diagnosis to confirm ventricular enlargement.
MRI Scan (Magnetic Resonance Imaging): Offers the most detailed images of brain structures. It's crucial for determining the cause of the hydrocephalus (e.g., a blockage) and for planning surgery, especially for procedures like ETV. If your doctor recommends further imaging to monitor your condition, consulting a neurologist via Apollo24|7 can help you understand the next steps.
Exploring the Best Hydrocephalus Treatment Options
There is no effective long-term medication for hydrocephalus; surgery is the only definitive treatment for normal pressure hydrocephalus and other types. The goal of all procedures is to divert the excess CSF to another area of the body where it can be absorbed.
Consult a Specialist for Personalised Advice
Shunt Systems; The Gold Standard
A shunt is a flexible tube and valve system that has been the cornerstone of hydrocephalus treatment for decades.
Components of a Shunt: How It Works: The system is implanted under the skin. A catheter is placed inside a ventricle in the brain, a valve regulates the flow of CSF, and a drainage catheter is tunneled to another body cavity, most commonly the abdomen (ventriculoperitoneal or VP shunt). The shunt continuously drains excess fluid.
Potential Shunt Complications and Malfunction: Shunts are life-saving but mechanical devices. They can fail due to infection, blockage, or breakage. Recognizing symptoms of shunt malfunction, a return of the original hydrocephalus symptoms like severe headache, vomiting, and drowsiness, is a critical part of long-term care. This constitutes a medical emergency.
Endoscopic Third Ventriculostomy (ETV): A Shunt-Free Alternative
ETV is a minimally invasive procedure that creates a new pathway for CSF to flow out of the blocked ventricles, bypassing the need for a shunt.
Is ETV the Right Procedure for You? The neurosurgeon uses a small camera (endoscope) to make a hole in the floor of the third ventricle. Success depends heavily on the cause of the hydrocephalus.
It is most successful in older children and adults with specific types of blockages (e.g., aqueductal stenosis). A key advantage is that it eliminates the risks associated with a lifelong implanted device.
ETV with Choroid Plexus Cauterization (CPC)
Often used in combination with ETV for infants, CPC involves cauterizing (burning) the tissue in the ventricles that produces CSF, thereby reducing the amount of fluid made. The combination of ETV+CPC can improve success rates in certain pediatric cases.
Making the Choice: Shunt vs. ETV
So, which is the best treatment? It's a strategic decision made by a multidisciplinary team led by a skilled neurosurgeon.
Factors Your Neurosurgeon Will Consider
Cause of Hydrocephalus: ETV is only an option if there is a specific type of blockage.
Patient Age: ETV success rates are generally higher in patients over six months old.
Anatomy: The patient's brain anatomy must be suitable for the ETV procedure.
Surgeon Experience: The expertise of the surgical team is a significant factor.
Risk Profile: The team will weigh the immediate surgical risks of ETV against the long-term risk of shunt failure.
Recent studies show that in appropriate candidates, ETV can have a long-term success rate of over 60-70%, while shunts have a very high initial success rate but a significant failure rate over time (approximately 40-50% of shunts fail within the first two years).
Life After Surgery; Long-Term Management and Care
Treatment doesn't end with surgery. Hydrocephalus is often a lifelong condition requiring vigilant management.
Monitoring for Shunt Failure Symptoms
For those with a shunt, patients and caregivers must be experts at recognizing the signs of malfunction, which are often the same as the original hydrocephalus symptoms. Any sudden, severe headache, vomiting, or change in consciousness requires immediate medical attention.
The Importance of Ongoing Neurological Care
Regular follow-ups with a neurologist or neurosurgeon are essential, even if feeling well. These check-ups may include periodic imaging to ensure the best treatment continues to work effectively. Managing a chronic neurological condition like hydrocephalus requires consistent care. Platforms like Apollo24|7 make it easier to schedule regular online consultations with specialists to monitor your progress and manage any new symptoms.
Conclusion
Navigating the path to the best hydrocephalus treatment is a journey that blends advanced medical science with personalized care. While the diagnosis can be daunting, modern neurosurgical techniques like shunts and ETV offer effective ways to manage the condition and allow individuals to lead full, active lives. The core of successful management lies in understanding your specific diagnosis, being an active participant in your treatment decisions with your medical team, and committing to vigilant, long-term follow-up care. Remember, you are not alone. A strong support system of family, friends, and healthcare professionals is your greatest asset. If you or a loved one are experiencing symptoms, take the first step today by consulting a specialist to get a clear diagnosis and discuss the treatment options that are right for you.
Consult a Specialist for Personalised Advice
Consult a Specialist for Personalised Advice

Dr. Rajib Ghose
General Physician/ Internal Medicine Specialist
25 Years • MBBS
East Midnapore
VIVEKANANDA SEBA SADAN, East Midnapore

Dr. Sriya Mukherjee
General Practitioner
10 Years • MBBS
Kolkata
SEVA POLYCLINIC, Kolkata

Dr. Rajesh R
General Practitioner
24 Years • MBBS
Bengaluru
Maruti Polyclinic and dental care, Bengaluru

Dr. Ashita Kuruvilla
General Practitioner
7 Years • MBBS
Kolkata
KVC CLINIC, Kolkata

Dr Churchil Gupta
General Practitioner
2 Years • MBBS
Greater Noida
Vedant Clinic, Greater Noida
More articles from Hydrocephalus
Frequently Asked Questions
Q1. Can hydrocephalus be treated without surgery?
No, there are no medications that can cure hydrocephalus. Surgery to divert the cerebrospinal fluid (either with a shunt or an ETV) is the only effective long-term treatment. Medications may be used temporarily to reduce fluid production before surgery.
Q2. What is the life expectancy for someone with a shunt?
With successful treatment and proper management, most people with hydrocephalus can have a normal life expectancy. The shunt itself does not limit lifespan; however, the underlying cause of the hydrocephalus and the vigilant management of potential shunt complications are the key factors.
Q3. How often do shunts need to be replaced?
There is no set schedule. A shunt can last a few years, decades, or even a lifetime. They are only replaced if they malfunction due to a blockage, infection, or breakage. Many people require multiple revisions over their lifetime.
Q4. What are the first signs of a shunt malfunction?
The first signs often mirror the original symptoms of hydrocephalus: severe headache (especially upon waking), nausea/vomiting, drowsiness, vision problems, and irritability (in children). This is a medical emergency requiring immediate attention.
Q5. Is normal pressure hydrocephalus (NPH) reversible?
Yes, to a significant degree, especially if diagnosed and treated early. Surgery (often with a shunt) can lead to dramatic improvement in walking, cognitive function, and bladder control. The earlier the treatment, the better the potential outcome.