Guide to Hypothyroidism During Pregnancy
Explore how hypothyroidism affects pregnancy, including symptoms, risks to mother and baby, and treatment options. Learn the importance of early diagnosis and thyroid management for a healthy pregnancy journey.

Written by Dr. Rohinipriyanka Pondugula
Reviewed by Dr. M L Ezhilarasan MBBS
Last updated on 13th Jan, 2026
Congratulations on your pregnancy! This is a time of incredible change and excitement. If you've been diagnosed with hypothyroidism (an underactive thyroid) or are learning about it now, you might be feeling a mix of joy and concern. You're not alone, and the most important thing to know is that with proper management, you can have a perfectly healthy pregnancy and baby. Hypothyroidism during pregnancy is a common condition where your thyroid gland doesn't produce enough crucial hormones. These hormones are vital not just for your metabolism and energy but are absolutely essential for your baby's brain development and growth, especially in the first trimester when their own thyroid hasn't formed yet. This guide will walk you through everything—from understanding causes and symptoms to navigating safe treatment and monitoring. We'll empower you with knowledge so you can confidently partner with your healthcare team for a smooth and healthy journey.
What is Hypothyroidism and Why Does it Matter in Pregnancy?
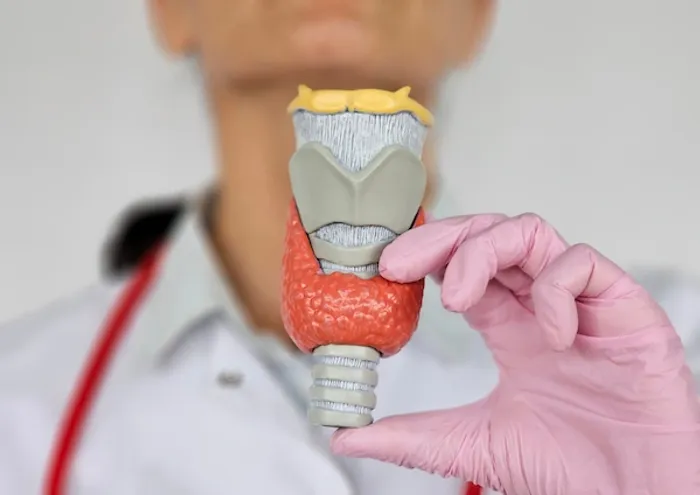
Hypothyroidism is a condition where the butterfly-shaped thyroid gland in your neck fails to produce sufficient thyroid hormones, primarily Thyroxine (T4). While this condition requires management at any stage of life, its importance is magnified tenfold during pregnancy.
The Role of Thyroid Hormones in Your Body and Your Baby's Development
Think of thyroid hormones as the master regulators of your body's metabolism. During pregnancy, their job description expands dramatically. In the critical first 12 weeks, your baby is entirely dependent on your thyroid hormones for neurological development, including the formation of the brain and nervous system. Even after the baby's thyroid begins to function on its own around week 12, it still relies on you for a supply of iodine, which is a key building block for thyroid hormones. Untreated or poorly managed hypothyroidism and miscarriage risk are unfortunately linked, but also associated with risks of preterm birth, low birth weight, and preeclampsia for the mother.
What Causes Hypothyroidism When You're Expecting?
Understanding the cause helps tailor your treatment plan. The vast majority of cases have a specific autoimmune origin.
Hashimoto's Thyroiditis: The Most Common Culprit
In up to 90% of cases, the reason for an underactive thyroid is Hashimoto's disease. This is an autoimmune disorder where your body's immune system mistakenly attacks and slowly destroys your thyroid gland, impairing its ability to produce hormones. If you had Hashimoto's before pregnancy, you'll need close monitoring, as your medication needs will almost certainly increase.
Other Potential Causes of Low Thyroid Function
Other causes include previous surgical removal of the thyroid (due to cancer or nodules), radioactive iodine treatment, or certain medications. Some women may also have been borderline hypothyroid before conception, and the increased demands of pregnancy push them into a full-blown deficiency. A less common cause worldwide, though still significant, is severe iodine deficiency, which is why prenatal vitamins contain iodine.
Symptoms of Hypothyroidism in Pregnancy
This can be tricky, as many symptoms of underactive thyroid in pregnancy mimic the common discomforts of pregnancy itself. This is why testing, not just symptom-spotting, is crucial.
Common Symptoms Often Mistaken for Normal Pregnancy Discomfort
- Extreme fatigue and sluggishness
- Unexplained weight gain
- Feeling unusually cold
- Muscle cramps and aches
- Constipation
- Dry skin and hair
When to Be Concerned?
While the above can be normal, a combination of several severe symptoms, especially if they include a noticeably enlarged thyroid (goiter), severe brain fog, a hoarse voice, or a significantly slowed heart rate, warrants immediate discussion with your doctor.
The Importance of Diagnosis
Diagnosis is not based on symptoms alone; it requires a simple blood test. If your condition does not improve after trying rest and diet changes, or if you have a known history, consulting a doctor is essential. Apollo24|7 offers convenient home collection for tests like thyroid function panels, making it easier to get tested from the comfort of your home.
Understanding TSH, T4, and T3 Tests and Pregnancy-Specific Ranges
The primary test is for Thyroid-Stimulating Hormone (TSH). This is a pituitary hormone that tells your thyroid to work. If your thyroid is underactive, your pituitary gland "shouts" louder, sending out more TSH. Therefore, a high TSH level indicates hypothyroidism. Doctors also often measure Free T4 (the active thyroid hormone). It's vital to know that normal TSH levels in first trimester and beyond are different—and stricter—than non-pregnancy ranges. Generally, TSH should be kept below 2.5 mIU/L in the first trimester and below 3.0 mIU/L in the second and third trimesters.
Who Should Be Screened and When?
The American College of Obstetricians and Gynecologists (ACOG) recommends screening women with a personal or family history of thyroid disease or symptoms at the first prenatal visit. Many endocrinologists advocate for universal screening given the high prevalence and serious consequences of missing a diagnosis. If you are planning a pregnancy and have concerns, getting a thyroid function test beforehand is ideal.
Potential Risks: For the Mother and the Developing Baby
Left unmanaged, hypothyroidism poses significant risks. This underscores why treatment is so effective and important—it mitigates these risks almost entirely.
Risks to the Mother's Health
For the mother, uncontrolled hypothyroidism increases the chance of:
- Preeclampsia: A serious condition characterized by high blood pressure.
- Anaemia: A lack of healthy red blood cells.
- Postpartum hemorrhage: Excessive bleeding after delivery.
- Gestational diabetes: Though the link is still being studied.
Risks to the Baby's Development
For the baby, the most significant risk is impaired neurodevelopment, which can affect IQ and cognitive function later in life. Other risks include:
- Preterm birth.
- Low birth weight.
- In rare, severe cases, congenital cretinism (which involves severe developmental delays and dwarfism).
Consult Top Specialists
Safe and Effective Treatment
The good news is that treatment is straightforward, highly effective, and safe for both you and your baby.
Levothyroxine: The Gold Standard Medication
The treatment is a synthetic form of the T4 hormone, called Levothyroxine (brand names include Synthroid, Levoxyl, Eltroxin). It is identical to the hormone your body makes and is completely safe during pregnancy. It is essential to never stop taking this medication without your doctor's instruction.
- Dosage and Timing: Your pre-pregnancy dosage will almost certainly need to be increased, often by 25-50% immediately upon confirmation of pregnancy. This is due to the increased hormonal demand. Taking your pill consistently at the same time every day is critical for stable hormone levels.
- How to Take Your Medication for Best Absorption: Levothyroxine is best absorbed on a completely empty stomach. Take it first thing in the morning with a full glass of water and wait at least 30-60 minutes before eating or drinking anything else (especially coffee). Avoid taking it at the same time as prenatal vitamins, calcium, or iron supplements, as they can block absorption. Space them out by at least 4 hours.
Monitoring and Adjusting Your Treatment
Managing hypothyroidism in pregnancy is a dynamic process, not a "set it and forget it" prescription.
The Schedule for Blood Test Monitoring During Each Trimester
You will need your TSH levels checked frequently:
- At diagnosis and start of treatment.
- Every 4-6 weeks during the first half of pregnancy.
- At least once in the second half of pregnancy, and more often if your dose is adjusted.
- Finally, around 6 weeks postpartum to readjust to your pre-pregnancy dose.
How Your Medication Dosage Might Change?
Your doctor will adjust your Levothyroxine dose based on your TSH test results. It's common to have your dose increased several times throughout pregnancy as your blood volume expands and the baby's demands grow. Don't be alarmed by this; it's a sign your care team is being proactive.
Diet and Nutrition
While medication is the primary treatment, nutrition plays a vital supporting role.
The Iodine Imperative:
- Iodine is the fundamental building block of thyroid hormones. During pregnancy, your need for iodine increases by about 50%. Most of this should come from your prenatal vitamin (ensure it contains ~150 mcg of iodine) and a balanced diet including iodized salt, dairy products, and seafood. However, extremely high doses (e.g., from supplements beyond your prenatal) can be harmful, so always consult your doctor before adding any new supplement.
- Selenium and Other Supporting Nutrients
Selenium is a mineral that helps convert T4 into the active T3 hormone. Brazil nuts, tuna, and sardines are excellent sources. A balanced diet for hypothyroidism during pregnancy should also include adequate protein, zinc, and iron from whole foods like lean meats, legumes, and leafy greens. - Foods to Be Mindful Of (Goitrogens)
Cruciferous vegetables like broccoli, cauliflower, and cabbage contain substances called goitrogens that can interfere with thyroid function if consumed in extremely large, raw amounts. For nearly everyone, cooking these vegetables negates this effect, and they are far too nutritious to avoid. Enjoy them as part of a varied diet.
The Postpartum Period: What to Expect After Delivery
Once your baby is born, your thyroid hormone requirements will quickly return to your pre-pregnancy levels. Your doctor will likely reduce your Levothyroxine dose back to what it was before you conceived. It is critical to get your TSH checked around 6 weeks postpartum.
- Postpartum Thyroiditis:
This is an inflammation of the thyroid that affects up to 10% of women in the year after childbirth. It often follows a pattern: a hyperthyroid (overactive) phase first, causing anxiety, fatigue, and weight loss, followed by a hypothyroid phase. For most, thyroid function returns to normal within 12-18 months, but some women develop permanent hypothyroidism. If you experience strange mood swings, fatigue, or anxiety postpartum, ask your doctor to check your thyroid.
Planning a Future Pregnancy with a Thyroid Condition
If you have hypothyroidism and are planning another pregnancy, preconception counseling is key. The goal is to optimize your thyroid levels before you conceive. Ideally, your TSH should be below 2.5 mIU/L before pregnancy. As soon as you get a positive test, contact your doctor for an immediate TSH test and a likely medication dose adjustment.
Conclusion
Navigating a pregnancy with hypothyroidism may seem daunting at first, but it is a well-understood condition with a clear path to management. By committing to your medication regimen, attending all your monitoring appointments, and maintaining open communication with your healthcare providers, you are taking the most powerful steps to protect your health and your baby's development. Remember, you are not just managing a condition; you are actively nurturing a new life. This journey requires partnership and vigilance, but the outcome—a healthy mother and a healthy baby—is absolutely worth it. If you have any concerns about your symptoms or treatment plan, consult a doctor online with Apollo24|7 for expert guidance and reassurance throughout your pregnancy.
Consult Top Specialists
Consult Top Specialists

Dr. Pavithra Ramakrishnan
Obstetrician and Gynaecologist
10 Years • MBBS, MS (OG), Diploma in Aesthetic (Cosmetic) Gynaecology
Chennai
Apollo Speciality Hospitals OMR, Chennai
(50+ Patients)

Dr. Sravanthi Pandala
Obstetrician and Gynaecologist
9 Years • MBBS, MMS(OBG).,FMAS.,F.ART.,DRM(Germany).,
Nellore
Apollo Speciality Hospitals, Nellore
(100+ Patients)
Dr. Arpita Jain Garg
Obstetrician and Gynaecologist
3 Years • MBBS, DNB (Obstetrics & Gynaecology), PGDHHM
Ahmedabad
MH AHMEDABAD, Ahmedabad

Dr. K Laxmi Reddy
Obstetrician and Gynaecologist
24 Years • MBBS, DGO, DNB
Kokapet
VISLON HOSPITAL, Kokapet

Dr. Sheetal Aggarwal
Obstetrician and Gynaecologist
17 Years • MBBS, MS (Obstetrics & Gynaecology)
Gurugram
Dr Sheetal's clinic, Gurugram
Consult Top Specialists

Dr. Pavithra Ramakrishnan
Obstetrician and Gynaecologist
10 Years • MBBS, MS (OG), Diploma in Aesthetic (Cosmetic) Gynaecology
Chennai
Apollo Speciality Hospitals OMR, Chennai
(50+ Patients)

Dr. Sravanthi Pandala
Obstetrician and Gynaecologist
9 Years • MBBS, MMS(OBG).,FMAS.,F.ART.,DRM(Germany).,
Nellore
Apollo Speciality Hospitals, Nellore
(100+ Patients)
Dr. Arpita Jain Garg
Obstetrician and Gynaecologist
3 Years • MBBS, DNB (Obstetrics & Gynaecology), PGDHHM
Ahmedabad
MH AHMEDABAD, Ahmedabad

Dr. K Laxmi Reddy
Obstetrician and Gynaecologist
24 Years • MBBS, DGO, DNB
Kokapet
VISLON HOSPITAL, Kokapet

Dr. Sheetal Aggarwal
Obstetrician and Gynaecologist
17 Years • MBBS, MS (Obstetrics & Gynaecology)
Gurugram
Dr Sheetal's clinic, Gurugram
Frequently Asked Questions
Can hypothyroidism make it harder to get pregnant?
Yes, untreated hypothyroidism can disrupt your menstrual cycle and inhibit ovulation, leading to difficulties conceiving. Proper treatment to normalize thyroid levels often restores fertility.
Will I have to stay on thyroid medication forever?
If your hypothyroidism is due to a permanent cause like Hashimoto's or surgical removal, then yes, lifelong treatment is typically needed. However, your dosage will need to be adjusted after pregnancy and during other life stages.
Is it safe to breastfeed while taking Levothyroxine?
Absolutely. Levothyroxine is safe during breastfeeding. Only minimal amounts pass into breast milk, and it is not harmful to your baby. In fact, maintaining your treatment ensures you have the energy and health to care for your newborn.
Will my baby have hypothyroidism because I do?
It is possible but not guaranteed. Babies born to mothers with thyroid disease are at a slightly higher risk. This is why newborn screening, which includes a test for congenital hypothyroidism, is standard practice and can catch any issues early for immediate treatment.
What's the difference between hypothyroidism and postpartum thyroiditis?
Hypothyroidism is a chronic condition of an underactive thyroid. Postpartum thyroiditis is a temporary inflammation of the thyroid gland that occurs after childbirth. It often has a hyperthyroid phase first before swinging to hypothyroidism. While it often resolves, it can sometimes develop into permanent hypothyroidism.