Mucormycosis Symptoms and Treatment Options
Learn about Mucormycosis (Black Fungus), a rare but serious fungal infection. Discover its key symptoms, diagnosis, and the critical treatment options available.

Written by Dr. Shaik Abdul Kalam
Reviewed by Dr. Rohinipriyanka Pondugula MBBS
Last updated on 25th Aug, 2025
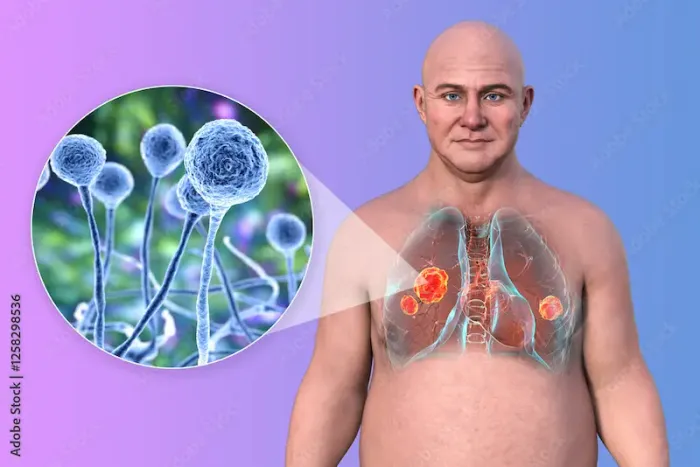
Mucormycosis, often referred to as "black fungus," is a rare but serious fungal infection that can affect people with weakened immune systems. While it is not contagious, it can be life-threatening if not treated promptly. Understanding its symptoms, causes, and treatment options can help you take the right steps if you or a loved one is at risk.
What Is Mucormycosis?
Mucormycosis is caused by a group of molds called mucormycetes, commonly found in soil, decaying organic matter, and even in the air. These fungi usually don’t harm healthy individuals, but they can cause severe infections in people with weakened immunity, uncontrolled diabetes, or those recovering from serious illnesses like COVID-19.
The infection primarily affects the sinuses, lungs, and brain, but it can also spread to other parts of the body, leading to tissue damage and even death if untreated.
Who Is at Risk?
Certain groups of people are more likely to develop mucormycosis, including:
• People with uncontrolled diabetes, especially those with high blood sugar levels.
• Cancer patients undergoing chemotherapy.
• Organ transplant recipients on immunosuppressive drugs.
• People with long-term steroid use, which weakens the immune system.
• Those recovering from severe COVID-19, particularly if they were on oxygen support or steroids.
Symptoms of Mucormycosis
The symptoms depend on which part of the body is infected. Here are the most common types and their signs:
1. Rhino-Orbital-Cerebral Mucormycosis (Sinus & Brain Infection)
• Nasal congestion or sinus pain
• Blackish discharge from the nose
• Facial swelling or numbness
• Blurred or double vision
• Toothache or loosening of teeth
• Headache and fever
2. Pulmonary Mucormycosis (Lung Infection)
• Cough (sometimes with blood)
• Shortness of breath
• Chest pain
• Fever
3. Gastrointestinal Mucormycosis (Stomach & Intestines)
• Abdominal pain
• Nausea and vomiting
• Blood in stools
4. Cutaneous Mucormycosis (Skin Infection)
• Blistering or ulcers on the skin
• Blackened skin tissue
• Pain and swelling
If you or someone you know experiences these symptoms—especially after recovering from COVID-19 or having uncontrolled diabetes—seek medical help immediately. Early diagnosis and treatment are crucial.
How Is Mucormycosis Diagnosed?
Doctors may use the following tests to confirm mucormycosis:
• Imaging tests (CT or MRI scans) to check for fungal invasion.
• Tissue biopsy to examine the infected area under a microscope.
• Blood tests to assess overall health and immune function.
Treatment Options for Mucormycosis
Since mucormycosis progresses rapidly, timely medical intervention is critical. Treatment usually involves:
1. Antifungal Medications
• Amphotericin B (the most common antifungal for mucormycosis).
• Posaconazole or Isavuconazole (alternative options).
These medications are given intravenously (IV) in severe cases.
2. Surgical Debridement
Doctors may remove infected or dead tissue to stop the spread of the fungus.
In severe cases, surgery may involve removing parts of the nose, jaw, or even the eye to save the patient’s life.
3. Controlling Underlying Conditions
• Managing diabetes by keeping blood sugar levels in check.
• Reducing steroid use (if possible) under medical supervision.
• Strengthening the immune system with proper nutrition and care.
How Can You Prevent Mucormycosis?
While not all cases can be prevented, you can reduce the risk by following these steps:
• Control Blood Sugar Levels – If you have diabetes, monitor and maintain healthy glucose levels.
• Use Steroids Wisely – Avoid unnecessary or excessive steroid use, especially during COVID-19 recovery.
• Maintain Hygiene – Wear masks in dusty areas, keep wounds clean, and avoid contaminated water.
• Boost Immunity – Eat a balanced diet rich in vitamins and minerals.
• Seek Early Medical Help – If you notice any unusual symptoms, consult a doctor without delay.
When to See a Doctor?
If you experience persistent sinus pain, black nasal discharge, vision problems, or skin lesions, especially after COVID-19 recovery or steroid treatment, seek emergency medical care.
At Apollo 24|7, you can book a consultation with specialists who can diagnose and treat mucormycosis effectively. Early detection can save lives!
Final Thoughts
Mucormycosis is a dangerous but manageable infection if caught early. By staying informed, maintaining good health practices, and seeking prompt medical attention, you can protect yourself and your loved ones.
If you suspect any symptoms, do not delay—consult a doctor today. Your health is precious, and timely action makes all the difference.
Book a consultation now on Apollo 24|7 for expert care. Stay safe, stay healthy!