The Urologist's Role in Male Infertility: A Complete Guide
Know about the role of urology in male infertility, what it is, the difference with reproductive endocrinologists, diagnosis, conditions treated, treatment options, lifestyle modifications and more.

Written by Dr. Md Yusuf Shareef
Reviewed by Dr. J T Hema Pratima MBBS, Fellowship in Diabetes Mellitus
Last updated on 13th Jan, 2026

Introduction
When a couple faces challenges conceiving, the journey often focuses initially on the female partner. However, male factors are a sole or contributing cause in about 50% of cases. This is where a urologist specialising in male infertility becomes a pivotal figure. This guide demystifies their crucial function, moving beyond the common misconception that they only deal with kidneys or prostates. We will explore how these specialists diagnose the complex causes behind low sperm count, poor motility, or other issues, and the array of treatments they offer, from medication and lifestyle advice to advanced microsurgical procedures.
What is a Male Fertility Urologist (Andrologist)?
A urologist is a physician specially trained in the health of the urinary tract and the male reproductive system. A male fertility urologist, often known as an andrologist, takes this a step further by focusing specifically on conditions affecting male reproduction, including infertility, low testosterone, erectile dysfunction, and ejaculatory disorders. They are the medical detectives and surgeons dedicated to identifying and fixing the biological issues that can prevent a man from fathering a child.
Consult a Urologist for Personalised Advice
Urologist vs. Reproductive Endocrinologist: Understanding the Difference
This is a common point of confusion. While both work towards the same goal—helping you build a family, their focus differs:
- A Reproductive Endocrinologist (RE) is an OB/GYN subspecialist who focuses on the female reproductive system. They are experts in ovulation induction, IVF, and embryo transfer. They often order the initial semen analysis but typically refer the male partner to a urologist for any abnormal findings.
- A Urologist/Andrologist is the specialist for the male partner. They diagnose the specific male condition, provide treatment to improve natural conception chances, or perform procedures to retrieve sperm for use with IVF/ICSI by the RE.
The Andrology Subspecialty: Advanced Male Reproductive Care
Andrology is the specific field of medicine dealing with male health. A urologist with a focus on andrology has advanced training in microsurgery, hormone management, and the interpretation of complex semen and genetic tests. This expertise is crucial for handling delicate procedures like vasectomy reversals or sperm retrievals, where precision is measured in millimetres.
When Should You See a Urologist for Infertility?
Knowing when to seek specialised help can save valuable time and emotional energy. The general rule of thumb is to seek an evaluation after one year of unprotected, well-timed intercourse without conception. However, you should see a urologist for male infertility sooner if you or your partner has any known risk factors or symptoms.
Key Indicators and Symptoms
Don't wait a full year if you experience:
- Problems with sexual function (e.g., erectile dysfunction, low libido)
- Pain, discomfort, or a lump in the testicular area
- A history of testicular trauma, surgery (especially hernia repair), or infection
- A known genetic condition, like cystic fibrosis or Klinefelter syndrome, in your family
- Issues with ejaculation, such as low volume or dry orgasms (which could indicate retrograde ejaculation)
After an Abnormal Semen Analysis Result
This is the most common pathway to a urologist. If an initial semen analysis reveals issues like low sperm count (oligospermia), poor sperm movement (asthenospermia), abnormal sperm shape (teratospermia), or the complete absence of sperm (azoospermia), a urologist is the next essential step to determine the "why" behind these results.
The Diagnostic Process: How a Urologist Finds the Root Cause
The urologist's approach is systematic and thorough, designed to leave no stone unturned.
The Initial Consultation: Medical History and Physical Exam
This is more than just paperwork. The urologist will ask detailed questions about your childhood development, past illnesses, surgeries, lifestyle habits (smoking, alcohol, heat exposure), and any medications you're taking. The physical exam is crucial; it assesses testicular size, consistency, and checks for the presence of a varicocele—a varicose vein in the scrotum that is a leading cause of infertility.
Semen Analysis: The Cornerstone of Male Fertility Testing
This test is so vital that it's often repeated for accuracy. It evaluates:
- Volume: The amount of fluid ejaculated.
- Count: The concentration of sperm per millilitre.
- Motility: The percentage of sperm that are moving.
- Morphology: The percentage of sperm that are normally shaped.
- An abnormal result guides the urologist toward the next appropriate tests.
Advanced Diagnostic Testing
Hormonal Blood Work: Measures testosterone, FSH, LH, and prolactin levels. Imbalances can signal a problem with the pituitary gland or testicular function.
- Scrotal Ultrasound: This painless test uses sound waves to create images of the testicles and surrounding structures. It's the gold standard for confirming a varicocele and ruling out other abnormalities like tumours.
- Genetic Testing: Recommended if sperm concentration is very low or absent. Tests like karyotype analysis or Y-chromosome microdeletion testing can identify genetic causes of infertility.
- Post-Ejaculatory Urinalysis: Used to diagnose retrograde ejaculation, where sperm travel backwards into the bladder instead of out through the penis.
Common Male Infertility Conditions a Urologist Treats
Varicocele: The Most Common Reversible Cause
A varicocele is an enlargement of veins within the scrotum, similar to varicose veins in the legs. It affects about 15% of all men but is found in about 40% of men with infertility. It can raise scrotal temperature, impairing sperm production and quality. Repairing a varicocele can often significantly improve semen analysis parameters.
Obstructive Azoospermia: Blockages in the Sperm Delivery System
In this condition, the testicles produce sperm normally, but a blockage (from prior infection, surgery, or a genetic condition like CBAVD) prevents them from being ejaculated. Treatment for obstructive azoospermia often involves microsurgical reconstruction to bypass the blockage or sperm retrieval for use with IVF/ICSI.
Non-Obstructive Azoospermia: Sperm Production Issues
This is a more challenging condition where the testicles produce very few or no sperm. Causes include genetic factors, hormonal imbalances, or prior chemotherapy. Even in severe cases, small pockets of sperm production may exist. A highly skilled urologist can perform a microTESE procedure to meticulously search for and extract these sperm for ICSI.
Treatment Options: From Medication to Microsurgery
The treatment plan is entirely personalised based on the diagnosis.
Medication and Hormonal Therapies
If a hormonal imbalance is identified, medications like Clomiphene Citrate can stimulate the body's own production of hormones to boost sperm production. Antibiotics are used to treat infections that may be impacting fertility.
Surgical Solutions for Male Infertility
- Varicocelectomy: This outpatient surgery ties off the abnormal veins, allowing blood to flow through healthier pathways. Studies show it can improve sperm count and motility in 60-70% of men, leading to natural pregnancy in many cases.
- Vasectomy Reversal: A microsurgical procedure to reconnect the vas deferens, allowing sperm to re-enter the ejaculate. Success depends on the time since the original vasectomy.
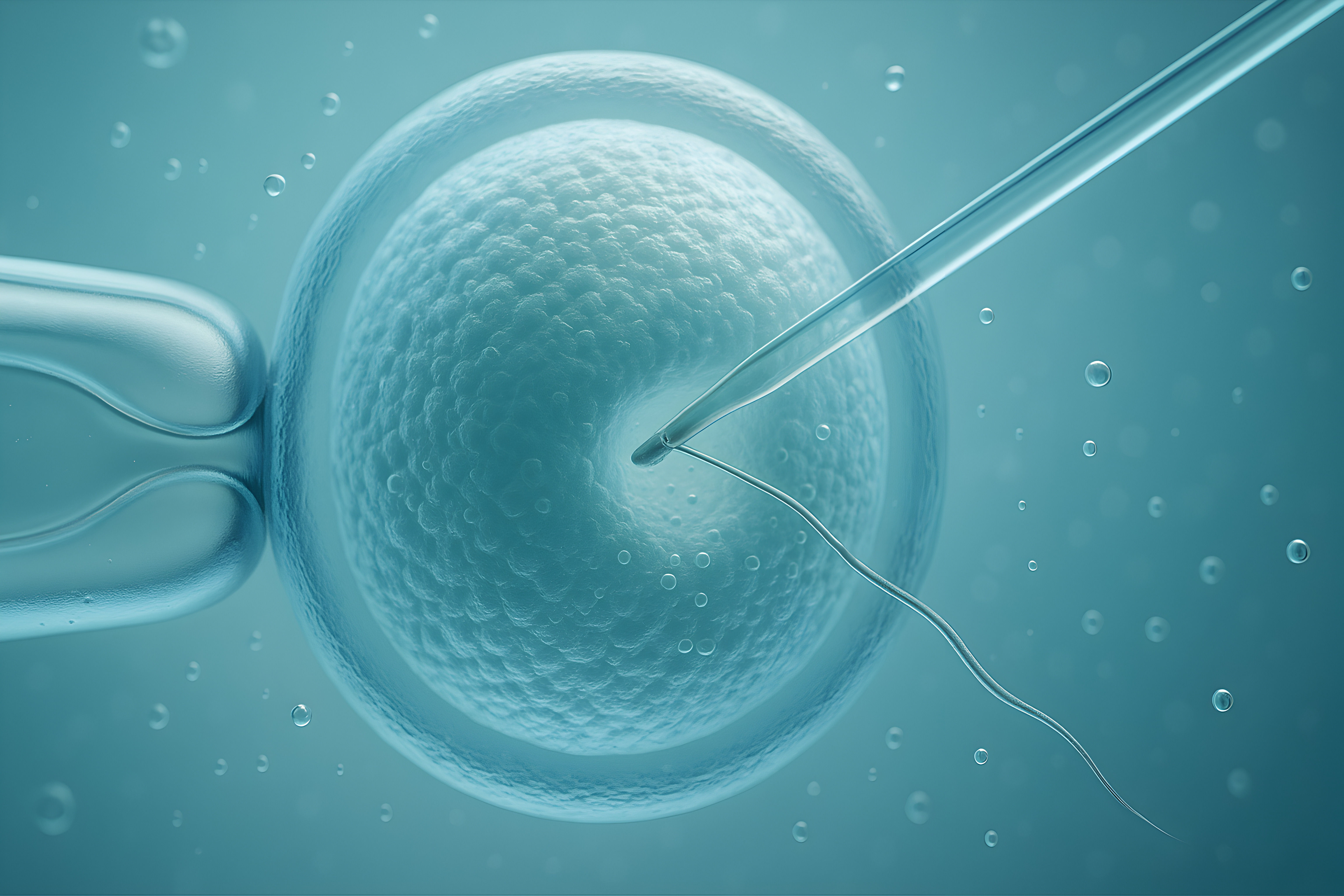
- Sperm Retrieval Techniques: For men with obstructions or low production, sperm can be retrieved directly from the testicle (TESA, TESE) or epididymis (PESA). The most advanced technique, microTESE, uses an operating microscope to identify and extract viable sperm from the testicular tissue with high precision, offering hope even for men with non-obstructive azoospermia.
The Urologist's Role in Assisted Reproductive Technology (ART)
The urologist is not working in a vacuum. They are a key member of the fertility team. After retrieving sperm, they work directly with the IVF lab to ensure the specimen is properly processed and prepared for Intracytoplasmic Sperm Injection (ICSI), where a single sperm is injected directly into an egg. They provide crucial counselling to couples on the realistic success rates of these advanced procedures.
Lifestyle Modifications and Their Impact on Fertility
A urologist will always discuss modifiable factors. This includes:
- Avoiding heat exposure (hot tubs, saunas, tight underwear)
- Quitting smoking and limiting alcohol
- Maintaining a healthy weight through diet and exercise
- Reducing stress
- Reviewing medications that might harm sperm production
- Often, these changes can make a significant difference in semen quality.
The Emotional Side of Male Infertility
An often-overlooked aspect of a urologist's role is addressing the psychological impact. Infertility can be a profound source of stress, anxiety, and feelings of inadequacy. A good urologist acknowledges this, provides empathetic counselling, and may recommend support groups or mental health professionals specialising in fertility issues. Open communication between partners is encouraged as a vital part of the healing and treatment process.
Conclusion
The journey through male infertility can feel isolating and complex, but you don't have to navigate it alone. Understanding the essential role of urologists provides a clear roadmap. They offer the expertise to accurately diagnose the root cause and provide a spectrum of effective treatments, from simple interventions to groundbreaking microsurgical techniques. If you and your partner are facing fertility challenges, taking the step to consult a specialist is powerful. A proactive evaluation can often identify treatable conditions, opening the door to new possibilities and hope.
Consult a Urologist for Personalised Advice
More articles from Infertility
Frequently Asked Questions
What is the success rate of varicocele surgery for improving fertility?
Success varies, but studies show that after a varicocelectomy, about 60-70% of men experience significant improvement in sperm count and motility. This leads to natural pregnancy for about 40-50% of couples within one to two years post-surgery, depending on female factors.
Can a urologist help if I have a low sperm count due to hormonal issues?
Absolutely. Hormonal imbalances are a common and often treatable cause of low sperm count. A urologist can prescribe medications like clomiphene or gonadotropins to stimulate your body's natural hormone production, which can effectively boost sperm production.
Is microTESE painful, and what is the recovery like?
MicroTESE is performed under anaesthesia, so you won't feel pain during the procedure. Post-operatively, it involves minor discomfort, swelling, and bruising for a week or two, manageable with pain medication. Most men can return to sedentary work within a few days but should avoid heavy lifting and strenuous activity for 2-4 weeks.
How much does male infertility treatment cost?
Costs vary widely based on the treatment. A diagnostic workup and medication may be a few thousand rupees, while surgeries like varicocelectomy or vasectomy reversal can cost more. Advanced sperm retrieval procedures (TESE, microTESE) and IVF/ICSI are the most expensive options. It's best to consult your doctor and insurance provider for specific details.
When should I consider seeing a urologist instead of just my primary care doctor?
You should see a urologist specifically if you have received an abnormal semen analysis result, have been trying to conceive for over a year, or have any specific symptoms like testicular pain, a lump, or ejaculatory problems. A urologist has the specialised training and tools for a definitive diagnosis and treatment.